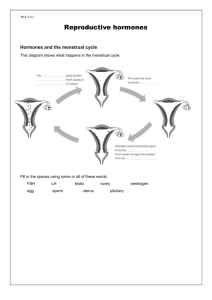
Physiologic & menstruation
advertisement
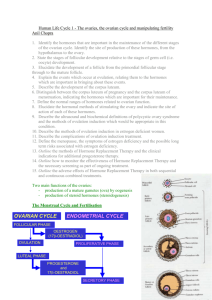
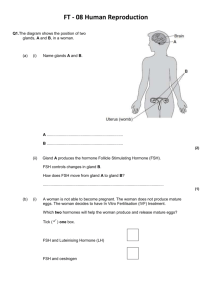
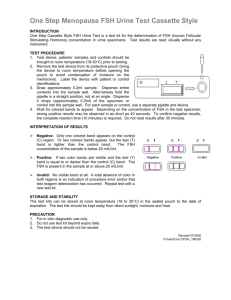
Physiology of menstruation Dr: Abir Mohidien Said 2012 The normal menstrual cycle Menstruation describes the female period, involves the monthly release of an egg(ovum) in a process called ovulation, with bleeding due to shedding of the uterine lining following failure of fertilization of the oocyte or failure of implantation. The cycle has an average duration of 28 days, but the normal range is bet.21-35 days. The normal menstrual cycle Menstruation usually starts at an average age of 13( called menarche) and lasts on average till age 51 (called menopause). Normal menstruation is a highly complex interactions between a number of hormones produced by 3 organs of the body: Hypothalamus Pituitary gland Ovary The interactions between these organs are referred to as the hypothalamic-pituitary-ovarian axis(HPO axis) Hypothalamus The hypothalamus in the forebrain secretes GnRH which controls of 2 important pituitary hormone secretion FSH (follicular stimulating hormone)& LH ( luteinising hormone) GnRH is of great importance in the menstrual cycle, its release occurs in a pulsatile fashion to stimulate LH & FSH, anything that interferes with the pulse frequency of GnRH can stop the menstrual cycle from occurring If GnRH is given in a constant high dose, it desensitizes the GnRH receptor & reduces LH & FSH release Pituitary gland Anterior pit.gland causes synthesis & release of gonadotrophic hormones FSH & LH by stimulation of GnRH. This process is influence and stimulate the ovarian sex steroid hormones: oestrogen & progesterone. Negative feedback (low level of oestrogen will ↓LH production) Positive feedback (high level of oestrogen will ↑ LH production) Pituitary gland GnRH agonists when administered continuously they will down regulate the pituitary and ↓ LH & FSH secretion, this has effects on ovarian function and oestrogen and progestron levels also fall and most women become amenorrhoeic, these drugs are used as treatment for endometriosis and to shrink fibroid prior to surgery. Pituitary gland As the dominant follicle grows further oestrogen level ↑ until it is sufficient to exert a positive feed back effect on the pituitary LH secretion which is ↑ more rapidly from day 12 onward called the LH surge. Combined oral contraceptive pill creates artificially a constant serum oestrogen level in the negative feedback , inducing low level of gonadotophin hormone release. Unlike oestrogen, low level of progesterone have a positive feedback effect on pituitary LH & FSH. Ovary Females are born with 2-4 mil.primary follicles. These containing oocytes will activate and grow in a cyclical fashion, causing ovulation and menstruation in the onset of menarche. No new oocytes are formed during the female lifetime. Normal menstruation cycle in the ovary will go through three phases: follicular phase ovulation luteal phase Follicular phase Within the follicles , there are two cell types: theca and granulosa cells which respond to LH and FSH stimulation and produce oestrogen, progestrone , inhibin and activin. Both FSH & LH are required to generate a normal cycle with adequate amounts of oestrogen. As the follicles grow & oestrogen secretion ↑, there is negative feedback on the pituitary to ↓ FSH secretion. this select one follicle to continue in its development towards ovulation ( the dominant follicle) Follicular phase While smaller follicles will undergo atresia. Exogenous gonadotrophins is likely to stimulate growth of multiple follicles which continue to develop, risk of multiple gestations about 30%. Inhibin is secreted by granulosa cells within the ovaries & it participated in feedback to the pituitary to down regulate FSH. Activin is structurally similar to inhibin but has an opposite action, acts to ↑FSH binding on the follicles. Ovulation The dominant follicle grow to 18-22 mm at average of 14 days, oestrogen ↑until exert a positive feedback effort on the hypothalamus & pituitary to cause the LH surge. This occurs over 24-36 hours, LH induced dominant follicle to produce progestrone & causing a small per ovulatory rise in FSH. Androgens synthesized in the theca cells ↑at time of ovulation to stimulat libido & sexual activity. Luteal phase After the release of the oocyte, the remaining granulosa and theca cells on the ovary form the corpus luteum ( yellow body), its extensive vascularization to supply granulosa cells with a rich blood supply for continued steroidogenesis. Highest level of progesterone in luteal phase to prepares endometrium for pregnancy & has the effect of suppressing FSH & LH secretion to a level that will not produce further follicular growth in the ovary during that cycle. Luteal phase In the absence of beta human chorionic gonadotrophin βHCG which producers from an implantning embryo, the corpus luteum will regres & disappear from ovary ( luteolysis). The withdrawal of progesterone causing shedding of the endometrium & menstruation. ↓ in levels of progesterone, oestrogen & inhibin feedingback to pituitary cause ↑gonadotrophic hormones, particulary FSH & new preantral follicles begin to be stimulated & begins a new cycle Menstruation In reproductive age its under the influence of sex hormones. exposur to oestrogen & progest, will results proliferative & secretory phase. Menstruation day 1 is the shedding of the dead endometrium( uppermost layer) and day 5-6 of cycle regenerates again. Approximatly 14 days after ovulation ↓in circulating levels of oestrogen and progestrone leads to loss of tissue fluid, vasoconstriction of spiral arterioles and distal ischaemia and this leads to loss of the upper layer along with bleeding. Menstruation Contraceptive pill or hormone replacement therapy produces artificially withdrawal bleeding. Prostaglandines are produced by the endometrium and are vasoconstrictors. Non-steroidal anti-inflammatory agents used for treatment of heavy and painful periods. Mefenamic acid is a prostaglandin synthetase inhibitor used as a treatment for heavy menstrual bleeding ( reduces blood loss by 2025%) The proliferative phase After menstruation enters the proliferative phase, when glandular and stromal growth occur, the epithelium changes from single layer of columnar cells to a pseudostratified epithelium with frequent mitosis, thickness ↑ rapidly. The secretory phase After ovulation and progestrone surge( generally around day 14), cellular proliferation is inhibited and endometrial thickness does not increase any further, the endomerial glands will become more tortuous, spiral arteries will grow and fluid is secreted into glandular cells and uterin lumen. On the withdrawal of both oestrogen and progesterone, the decidua will collapse with vasoconstriction and relaxation of spiral arteries and shedding of the outer layers of the endometrium . Proliferative phase secretory phase Measurement of ovarian reserve Menstruation remaining depends of number oocytes. Deficit of gonadotrophin or exposure to toxins accelerate menopause age. U/S to measure of ovarian volume, diameter and antral follicle count to calculate ovarian reserve. Biochemical markers: FSH, oestradiol, inhibin B, anti-Mullerian hormone AMH( is produced in the granulosa cells and not change in response to gonadotrophins during the cycle)