The Evolving Role of Nursing in ACOs and Medical Homes
advertisement

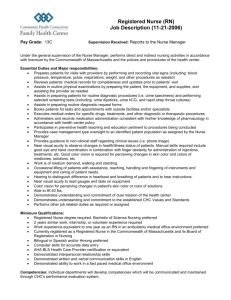
The Evolving Role of Nursing in ACOs and Medical Homes Carol A. Conroy DNPc RN CNOR Chief Nursing Officer/VP Operations VONL SUMMIT: April 19, 2013 The Care Span: The Significance of Transitions • Transitions: Handovers are vulnerable exchange points that contribute to unnecessarily high rates of health services use • 2009 study reported 20% of Medicare beneficiaries discharged from hospitals were re-hospitalized within 30 days; 34% within 90 days. • 13% of Medicare beneficiaries experience 3 or more provider handovers during a 30 day period • Patient “churning” accounts for $15 billion in annual Medicare spending • Transitional Care is a broad range of time-limited services designed to – ensure health care continuity – avoid preventable poor outcomes among at-risk populations – promote the safe and timely transfer of patients from one level or type of care setting to another Hallmarks of Transitional Care • Focused on highly vulnerable, chronically ill patients throughout critical transitions in health and health care • Considers the time-sensitive nature of services • Emphasizes the education of patients and family care-givers • Compliments, but not the same as primary care, care coordination, discharge planning, disease management and case management What Patient-Centeredness Should Mean • Power and control shifts into the hands of patients, families, and communities • Status quo: the cathedral of care is the hospital and health care professionals are the “hosts” • New order: health care professionals are guests in the patients’ lives Clinical Nurse Specialist (CNS) Role Redesign • Acute Care Based • Practice in settings across the continuum • Focus on inpatient care delivery • Focus on high-risk populations • High degree of setting control • Patient self-management and shared decision making CNS Role Re-design • Re-engineered an existing resource to address the needs of patients at high-risk for failure after discharge • Shifted the focus to high risk populations across multiple care settings or the patient home Who really Controls Outcomes? The majority of health care occurs at the low-acuity end of the scale, where outcomes are controlled not by physicians or “the system” but by the everyday choices of individuals and families, which are strongly influenced by their values, culture and communities. The largest opportunity clinical staff have to influence health outcomes is to influence choices by partnering over time. 100 Patient/Family “Control” The “System” 0 Low “Acuity” High Ref: Gottlieb, Sylvester and Eby. Transforming Your Practice: What Matters Most. Family Practice Management. www.aafp.org/fpm. January 2008. Key Concepts • Patient/Family control. Think of low acuity as being the home setting and high acuity being the intensive care unit. The patients lifetime of “Health” management occurs in the low acuity setting where the patient makes their health decisions. • New skills for nursing in the low acuity setting include shared decision making, patient goal setting and selfmanagement. • The medical home provides the environment for the application of these skills • The CNS identifies and assists the patient to manage risks during complex care transitions and facilitates exquisite coordination of handovers. Element Transitional Care Nurse (TCN) Blueprint Case Manager Home Health Nurse Education Masters Prepared Clinical Nurse Specialist UPenn TCN trained RN BSN RN Setting All settings across the continuum Non-SVHC settings (Tertiary care, nursing homes, patient home) Single primary care practice Residence of referred patients that meet payer criteria Population High-Risk, high utilizers Complex patients with multiple providers or settings of care No payer referral required Primary care practice population Only home bound patients that meet payer criteria Key Functions Coordination and collaboration across multiple providers and care settings Identification of high-risk patients Intensive disease management and care coordination of individual patients Research on best-practice and outcomes Implementation and spread of evidenced-based practice across care setting Address systemic care transition process issues Assessment and risk identification Panel management Population management Wellness and prevention Chronic disease management Case management Patient education Patient goal setting Assessment and risk identification and referral Panel management Population management Wellness and prevention Chronic disease management Case management Patient education Patient Goal setting Service Duration Time limited (8-12 weeks per patient) The duration a patient is member of primary care practice panel Intermittent short episode of care. Number of visits limited Challenges to the CNS role redesign • Shift away from acute care focus to the continuum of care • Staff training and role redefinitions • Avoid duplication of services • Patient navigation across multiple, complex medical settings • Patient/family directed care CNS Redesign Strategies • Orientation to transitions across the continuum • Identification of high-risk patients • Focus on the patient not the disease • Use of Patient self-management tools • Use of Shared decision making • Transitions Team includes community partners • Communication with the primary care practice teams in medical homes • Formal education in partnership with UPenn References American Academy of Nursing. (2012). Policy Brief 3.5.12. The Imperative for Patient, Family and Population Centered Interprofessional Approaches to Care Coordination and Transitional Care. ANA. (2012). White Paper: The Value of Nursing Care Coordination Berwick D. “What ‘Patient-Centered’ Should Mean: Confessions of an Extremist” Health Affairs, July 19, 2012 Brock J, Mitchell J, Irby K, Stevens B, Archibald T, Goroski A, Lynn J. “Association Between Quality improvement for Care Transitions in Communities and Rehospitalizations Among Medicare Beneficiaries.” JAMA, 23/30, Vol 309, No.4, 2013 Clavelle J. “Implementing Institute of Medicine Future of Nursing Recommendations: A Model for Transforming Nurse Practitioner Privileges.” JONA, Vol. 42, No.9, 2012 Goodman DC, Fisher E, Chang C,. “The Revolving Door: A Report on US Hospital Readmissions.” Robert Wood Johnson Foundation/The Dartmouth Institute; 2013 Naylor MD, Aiken LH, Kurtsman ET, et al. “The Care Span: The Importance of Transitional Care in Achieving Health Reform.” Health Affairs, 304(4): 746-754, 2011 Sherman RO. “Lessons in Innovation: Role Transition Experiences of Clinical Nurse Leaders.” JONA, Vol. 40, No. 12, 2010