Female Hormonal Cycle - also known as the MENSTRUAL CYCLE

Female Hormonal Cycle
MENSTRUAL CYCLE by : S. Rouholamin MD
Reproductive hormones: GnRH
GnRH: decapeptide, by neurons in arcuate nucleus of hypothalamus
Regulate secretion of two hormones: FSH and LH
Pulsatile secretion
Extremely short half-life: only 2-4 min
Gonodotropins
LH &FSH: by ant pituitary gonadotroph cells
Ovarian follicular stimulation
Glycoproteins, alpha &beta subunit
Prolactin
Poly peptide, by ant pituitary lactotroph
Primary trophic factor responsible for the synthesis of milk by breast
PRL secretion is under tonic inhibitory control by hypothalamic secretion of dopamine
PRL stimulation: breast manipulation, drugs, stress, exercise, certain foods
TSH
By ant pituitary thyrotrophs in response to TRH
TRH:by arcuate nucleus ,portal circulation, pituitary
TRH: TSH & PRL release
Hypo- and hyperthyroidism: ovulatory dysfunction
Oxytocin
9 aa peptide, by paraventricular nucleus of hypothalamus
Uterine muscular contraction, breast lactiferous duct myoepithelial contraction
MENSTRUAL CYCLE
Normal cycle length is considered 28 days
varies from female to female (21-35 days)
Ovarian cycle: 1-follicular ,2-luteal
Uterine cycle: 1-proliferative ,2-secreatory
1 – Follicular phase
Development dominant follicle, mature at midcycle, ovulation
Average length:10-14 days
Variability in length: variations in total cycle length
2-luteal phase
Ovulation to menses
Average length: 14 days
Normal menstrual cycle
21-35 days
2-6 days of flow
Average blood loss:20-60 ml
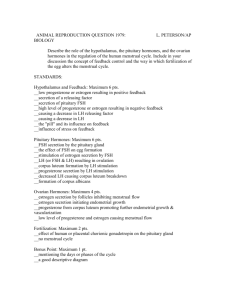
Hormonal variations
1.
At the beginning of cycle: levels of gonadal steroids are low
2.
Demise of corpus luteum, FSH levels rise, cohort of growing follicles is recruited, rise in estrogen: stimulus for uterine endometrial proliferation
Hormonal variations
3.
Rising estrogen levels: negative feedback on pituitary FSH secretion; growing follicle produce inhibin-B: suppresses pituitary FSH secretion;
Rising estrogen levels: LH initially decreases but late in follicular phase LH levels increased dramatically
Hormonal variations
4.
At the end of follicular phase (just before ovulation) FSH-induced LH receptors on granulosa cells; with LH stimulation, modulate secretion of progesterone
Hormonal variations
5.
After sufficient degree of estrogenic stimulation; pituitary LH surge triggered, proximate cause of ovulation occurs 24 to 36 hours later
Hormonal variations
6.
Estrogen level decreases through the early luteal phase from just before ovulation until midluteal phase, rise again as a result of corpus luteum secretion
Hormonal variations
7.
Progesteron levels rise after ovulation; presumptive sign of ovulation
8.
Progesteron;estrogen and inhibin-A : suppress gonadotropin secretion and new follicular growth
Cyclic changes of the
Endometrium
Decidua functionalis: 2/3 superficial, proliferate and shed each cycle
Decidua basalis: deepest region, source of endometrial regeneration after each menses
1-Proliferative phase
First day of vaginal bleeding :day 1 of the menstrual cycle
Progressive mitotic growth of decidua functionalis, preparation for implantation of embryo
Thin endometrium (1-2 mm); straight, narrow, short endometrial glands become longer, tortuous structures
2-Secretory phase
48 to 72 hours following ovulation, progesteron secretion: eosinophilic protein-rich secretory product in glandular lumen
Postovulatory day 6-7,maximal secretory activity: optimal for implantation of blastocyst
Stromal edema in late secretory phase
2-Secretory phase
2 days before menses:dramatic increases in PMN migrate from vascular system
Menses
Absence of implantations, glandular secretion ceases, irregular break-down of decidua fuctionalis
Destruction of corpus luteum and its productions estrogen and progesteron: cause of shedding
Withdrawal of sex steroids: spiral art spasm, endometrial ischemia, lysosoms breakdown, proteolytic enzymes release
Ovarian follicular development
Fetus:6-7 million in 20 wks
At birth:1-2 million
At puberty:300,000
Release during ovulation:400-500
At menopause:rare
Oogonia: only one final daughter cell (oocyte), three polar body
Oocyte arrested in prophase
(diploten) until time of ovulation
Two-cell two-gonadotropin theory
with LH stimulation, the ovarian theca cells produce androgens that convert by granulosa cells into estrogens under the stimulus of FSH