Folie 1
advertisement
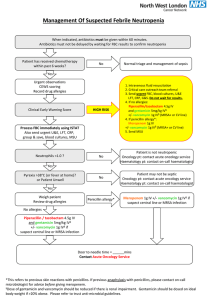
Antibiotikatherapie der Sepsis Tobias Welte Klinik für Pneumologie Medizinische Hochschule Hannover Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 Adequate vs inadequate antibiotic therapy Hospital mortality (%) p<0.001 p<0.001 88/169 71/169 114/486 52.1% 23.5% 42.0% 17.7% 86/486 Mortality type Hospital mortality and infection-related mortality rates for infected patients from all causes (n=655) receiving either initially inadequate or adequate antimicrobial treatment Prospective US cohort study evaluating 2000 consecutive patients Kollef et al. Chest 1999;115:462-74 Welte – Bremen 20.02.2014 Adequate versus inadequate initial antibiotic treatment and mortality p<0.001 Hospital mortality (%) 70 60 91/14 7 50 40 30 20 98/34 5 10 0 Adequate Inadequate Initial antimicrobial treatment Prospective US study in ICUs (492 bloodstream infections) ICU, intensive care unit Welte – Bremen 20.02.2014 Ibrahim et al. Chest 2000;118:146-55 Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 Changes in vancomycin MIC have been observed in the clinical setting • • TEST programme = international surveillance with standardised BMD methodology Looking for progression of vancomycin ‘creep’ into vancomycin resistance Phenotype Year Isolates S. aureus MRSA MSSA 2004-2009 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 20,004 797 (4.0) 8249 439 (5.3) 11,755 358 (3.0) 2004 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 2525 101 (4.0) 1158 65 (5.6) 1367 36 (2.6) 2005 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 2930 62 (2.1) 1411 39 (2.8) 1519 23 (1.5) 2006 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 3612 94 (2.6) 1531 50 (3.3) 2081 44 (2.1) 2007 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 4944 160 (3.2) 2028 78 (3.8) 2916 82 (2.8) 2008 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 4348 253 (5.8) 1481 136 (9.2) 2867 117 (4.1) 2009 All (n) Vancomycin MIC ≥2 µg/mL, n (%) 1645 127 (7.7) 640 71 (11.1) 1005 56 (5.6) p<0.001 Welte – Bremen 20.02.2014 Hawser et al. Int J Antimicrob Agents 2011;37:219-24 Vancomycin treatment failures increase with MIC 60 51 Failure rate (%) 50 40 30 22 20 31 27 10 0 0.0 0.5 1.0 1.5 2.0 MIC (μg/mL) Relationship between MIC and vancomycin treatment MIC, minimum inhibitory concentration Stevens. Clin Infect Dis 2006;42 Suppl 1:S51-7 Welte – Bremen 20.02.2014 Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 Importance of PK-PD parameters for optimal treatment of MRSA infection • For vancomycin and linezolid Antibiotic (C) – 24-hour AUC appears to be the most important PKPD parameter1,2 Peak AUC, area under the curve; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant S. aureus; PD, pharmacodynamic; PK, pharmacokinetic Welte – Bremen 20.02.2014 24-hour AUC MIC Time (h) 1. Andes et al. Antimicrob Agents Chemother 2002;46:3484-9; 2. Moise PA et al. Am J Health-Syst Pharm. 2000;57:S4-S9. Time to MRSA eradication with vancomycin Culture-positive patients (%) AUC/MIC<400 (n=16) AUC/MIC≥400 (n=18) 100 80 60 40 20 p=0.04 0 0 10 20 Days of therapy until bacterial eradication 30 AUIC, area under the inhibitory curve; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant S. aureus Moise-Broder et al. Clin Pharmacokinet 2004;43:925-42 Welte – Bremen 20.02.2014 Percent Probability of achieving AUIC/MIC ≥400 for vancomycin regimens of varying intensity when Cmin was between 15 and 20 mg/L MIC value (mg/L) AUIC, area under the inhibitory curve; Cmin, trough concentration; q12h, every 12 hours; MIC, minimum inhibitory concentration Welte – Bremen 20.02.2014 Patel et al. Clin Infect Dis 2011;52:969-74 Vancomycin: penetration in the lung tissue Vancomycin 6 hours post-injection ELF: mean 2.03 µg/ml (1-2.77 µg/ml)1 * Healthy volunteers 52%2 * Patients with pneumonia 9-18%1,3 No relationship between clinical outcomes and pharmacokinetics has been established * Data represent the drug level in ELF as a percentage of the simultaneous levels in plasma ELF, epithelial lining fluid Welte – Bremen 20.02.2014 1. Georges et al. Eur J Clin Microbiol Infect Dis 1997;16:385-8; 2. Rybak. Clin Infect Dis 2006;42 Suppl 1:S35-9; 3. Lamer et al. Antimicrob Agents Chemother 1993;37:281-6 Linezolid: high penetration in the lung tissue Linezolid 8 hours post-injection ELF: mean 31.4 µg/ml (8.3-89.2 µg/ml)1 *Healthy volunteers ~400%1 *Patients with pneumonia 105%2 No relationship between clinical outcomes and pharmacokinetics has been established * Data represent the drug level in ELF as a percentage of the simultaneous levels in plasma ELF, epithelial lining fluid Welte – Bremen 20.02.2014 1. Conte Jr et al. Antimicrob Agents Chemother 2002;46:1475-80; 2. Boselli et al. Crit Care Med 2005;33:1529-33; Linezolid: high bioavailability in ELF 16 critically ill VAP patients studied at steady state – – • • • • All with late-onset VAP 12 with organisms: 3 MRSA, 1 MSSA, 8 enteric Gram-negatives (4 enterobacteriaceae and 4 P. Aeruginosa) Serum and ELF concentrations after 2 days of therapy Blood at 10, 20, 30, 45 minutes and 1, 2, 4, 8, 12 hours after infusion BAL 1 and 12 hours after infusion Similar levels in serum and ELF – – Range of peak penetration: 34-188% Range of trough penetration: 28-220% Serum ELF 20 Linezolid concentration (mg/L) • 16 12 8 4 0 −1 0 2 4 6 Time (hours) 8 10 12 No relationship between clinical outcomes and pharmacokinetics has been established Mean steady-state plasma (red circles) and ELF (blue circles) concentrations with NP (n=16). The dotted line represents the susceptibility breakpoint (4 mg/L) of staphylococci for linezolid (1). Error bars represent standard deviations BAL, bronchoalveolar lavage; ELF, epithelial lining fluid; MRSA, methicillin-resistant S. aureus; MSSA, methicillin-sensitive S. aureus; VAP, ventilator-associated pneumonia Boselli et al. Crit Care Med 2005;33:1529-33 Welte – Bremen 20.02.2014 Continuous vs intermittent infusion vancomycin • • • Prospective randomised study Designed to compare continuous vs intermittent vancomycin in 119 critically ill patients with MRSA infections Microbiological and clinical outcomes and safety were similar No statistically significant difference was found between the two treatment groups 60 Intermittent infusion (n=58) Continuous infusion (n=61) 50 Patients (%) • 40 30 20 10 n=30 n=28 n=15 n=13 n=7 n=5 0 No pathogen (day 5) Treatment failure (day 10) Infection-related deaths (day 10) Adapted from Wysocki et al. Antimicrob Agents Chemother 2001;45:2460-7 Welte – Bremen 20.02.2014 Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 Nephrotoxicity (%) Renal effects related to vancomycin concentration p=0.002 70 60 50 40 30 20 10 0 Renal toxicity was defined as increased creatinine by 0.5 mg/dL or doubling of baseline value <15 15-20 >20 Maximum vancomycin steady-state trough concentrations (mg/mL)a Aggressive dosing and prolonged administration of vancomycin are associated with a greater risk of nephrotoxicity in patients with MRSA HCAP aMaximum vancomycin serum trough concentrations ≥15 µg/mL (n=49); maximum vancomycin serum trough concentrations <15 µg/mL (n=45) Retrospective US observational single-centre study HCAP, healthcare-associated pneumonia; MRSA, methicillin-resistant S. aureus Adapted from Jeffres et al. Clin Ther 2007;29:1107-15 Welte – Bremen 20.02.2014 Vancomycin relationships: toxicity and target attainment AUC/MIC ratio ≥400 MIC value Nephrotoxic event 0.5 mg/L (%) 1.0 mg/L (%) 2.0 mg/L (%) Non-ICU (%) ICU (%) 500 mg IV q12h 57 15 0.7 3 10 1000 mg IV q12h 90 57 15 6 16 1500 mg IV q12h 97 79 38 9 25 2000 mg IV q12h 98 90 57 14 34 AUC, area under the curve; ICU, intensive care unit; MIC, minimum inhibitory concentration Patel et al. Clin Infect Dis 2011;52:969-74 Welte – Bremen 20.02.2014 Vancomycin concentration-time profile Lodise et al. Clin Infect Dis 2009;49:507-14 • • Retrospective US study correlating the vancomycin nephrotoxicity with its pharmacokinetics in 166 non-neutropenic patients – Baseline creatinine <2.0 mg/dL – Vancomycin >48 h 21 patients with nephrotoxicty (50% or 0.5 mg/dL increase in the serum creatinine level from baseline) The results indicate that a vancomycin exposure–toxicity response relationship exists. The vancomycin trough value is the pharmacodynamic index that best describes this association Logistic regression-derived nephrotoxicity probability functions ICU patients ICU patients Probability of Nephrotoxicity • Non-ICU patients Non-ICU patients 1.00 0.80 0.60 0.40 0.20 0.00 0 5 10 15 20 25 Initial Vancomycin Trough Value, mg/L ICU, intensive care unit Welte – Bremen 20.02.2014 30 Outline • Consequences of inappropriate MRSA NP therapy • Appropriate MRSA NP therapy – Vancomycin MIC creep – PK of vancomycin and linezolid – Nephrotoxicity of vancomycin • ZEPHyR study and results • Conclusions MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 ZEPHyR study: design overview and objective Design overview • Phase IV, randomised, double-blind, multicentre, international comparator-controlled study in MRSA VAP, HAP or HCAP – Fixed-dose linezolid vs dose-optimised vancomycin – Non-inferiority study with a nested superiority hypothesis Study objective • To prospectively assess the efficacy, safety and tolerability of linezolid compared with vancomycin in MRSA nosocomial pneumonia HAP, hospital-acquired pneumonia; HCAP, healthcare-associated pneumonia; MRSA, methicillin-resistant S. aureus; VAP, ventilator-associated pneumonia Welte – Bremen 20.02.2014 Wunderink et al. Clin Infect Dis 2012;54:621-9 ZEPHyR study: randomisation and interventions Linezolid IV 600 mg q12h 1:1 randomisation 7-14 days EOT visit EOS visit Within 5 days 7-30 days after EOT of EOT Follow-up call: survival status at day 60 Vancomycin IV 15 mg/kg q12h Vancomycin dose adjusted by unblinded pharmacist per local protocols based on trough levels and renal impairment Gram-negative coverage (not MRSA active) EOT, end of treatment; EOS, end of study; MRSA, methicillin-resistant S. aureus Welte – Bremen 20.02.2014 Wunderink et al. Clin Infect Dis 2012;54:621-9 Patients with clinical response (%) Statistically superior clinical efficacy of linezolid vs vancomycin in MRSA NP in the ZEPHyR study p=0.042 95% CI 0.5-21.6 95% CI 4.9-22.0 95% CI 0.1-19.8 150/180 161/201 130/186 95/165 95% CI 4.0-20.7 145/214 102/186 81/174 Primary end point 92/205 Secondary end points Patients with EOS outcome of ‘indeterminate’ were excluded from the efficacy analysis CI, confidence interval; EOS, end of study; EOT, end of treatment; mITT, modified intent-to-treat; MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia; PP, per protocol Wunderink et al. Clin Infect Dis 2012;54:621-9 Welte – Bremen 20.02.2014 Statistically-significant higher rates of microbiological success with linezolid vs vancomycin in the ZEPHyR study PP population Patients with respiratory secretions for culture Patients with microbiological response (%) 95% CI 12.3-30.2 95% CI 0.4-21.5 58.1% (97/167) 47.1% (82/174) 63.9% (62/97) 68.3% (56/82) 36.1% (35/97) 31.7% (26/82) 82.6% (76/92) 81.9% (149/182) 49.0% (73/149) 60.6% (114/188) 61.4% (35/57) 50.0% (26/52) 54.1% (59/109) 48.2% (55/114) 51.0% (76/149) 51.8% (59/114) Linezolid Vancomycin Linezolid Vancomycin Linezolid Vancomycin Linezolid Vancomycin EOS EOT CI, confidence interval; EOS, end of study; EOT, end of treatment; PP, per protocol Welte – Bremen 20.02.2014 EOS EOT Wunderink et al. Clin Infect Dis 2012;54:621-9 Response differences between linezolid and vancomycin remained across most subgroups in the ZEPHyR study Clinical success rate1 (%) 100 Linezolid Vancomycin 80 60 57.6 46.6 40 62.5 58.8 55.5 44.2 50.0 44.4 55.6 48.6 40.8 61.5 50.0 43.1 47.8 51.7 43.1 31.6 20 0 APACHE, Acute Physiological Assessment and Chronic Health Evaluation; EOS, end of study; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant S. aureus; MV, mechanical ventilation Welte – Bremen 20.02.2014 Wunderink et al. Clin Infect Dis 2012;54:621-9 No relationship between vancomycin trough level and Clinical Microbiological outcomes in the ZEPHyR study Clinical success Clinical failure 20 17.8 16.0 14.4 14.8 15 12.2 12.6 10 5 73 0 Range: 82 3.4-50.8 2.8-43.2 47 52 5.1-45.0 2.7-41.4 23 Median vancomycin trough concentration (µg/mL) Median vancomycin trough concentration (µg/mL) 25 15 2.0-42.6 4.1-46.9 76 Range: 80 2.8-50.8 3.3-43.2 50 49 5.1-45.0 2.7-36.4 22 16 2.9-42.6 3.0-46.9 Vancomycin Vancomycin Vancomycin Day 3 Day 6 Day 9 End of study End of study Adapted from Niederman et al. Am J Respir Crit Care Med 2011;183:A3932 Welte – Bremen 20.02.2014 Nephrotoxicity was nearly twice as common in vancomycin patients in the ZEPHyR study (mITT population) Patients with nephrotoxicity (%) Laboratory evidence of nephrotoxicity (0.5 mg/mL increase in serum creatinine if normal at baseline, or 50% increase if abnormal at baseline) GFR, glomerular filtration rate Adapted from Wunderink et al. Clin Infect Dis 2012;54:621-9 Welte – Bremen 20.02.2014 Linezolid has a comparable tolerability profile with vancomycin in the ZEPHyR studyLinezolid Vancomycin AE, n (%) (n=597) (n=587) Anaemia 30 (5.2) 42 (7.2) Renal failure/impairment/azotaemiaa 22 (3.7) 43 (7.3) Cardiac arrest 11 (1.8) 13 (2.2) Thrombocytopenia 8 (1.3) 13 (2.2) Pancreatitis 5 (0.8) 1 (0.2) — 1 (0.2) 4 (0.6) 2 (0.4) — 1 (0.2) Polyneuropathy Pancytopenia/neutropenia Paresthesia aPatient was reported to have ≥1 of the following: renal failure, renal impairment and/or azotaemia AE, adverse event Wunderink et al. Clin Infect Dis 2012;54:621-9 Welte – Bremen 20.02.2014 Similar 60-day mortality with linezolid and vancomycin: the ZEPHyR study Comparable all-cause 60-day mortality rates1 – Linezolid arm 15.7%; vancomycin arm 17.0% (ITT population) – Linezolid arm 28.1%; vancomycin arm 26.3% (mITT population) No pneumonia trial has ever demonstrated an overall mortality difference between antibiotics2 1. Wunderink et al. Clin Infect Dis 2012;54:621-9; 2. Wunderink et al. Clin Infect Dis 2012;55:163-5 [letter] Patients surviving (%) 100 Kaplan–Meier survival curves for the mITT population 80 60 40 Linezolid Linezolid censored 20 Vancomycin Vancomycin censored 0 0 ITT, intent-to-treat; mITT, modified intent-to-treat Welte – Bremen 20.02.2014 10 20 30 40 50 60 70 Time (days) 80 90 100 110 120 Conclusions • MRSA NP remains an important healthcare burden • Linezolid demonstrated statistically superior clinical efficacy versus vancomycin in the treatment of MRSA NP in the ZEPHyR study1 • Overall, linezolid demonstrated an acceptable safety and tolerability profile for the treatment of proven MRSA nosocomial pneumonia1 • Linezolid was associated with lower rates of pneumonia-related rehospitalisation versus vancomycin in a US retrospective study 2 MRSA, methicillin-resistant S. aureus; NP, nosocomial pneumonia Welte – Bremen 20.02.2014 1 .Wunderink et al. Clin Infect Dis 2012;54:621-9 2. Mullins et al. Poster PIN56 presented at ISPOR 2012 Welte – Bremen 20.02.2014