Running head: UNCERTAINTY
Uncertainty
Autumn Burns
Auburn University/Auburn Montgomery
UNCERTAINTY
2
Abstract
Walker and Avant’s eight steps for concept analysis are utilized in this paper to obtain the
defining attributes of uncertainty. Uncertainty affects many different domains, and more
specifically nursing and psychiatry. Three case illustrations, a model case, a borderline case, and
a related case, are discussed and demonstrate the relationship between the defining attributes and
uncertainty. Implications for nursing practice are educating the patient, spending time with the
patient, answering questions the patient might have, and being an advocate for the patient.
Understanding the concept of uncertainty and how it affects patients and their families while also
adopting suggested interventions could decrease overall uncertainty and increase positive patient
outcomes.
UNCERTAINTY
3
Uncertainty
Uncertainty is simply defined as an incapability to allocate definite values and/or
ascertain an exact conclusion for an event. It applies to not only to future events, but those
previously determined, and of the unknown. Different areas in which uncertainty may be
discussed include philosophy, economics, insurance, sociology, statistics, physician, nursing, and
psychology. The differences in uncertainty in each of the many fields it is employed are so subtly
diverse that it can be difficult to determine differences. The following discussion will address
uncertainty in its entirety, as well as, specifically in the selected fields of nursing and
psychology.
Identification of the Concept
Uncertainty in the specific event of illness is characterized by the failure to attain the
meaning for the medical occurrence. Illness uncertainty is developed when a patient is unable to
use past experiences to help them cope with a life-changing event (Bailey, et al., 2010). It can
include vagueness of the condition or the patient’s identification of the vast indicators about the
value and efficiency of the purposed treatment (Mauro, 2010). Due to the vast qualities
uncertainty holds it can be interpreted in many different ways.
Among the many issues that arise from uncertainty, difficulty in clinical assessment is
one of the primary complications. These issues develop from not only patient uncertainty but
also from physician uncertainty. In a study by Politi and Legare (2010), the effect of the doubt
derived through uncertainty on shared decision -making (SDM) between the patient and general
practitioner is observed. In their research the authors assert that SDM is essential and physicians
who manage there ambiguity are more likely to promote and participate in SDM. Politi and
Legare (2010), using longitudinal data a cross sectional analysis was performed on SDM among
UNCERTAINTY
4
primary physicians. The study found that doctors experienced anxiety from uncertainty, as well
as, reluctance to reveal uncertainty to patients. Conclusions drawn by the authors state that
measuring and observing the reactions of uncertainty by physicians is essential to bettering SDM
implementation there in by improving clinical assessment and treatment (Politi & Legare, 2010)
The author picked this concept because of how much uncertainty can impact a patient’s outcome.
At some point or another most patients will experience some degree of uncertainty. Through this
research the author hopes to utilize the knowledge gained to better identify with a patient’s needs
and thereby increase positive outcomes for patients and their families.
In the Field of Nursing
One of the most transcending factors of uncertainty is that it is an inescapable fact
of decision-making regardless if it is a decision being made about remodeling a home or patient
care. Specifically in the field of nursing, uncertainty is an unfortunate and unavoidable
occurrence (Vaismoradi, Salsai, & Ahmadi, 2010). Thompson & Dowding (2001) state that
many of nursing decisions and judgments are made from intuition and using their intuition can
actually decrease uncertainty. Nurses utilize their intuition, along with their base knowledge,
because many times there is not time to consult with a doctor before a decision is made.
The major issues that nurses and other healthcare employees encounter are how to make
decisions under the pressure of uncertain medical circumstances. Stress in nursing research is
predominantly focused on work characteristics that include workload, autonomy, and uncertainty
as important determinants of psychological, physiological and behavioral consequences
(Vaismoradi, et al., 2010). Uncertainty can effect the environment in such a way that it can lead
staff nurses to develop feelings of distress and ambivalence. Nurses also experience feelings of
ethical concern due to uncertainty about the optimal course of treatment for patients. Nurses also
UNCERTAINTY
5
carry the burden of a patient’s death even if they identified the problem and subsequently the
right treatment was taken. This stress can lead to anxiety for future decision-making. Most often
the nurse will always wonder what she/he could have done differently. This is a heavy burden to
carry as a nurse knowing that every day at work there is a life in your hands.
On the contrary Kamhi (2011) believes that uncertainty might actually enhance a nurses’
ability to adapt to unknown situation because they are more open than a nurse that feels more
certain and confident. Kamhi (2011) also believes that as health care workers, it is our duty to
inform patients when feeling uncertain about what plan of action to take. Some nurses and
practitioners may not want to confess to a patient that they are feeling uncertain because of the
fear that a patient may loose confidence and faith in them (Kamhi, 2011). Groopman (2007)
disagrees and believes that confiding in a patient about the uncertainty of their illness or
treatment options can actually enrich a patient’s experience. It is also suggested that showing
uncertainty can allow a patient to better understand and accept when a treatment option fails
(Groopman, 2011).
In the Field of Psychology
Similar to nursing, the field of psychology is also an inevitable environment to
uncertainty. Psychological factors arising from uncertainties is often related to medical issues
and are due to the increase of stress from being diagnosed with health problems, no matter the
severity. In one study, uncertainty was strongly correlated with psychological distress in
adolescents newly diagnosed with cancer (Stewart, Mishel, Lynn, & Terhorst, 2010). In children
and adolescents that survived cancer there is often the lingering feeling of wondering when the
cancer will return (Lee, 2006). Many times in these patients uncertainty about their illness can
UNCERTAINTY
6
progress to post traumatic stress symptoms (Lee, 2006). These symptoms can begin to interfere
with the patient’s outcomes and can inhibit them living their life, even when cancer free.
In a further study by Lin, Yeh, and Mishel (2010) observations showed social support can
increase development through uncertainty by lowering parental perplexity and encouraging more
coping in cases where children have been diagnosed with cancer. A patient that can rely on a
strong support group and who feels loved regardless of the outcome can generally deal with the
situations better. A loss of control can also make patients experience high anxiety due to the
feeling that they are not involved in the decision making process. In the author’s experience,
some younger patients will do whatever they can to regain some control and it can even result in
patients not taking their medication. The author has experienced a young female lung transplant
patient who stopped taking her immunosuppressant medications because the she was tired of
being different and doing what everyone else wanted her to do. The patient ultimately died
because she had severe rejection. It is important for patients to be a part of their care and because
all patients are different, its important to provide for different ways of coping. The other coping
mechanisms, such as religious and spiritual growth were also thought to foster dealing with and
surviving an illness (Lin, et al., 2010).
Aim of Analysis
Furthermore, in this author’s experience, a patient that is newly diagnosed with a life
threatening illness does not deal with their diagnosis as well as a patient diagnosed with a
chronic illness. It takes a longer time for someone who was seemingly healthy, prior to their
hospitalization, to wrap their mind around the new lifestyle that has been forced upon them. It
can be difficult for a patient to imagine all of the lifestyle changes that can occur with their new
diagnosis. Often patients that arrive in Heart and Lung Transplant Intensive Care Unit are
UNCERTAINTY
7
diagnosed with catastrophic illnesses, which result in major life changes. Some of these patients
who were normal a week ago, are now told that they have to have a heart transplant or have a left
ventricular assist device. Imagine the range of emotions these patients experience. On the other
hand, a patient with a chronic illness such as cystic fibrosis, who has lived with the possibility
that one day they would have to have a transplant, generally deals with the news with a little less
anxiety. Obviously each of these patients has a lot to consider and will have to deal with many
emotions, and the author is not implying that either journey is easier than the next. It is by
observation the author concludes that patients with a chronic illness often deal with a decline in
health better initially than those patients who are diagnosed for the first time. A patient who has
been sick their entire life understands their diagnosis and knows what to expect so most of the
time, it is less stressful for them. Any uncertainty in a patient causes most patients psychological
distress.
Uncertainty may be a seemingly simply characteristics, but it has the ability to cause
confusion and doubt during any type of event. The term’s very nature makes it an interesting and
important concept. Those factors are the reason the author believed this was an essential concept
to analysis. By fully understanding this complex idea the author believes that one can better be
able to help prevent negative outcomes to situation where uncertainty occurs and also to help
increase communication about fears, as well as, faults.
Three factors that contribute to uncertainty are lack of knowledge, dissimilarity in
analysis, and disagreement with evidence (Vaismoradi et al., 2010). A person obtaining partial
or inadequate information of an event results in lack of available evidence. Differences in
interpretation uncertainty occur due to restrictions in current empirical data. And finally the third
category is a by-product of the first and second categories and is due to a struggle in discerning
UNCERTAINTY
8
between the persons own lack of knowledge and the limitations of present date knowledge
(Vaismoradi et al., 2010).
Analysis of the Concept
Meleis (2012) describes a concept analysis as a way to expand your idea. Walker and
Avant concept analysis process was chosen for this paper. The author will discuss the seven steps
and the process of analysis of the information gathered for uncertainty. Uncertainty is a universal
and inherent idea that transcends across many different domains. It occurs when someone
experiences doubt, a lack of education, lack of control, and lack of family support. Using process
analysis, the author will describe the steps in developing the concept of uncertainty.
Process of Analysis
The author used Walker and Avant’s (2011) eight steps to gain direction and to develop
an outline. The eight steps begin with picking a concept, decide on the intention of the aim,
distinguish between the many uses of uncertainty, define the characteristics and traits of the
concept, pick a model case, determine the additional cases, identify what precedes the concept
and what results from the concept, and lastly describe empirical referents (Walker & Avant,
2011). The steps are listed in chronological form but during the process of gaining more
information, it may be necessary to revise previously completed steps (Walker & Avant, 2011).
Each step was utilized and scrutinized to better develop the structure of this concept analysis
paper. This structure fits best with the approach the author was taking to discuss uncertainty and
to demonstrate her thoughts associated with it. This analysis will be an in-depth look at the idea
of uncertainty and what can be done to promote lowering the negativity it can have on outcomes.
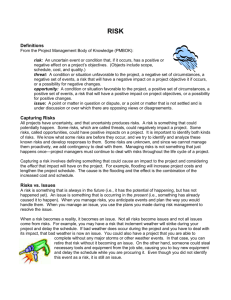
Figure 1 depicts a concept map and the physical process of concept analysis as it relates to
uncertainty as a concept.
UNCERTAINTY
9
Antecedents
The events that precede the feelings of uncertainty are called antecedents (Walker &
Avant, 2011). These events identified by the author are diagnosis of an illness, other concurrent
illnesses, un-education, and anxiety. When newly diagnosed patients are given information that
may change their life, it can be hard to handle. Lee (2006) stated that newly diagnosed
adolescent cancer patients had higher anxiety and feelings of uncertainty than those that had time
to process their diagnosis. These patients had concerns about their health care providers, survival
rates, and what kind of pain they would be in (Lee, 2006). Stress can also be linked to symptom
suffering and onset (Wallace, 2004). On the other hand, Decker, Haase, and Bell (2007) found
that patient that were five or more years from diagnosis of cancer had a higher uncertainty due to
their knowledge of the disease. These patients had questions that were unanswered and because
of their higher knowledge of their illness, had more anxiety over the potential of relapses
(Decker et al., 2007). Wallace (2004) found that patients who had a higher understanding of their
illness and treatment options, had a decrease in uncertainty.
Attributes
When a decision of any nature is being made a person is obligated to choose between
multiple alternatives in which each choice displays a variety of attributes that possess a
quantitative and qualitative character. Without completely observing and understanding all
attributes concerned one can not properly make a decision. In the concept of uncertainty lack of
control, fear of unknown, and lack of shared decision making are all attributes. Kamhi (2011)
found that patients that were told the truth, even when the doctors themselves were feeling
uncertain, was more apt to dealing with stressful situations. These factors whether individually
or combined can lead a person to be uncertain about the next steps that will led to a positive
UNCERTAINTY
10
outcome within an event. This notion is increased when the event itself has a severe or intense
disposition by already creating a naturally stress itself. Patients or families can experience fears
of the unknown because of unsure life expectancies of an illness (Lee, 2006). It is also suggested
that by giving patients some control of their care and providing them with information about
their illness can decrease anxiety and uncertainty they experience (Lee, 2006). Uncertainty can
also be caused by patients feeling as if they do not have a say in their care, especially when the
patient is an adolescent (Decker et al., 2007). Likewise, breast cancer patients often feel
uncertainty after their treatment is complete because of feelings of detachment from medical
personnel (Sammarco & Konecny, 2010). Nursing is already a very stressful environment and
when it is coupled with the addition of uncertainty, it can lead to a fear of being wrong.
Consequences
A concept results in a consequence or outcome and may help point to new research ideas
and views (Walker & Avant, 2011). The author examined the outcomes for uncertainty and
determined several factors from the literature reviewed. The consequences identified for
uncertainty are insecurity, anxiety, withdrawal and loneliness, lack of faith in treatment, and
anxiety about having to rely on others. Insecurity often plagues the average person and this is
often amplified in patients with a life changing illness. Women with chronic heart failure
displayed feelings of insecurity about their declining bodily functions (Burstrom, Brannstrom,
Boman, & Strandberg, 2011). These women also felt lonely and felt guilty about their family
having to take care of them (Burstrom et al., 2011). Heart failure is often very erratic and
uncontrollable which also lead to the women feeling fear and anxiety (Burstrom et al., 2011). A
patient may wonder what will happen in the future and have anxiety about the unpredictable
nature of their illness (Pritchard, 2011). The loss of control over their body made the women fear
UNCERTAINTY
11
for the future, and even death. Heart failure symptoms can present in many different ways and
because of this, it can sometimes be misdiagnosed. Patients may feel as though they are being
brushed off and not taken seriously. When patients feel as though their complaints are not being
heard it can result in a lack of faith in health care (Burstrom et al., 2011).
Empirical Referents and Measurement Tools
Empirical referents are not used to directly measure the concept but are utilized to
distinguish between the attributes (Walker & Avant, 2011). They are helpful in discriminating
between ideas because they are connected to the foundation of the concept. The empirical
referents identified for uncertainty are lack of shared decision-making, loss of control, fear of the
unknown, and anxiety.
Empirical referents can be measured by qualitative or quantitative methods. Qualitative
methods are subjective and could be measured by having a patient fill out a questionnaire or
simply in a face-to-face interview (Leithner et al., 2006). Quantitative methods are more
objective and can measured by scales such as the Hospital Anxiety and Depression Scale
(HADS). The measurement tool utilized for anxiety is the (HADS) (Pritchard, 2011). It takes
approximately two to five minutes to complete and is composed of two sections, one for anxiety
and one for depression. Each question is given a score of zero to three and then added up at the
end of the tool. A score of greater than eleven means that patient is at high risk for anxiety and
depression, a score of eight to ten are at borderline risk, and less than seven are normal.
Mishel’s Uncertainty in Illness Scale was utilized to determine the level of uncertainty
patients were feeling (Decker et al., 2007). This scale is made up of two or four components. For
the purpose of determining uncertainty in this paper, the author will use the two-component
scale. This scale is divided into two groups, ambiguity and complexity (Decker et al., 2007).
UNCERTAINTY
12
Ambiguity is made of sixteen questions that are connected to illness and complexity is made up
of twelve questions that are about their view of treatment and health care (Decker et al., 2007).
These questions are graded on a one to five scale with one being strongly agrees and five being
strongly disagrees (Decker et al., 2007). The questions are scored with the highest score meaning
high uncertainty (Decker et al., 2007).
Case Illustrations
The author will discuss three cases, a model case, a borderline case, and a related case
that exhibits attributes of uncertainty. The model case is an example that embodies the concept of
uncertainty and will contain all of the attributes of uncertainty (Walker & Avant, 2011). The
borderline case will contain the majority of the attributes of uncertainty but will be unlike the
model case in some way (Walker & Avant, 2011). Unlike either of the previous cases, the related
case may only contain some of the attributes of uncertainty but is still linked with the concept.
The author will discuss examples of each case and how each relates to the concept of
uncertainty.
Model Case.
A 32-year-old woman was admitted to Heart and Lung Transplant Intensive Care Unit
(HTICU) via critical care transport. She presented with post-partum cardiomyopathy from an
outside hospital. She came to the emergency room with complaints of shortness of breathe and
fatigue. Post-partum cardiomyopathy was diagnosed by chest x-ray and echocardiogram and she
was then transferred to University Hospital at Birmingham (UAB) for further evaluation. Upon
arrival the patient was lethargic and was hemodynamically unstable. The physicians informed
the family that the patient would need emergent surgery to place a left ventricular assist device
(LVAD).
UNCERTAINTY
13
There are many factors that arise due to this situation. Life after a LVAD is quite
different and such a dramatic life style change. The patient can never be left alone, the patient
can not take a bath, the patient has a driveline that exists through their abdominal wall, and the
patient will always have to be aware of the device. The device has to always be hooked to two
sources of battery power, and for this reason it makes it difficult to just maintain every day tasks.
This patient in particular had a tough time adjusting to her new life. She did not choose to get the
device, even though she understood that her family had to make the choice to keep her alive, no
matter the cost. She feared for the future, whether or not she could have anymore children,
whether or not she would ever get rid of this device, or whether or not she would ever lead a
normal life. She was not married and wondered if anyone would ever love her with a machine
hanging off of her body. She felt as if she lost total control of her body and her life.
The antecedents that she experienced were un-education and diagnosis of an illness.
Since she had previously been healthy, being diagnosed with a life threatening illness was hard
for her to adjust to. She was really sick when she was admitted and therefore did not get the
teaching on the device or get to talk any patient that had a device, and because of this she felt
like she was in the dark. Her feelings of the fear of the unknown, fear of the future, lack of
shared decision making, and anxiety were attributes and empirical referents identified for
uncertainty. The outcomes of her situation resulted in her exhibiting insecurity about having this
machine attached to her body, anxiety and fear about her future with the device, and worried that
her family would feel burdened by her. She was afraid that because she required so much
attention and care that no one would ever love her, leaving her feeling lonely.
The HADS tool was used on this patient to determine her level of anxiety. She took the
test and scored a fifteen, indicating that she was at a high risk for anxiety and depression. Since
UNCERTAINTY
14
this is an attribute of uncertainty, it was also decided to use Mishel’s Uncertainty in Illness Scale.
She scored high on that scale, indicating she had a high level of uncertainty. This case is ideal
and contains all of the characteristics identified in this paper.
Borderline Case.
A 63-year-old man was admitted with a congestive heart failure exacerbation. He was
evaluated for medical management versus LVAD. While the tests were being conducted he was
started on a Primacor drip. After the tests were complete, the patient was noted to be eligible for
a LVAD. The doctors presented him with all of the data from his tests, such as a right heart
catheterization, and told him that he would need the device. The patient felt so much better since
being started on the Primacor drip and did not understand why he needed the LVAD. The
doctors explained that even though he felt fine right now that did not mean he would feel fine
tomorrow. They also explained that if he did not get the device and his health rapidly declined,
then he may not be eligible or if he did get the device he may not have a good recovery. The
patient was given the choice on whether or not to proceed with surgery or to be discharged home
on intravenous Primacor therapy. The patient exhibited fears of the unknown regarding his
health. If he went home and got really sick, he may not survive the surgery, and on the other
hand, he did not want to deal with the lifestyle change of the LVAD. He did feel like he was
involved in the decision making process, which made his outcome more positive. He felt like
even though it was his decision that he still was losing control of everything.
The antecedents the he experienced are diagnosis of an illness and he did not experience
un-education. Due to his stable health, he was given a video to watch about the device, patients
with the device came and spoke to him, and LVAD coordinators brought the equipment around
UNCERTAINTY
15
so that he could see how it worked. Some of the attributes and empirical referents that he
experienced matched the attributes for uncertainty. These attributes and empirical referents that
matched were a loss of control fear of the unknown, and anxiety. He did not experience lack of
shared decision-making because he was given the opportunity to make the decision about
whether or not to get the device or go home on a Primacor drip. The outcomes the patient
experienced resulting from uncertainty was insecurity, anxiety, and anxiety about having to rely
on others.
The HADS scale indicated that the patient was a borderline case for anxiety and
depression. The Mishel’s Uncertainty in Illness Scale was also preformed. The scale revealed
that the patient had a high level of uncertainty but not as high as the model case patient. This
patient demonstrates a clear connection to uncertainty and contains most of the characteristics
identified in this paper.
Related Case.
A 45-year-old woman was admitted with increased shortness of breath and was referred
from her cardiologist to UAB. She was being evaluated for heart transplant versus LVAD. Her
tests showed that she was eligible for both procedures and the doctors gave her the choice. They
told her that she could go home on Primacor infusion and wait for a transplant or she could get
the LVAD and build her strength. In the past other patients that were really deconditioned
recovered slowly from LVAD surgery. Even though they recovered slower than the average
patient, the device gave them time they may not of had to wait on a transplant. Often patients that
get a LVAD also build up their body and do better once they are transplanted. She chose to go
ahead and get the LVAD. She felt good about her decision because she had plenty of time to
discuss her options and to make an informed decision. She talked with patients that already had a
UNCERTAINTY
16
LVAD and was able to see what her life would be like living with an assist device. Even though
she felt good about her decision, she still had some fears for her future. She wondered how
painful surgery would be and how her family would respond to the demands of the LVAD
program. Since she was able to make her own decision about which route to take, she felt
confident that the LVAD was the right choice for her.
The antecedents that she experienced prior to uncertainty were diagnosis of an illness and
un-education. At first she was not sure what to expect, but once she had all of the information in
front of her and she was taught about each procedure, she was sure that she wanted to get the
LVAD. The attributes and empirical referents that were identified in her case are anxiety. She
did not experience the other attributes and empirical referents related to uncertainty, such as; lack
of shared decision-making, loss of control, and fear of the unknown. She was able to have the
final say as to which procedure she would have and felt as though the doctors listened to what
she needed, which allowed her to have some control. The outcomes experienced as a result of
uncertainty are insecurity and anxiety. She felt confident that she and her family were told about
what to expect and what kind of life style change that it would be, which allowed everyone to be
prepared.
The patient completed the HADS to determine her level of anxiety and depression. Her
results showed that she was a low borderline case for anxiety and depression. She was also asked
to perform the Mishel’s Uncertainty in Illness Scale. That scale determined that while she
exhibited high uncertainty, it was less than the other two cases, model and borderline. This case
is related to uncertainty but does not contain all of the characteristics of uncertainty.
Analysis Summary
UNCERTAINTY
17
Using the eight steps as defined by Walker and Avant (2011), one can identify a process
to develop a concept. These eight steps, choosing a concept, determine the aim, pinpoint all uses
of the concept, define the attributes, discover a model case, identify borderline, related, contrary,
invented, and illegitimate cases, define antecedents and consequences, and determine empirical
referents, are used to revise and enhance a concept (Walker & Avant, 2011). This process is ever
changing and also serves to obtain the defining attributes of a concept (Walker & Avant, 2011).
Ultimately the process of concept analysis can decrease ambiguity and clarify interpretations of
everyday nursing practice (Falan, 2010).
Implications/Application to Nursing Practice
Uncertainty impacts most everyone, from all walks of life, at some point or another. For
example, nurses deal with having uncertainty with difficult decision-making, patients deal with
uncertainty when diagnosed with a life threatening illness, and physicians deal with uncertainty
when they are unsure what course of action to take when treating a patient. Nurses touch lives
when they can pull from previous experiences or emotions that can better help them understand
what their patient is going through. In this case, because most everyone has experienced
uncertainty, a nurse can utilize past experiences to adjust patient care to better accommodate a
patient experiencing uncertainty.
Some interventions that could decrease a patient’s anxiety and feelings of uncertainty are
educating the patient, spending time with a patient, answer questions the patient might have, and
being an advocate for the patient. As previously stated, Wallace (2004) found that as a patient
became more educated about their illness, uncertainty decreased. As a nurse on Heart Transplant
Intensive Care Unit (HTICU), the author understands that educating patients about their illness is
an important part of recovery. University Hospital at Birmingham utilizes patient education
UNCERTAINTY
18
sheets that are given to patients when they are prescribed new medications or are diagnosed with
a new illness. On HTICU a pharmacist teaches heart transplant patients their new medications
and before they can leave the hospital, they have to be checked off. This is an example of
educating patient to decrease any uncertainty and allowing patients to take control of the
situation.
Sometimes it is necessary to spend a little extra time with patients that are experiencing
uncertainty. This can provide reassurance and establish a rapport with a patient that might
otherwise feel alone. Allowing the patient to voice their concerns can also promote
communication between patients and the medical staff. This time can also be used to find out the
needs and questions of the patient. Often times patients do not think of questions until after the
physician leaves, and so communicating with the patient can allow the nurse to fill the
communication gap to ensure the patient is receiving the best care possible. Understanding the
concept of uncertainty and how it affects patients and their families while also adopting
suggested interventions could decrease overall uncertainty and increase positive patient
outcomes.
UNCERTAINTY
19
References
Baily, D.E., Barroso, J., Muir, A.J., Sloane, R., Richmond, J., McHutchison, J., et al.
(2010). Patients with chronic hepatitis c undergoing watchful waiting: Exploring
trajectories of illness uncertainty and fatigue. Research in Nursing & Health. 33(5), 465473. doi:10.1002/nur.20397
Burstrom, M., Brannstrom, M., Boman, K., & Strandberg, G. (2011). Life experiences of
security and insecurity among women with chronic heart failure. Journal of Advanced
Nursing, 1-10. doi:10.1111/j.1365-2648.2011.05782.x
Decker, C., Haase, J., & Bell, C. (2007). Uncertainty in adolescents and young adults with
cancer. Oncology Nursing Forum, 34(3), 681-688.
Falan, S. (2010). Concept analysis of similarity applied to nursing diagnoses: Implications
for educators. International Journal of Nursing Terminologies and Classifications, 21(4),
144-155. doi:10.1111/j.1744-618x.2010.01163.x
Groopman, J. (2007). How Doctors Think. New York, NY: Houghton Mifflin.
Kamhi, A.G. (2011). Balancing certainty and uncertainty in clinical practice. Language,
Speech, and Hearing in Schools, 42, 59-64. doi:10.1044/0161-1461(2009/09-0034)
Lee, Y. (2006). The relationship between uncertainty and posttraumatic stress in survivors of
childhood cancer. Journal of Nursing Research Taiwan Nurses Association, 14(2), 133142.
Leithner, K., Assem-Hilger, E., Fischer-Kern, M., Loffler-Stastka, H., Thein, R., & PonocnySeliger, E. (2006). Prenatal Diagnosis, 26(10), 931-937. doi:10.1002/pd.1529
Lin, Y., Yeh, C.H. & Mishel, M.H. (2010). Evaluation of a conceptual model based on Mishel’s
theories of uncertainty in illness in a sample of taiwanese parents of children with
UNCERTAINTY
20
cancer: A cross-sectional questionnaire survey. International Journal of Nursing Studies,
47(12), 1510-1524. Doi:10.1016/j.ijnurstu.2010.05.009
Mauro, A.M., (2010). Long-term follow-up study of uncertainty and psychological adjustment a
among implantable cardioverter defibrillator recipients. International Journal of Nursing
Studies, 47(19), 1080-1088.
Meleis, A.I. (2012). Theoretical nursing: Development & progress, 5th ed. Philadelphia, PA:
Wolters Kluwer/Lippincott, Williams & Wilkins.
Politi, M. C. & Legare, F. (2010). Physicians reactions to uncertainty in the context of shared
decision making. Patient Education and Counseling, 80(2), 155-157.
Pritchard, M.J. (2011). Using the hospital anxiety and depression scale in surgical patients.
Nursing Standard, 25(34), 35-41.
Sammarco, A. & Konecny, L.M. (2010). Quality of life, social support, and uncertainty among
Latina and Caucasian breast cancer survivors: A comparative study. Oncology Nursing
Forum, 37(1), 93-99. doi:10.1188/10.ONF.93-99
Stewart, J. L., Mishel, M.H., Lynn, M.R., Terhorst, L. (2010). Test of a conceptual model of
uncertainty in children and adolescents with cancer. Research in Nursing & Health,
33(1), 179-191.
Thompson, C. & Dowling, D. (2001). Responding to uncertainty in nursing practice.
International Journal of Nursing Studies, 38(5), 609-615.
doi:10.1016/s0020-7489(00)00103-6
Vaismoradi, M., Salsai M., Ahmadi, F. (2010). Nurses’ experiences of uncertainty in clinical
practice: A descriptive study. Journal of Advanced Nursing, 67(5), 991-999.
Walker, L.O., & Avant, K.C. (2011). Strategies for Theory Construction in Nursing (5th ed.).
Upper Saddler River, NJ: Pearson Prentice Hall.
UNCERTAINTY
21
Wallace, M. (2004). Finding more meaning: The antecedents of uncertainty revisited. Journal of
Clinical Nursing, 14(7), 863-868.
UNCERTAINTY
22
Figure 1
Uncertainty as a concept
Definition
Uncertainty
Antecedents
Uncertainty
results in
consequences
All must be there
for a model
example
Nursing
Consequences
AIM
Psychology
Attributes
The related case may
only exhibit one of the
attributes
Related
case
Measure
Attributes
Empirical
Referents
The borderline case
Exhibits most, but not
all of the attributes
Borderline
case
Model
Case
The model
case possesses
all of the
attributes
LEGEND
For cases
Represents the relationship of the
model case and the attributes of
uncertainty. The model case will
exhibit all of the attributes
Demonstrates the relationship between
attributes and the borderline case. The
borderline case will exhibit most of the
attributes, but not all of them
Demonstrates the relationship
between attributes and the related
case. This case is connected to the
concept but does not display all of the
attributes.