File
advertisement
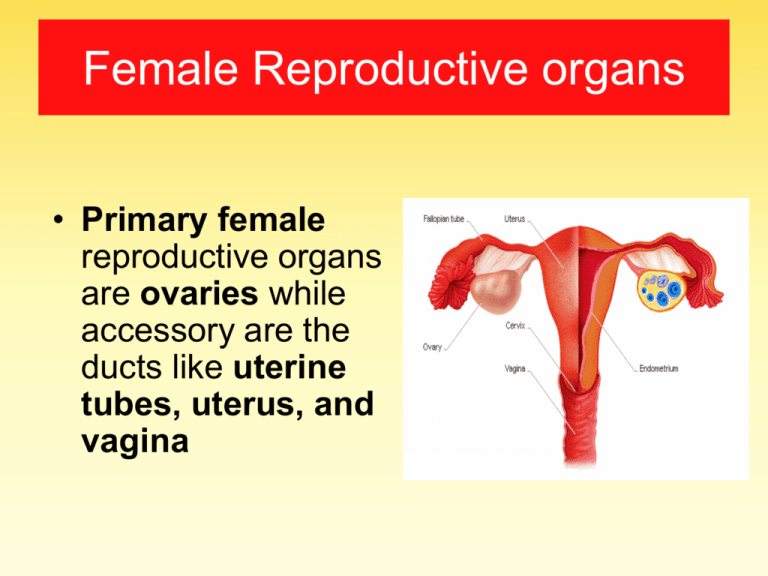
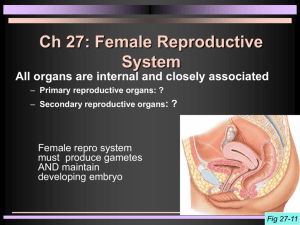
Female Reproductive organs • Primary female reproductive organs are ovaries while accessory are the ducts like uterine tubes, uterus, and vagina The Ovaries The Ovaries • The ovaries on the outer side are surrounded by a layer of epithelial cells called the germinal epithelium. • Embedded in their cortex are ovarian follicles in various stages of development. • The remains of ruptured follicle after ovulation is called corpus luteum Uterine Tubes • Uterine tubes receive the ovulated oocyte and provide a site for fertilization. They empty into the uterus. • They expand distally around the ovary forming the ampulla which ends in the funnel-shaped, ciliated infundibulum containing fingerlike projections called fimbriae. Uterine Tubes • The uterine tubes have no contact with the ovaries and the ovulated oocyte is cast into the peritoneal cavity. Beating cilia on the fimbriae create currents to carry the oocyte into the uterine tube. • The oocyte is carried toward the uterus by peristalsis and ciliary action of the lining ciliary epithelium of the tube. Uterus • The uterus is a hollow, thick-walled organ located in the pelvis anterior to the rectum and posterio superior to the urinary bladder. Its parts are • Fundus – rounded region superior to the entrance of the uterine tubes • Body – major portion of the uterus • Isthmus – narrowed region between the body and cervix Uterus • Cervix – narrow neck which projects into the vagina inferiorly • Cervical canal – cavity of the cervix that communicates with: – The vagina via the external os – The uterine body via the internal os • Cervical glands secrete mucus that covers the external os and blocks sperm entry except during midcycle Uterine Wall Stratum functionalis Stratum basale Endometrium Composed of three layers • Perimetrium – outermost serous layer; the visceral peritoneum • Myometrium – middle layer; consists of interlacing layers of smooth muscles • Endometrium – mucosal lining of the uterine cavity. It has numerous uterine glands and consists of – Stratum functionalis: It undergoes cyclic changes in response to ovarian hormones and is shed during menstruation – Stratum basalis: It forms a new functionalis layer after menstruation ends. It does not respond to ovarian hormones. Ovarian Cycle • Monthly series of events occurring in ovaries associated with the maturation of an egg is called an ovarian cycle. It consists of follicular phase and luteal phase • Follicular phase – period of follicle growth (days 1–14). During it primordial follicle becomes primary, secondary and tertiary follicles and follicular cells become granulosa cells secreting estrogen. Ovarian Cycle Follicular phase cont. The full sized follicle (vesicular follicle) bulges from the external surface of the ovary. The primary oocyte completes meiosis I, and the stage is set for ovulation. Ovulation occurs at the mid of the cycle and a twinge of pain is sometimes felt in pelvis at ovulation called Mittelschmerz Ovarian Cycle Luteal phase – A period of corpus luteum activity (days 14– 28). After ovulation, the ruptured follicle collapses, granulosa cells enlarge, and along with internal thecal cells, form the corpus luteum The corpus luteum secretes progesterone and estrogen.. Ovarian Cycle Luteal phase cont. If pregnancy does not occur, the corpus luteum degenerates in 10 days, leaving a scar (corpus albicans) in the ovary. If pregnancy occurs, the corpus luteum produces hormones until the placenta takes over that role (at about 3 months of gestation) MENSTRUAL CYCLE What actually happens in those 28 days? The ovarian and menstrual cycle of the human female Uterine (Endometrial) Cycle • Monthly cyclical changes in the endometrium of uterus for prepration of implantation (in the event of fertilization) and for menstruation (in the absence of fertilization) is called uterine cycle. • The uterine endometrial cycle can be divided into three phases: – the proliferative phase, – the secretary, – the menstrual phase. Uterine (Endometrial) Cycle • Proliferative Phase • The proliferative or follicular, phase, spans from the end of the menstruation until ovulation. • Under the influence of increasing levels of estrogen secreted by ovarian follicles all elements of endometrium proliferate. • The raw surface of endometrium is again covered with epithelium which proliferates out from the remains of the stems of uterine glands. The stromal cells increase Uterine (Endometrial) Cycle Proliferative Phase cont. • Endometrial glands elongate with cells containing some glycogen. But it is not secreted during the follicular phase. • Spiral arteries supplying blood also elongate. Stratum functionalis thus resumed again. Uterine (Endometrial) Cycle Secretary Phase • The luteal, or secretory phase, begins at ovulation and lasts until the menstrual phase of the next cycle. • At the beginning of the luteal phase, progesterone induces the endometrial glands to secrete glycogen, mucus, and other substances. These glands become tortuous and have large lumens due to increased secretary activity. Uterine (Endometrial) Cycle Secretary Phase cont. • The spiral arteries extend into the superficial layer of the endometrium. • In the absence of fertilization by day 23 of the cycle, the corpus luteum begins to degenerate and consequently ovarian hormone levels decrease. Uterine (Endometrial Cycle) Secretary Phase cont. • As estrogen and progesterone levels decrease, the endometrium undergoes involution. • Days 25-26 of the menstrual cycle, endothelin and thromboxin begin to mediate vasoconstriction of the spiral arteries. The resulting ischemia may cause some early menstrual cramps. Uterine (Endometrial Cycle) Secretary Phase cont. • By day 28 of the menstrual cycle, intense vasoconstriction and subsequent ischemia cause mass apoptosis of the stratum functionalis. Uterine (Endometrial) Cycle Menstrual Phase • The menstrual phase begins as the spiral arteries rupture secondary to ischemia, releasing blood into the uterus, and the apoptosed endometrium is sloughed off. It usually lasts four days. During this period, the stratum functionalis is completely shed. • Arterial and venous blood, remnants of endometrial stroma and glands, leukocytes, and red blood cells are all present in the menstrual flow. Hormonal control 1. 2. 3. Pituitary gland release Follicle Stimulating Hormone (FSH) that acts on the ovary. Ovarian follicles grow and mature under influence of FSH, and produce increasing quantities of estrogen When levels of estrogen reach a threshold level, a feed back process decreases the production of FSH by the pituitary. Hormonal control 4. 5. 6. Increased estrogen levels trigger the release of Luteinizing Hormone (LH) from the pituitary gland Ovulation occurs, that is release of an egg from the follicle. The empty follicle forms the corpus luteum, which produces progesterone which maintains the endometrium in a state of readiness to receive a fertilized egg Hormonal control 7. If the fertilized egg does not implant itself the progesterone level falls and mensturation commences. Summary of Reproductive Hormones in Females • Hypothalamus releases Gonadotropin Releasing Hormone (GRH) which binds with receptors in Ant. Pituitary • Anterior Pituitary releases Follicle Stimulating Hormone (FSH) and Luteinizing Hormone(LH) pass in blood to site of action • FSH acts on receptors in ovaries to stimulate development of the egg follicles • LH causes rupture of egg follicles. • Rupture of egg triggers production of estrogens and progestogens from remaining tissues of follicle,corpus luteum • These hormones travel in blood to the brain • Hypothalamus senses levels, then may decrease release of GRH At end of this study you are able to • Describe structure of ovary, uterine tubes and uterus • Discuss the cyclic changes in the female genital tract, which include: – The ovarian cycle (phases and hormonal control). – The uterine cycle (phases and hormonal control)