Pediatric OTCs - Canadian Healthcare Network
advertisement

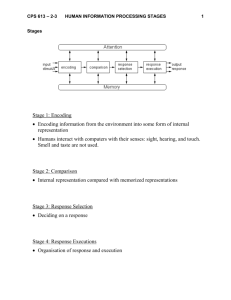
Pediatric OTCs Carolyn Whiskin, BScPhm Disclosure Honoraria have been received from the following companies in preparing, reviewing and giving presentations: Pfizer Abbott Merck GlaxoSmithKline Objectives • To understand the Canadian Paediatric Society Guidelines regarding cough, cold and fever • To understand treatment options and supportive measures for these conditions • To be able to integrate homeopathic and traditional medication in pediatrics The Common Cold • Young children have lowered immunity to the more than 100 different cold viruses • Not uncommon to get as many as 8–10 colds/yr before age 2 • Fewer colds with age as exposure increases and immunity develops • Typical symptoms: runny/stuffed-up nose, sneezing, coughing ,headache, mild sore throat, loss of appetite, fatigue, mild fever http://www.caringforkids.cps.ca/handouts/colds_in_children When To Refer Babies younger than 3 months • having trouble breathing • not eating, or if they are vomiting • have a fever (rectal temperature of 38.5°C or higher) When to Refer Children of all ages • Breathing rapidly or seem to be working hard to breathe • Blue lips • Coughing causing choking or vomiting • Waking with one or both eyes stuck shut with dried yellow pus http://www.caringforkids.cps.ca/handouts/colds_in_children When to Refer • Much more sleepy than usual, doesn’t want to feed or play, or is very fussy and cannot be comforted • Thick or coloured (yellow, green) discharge from the nose for more than 10 to 14 days. • Any sign of a middle ear infection (ear pain, drainage from the ear) http://www.caringforkids.cps.ca/handouts/colds_in_children Spreading a Cold Viruses live in the nose, mouth, eyes and skin and can stay on surfaces for many hours Germs can spread whenever we touch one of these things and then touch our nose, mouth or eyes before washing our hands http://www.nj.gov/health/flu/documents/module3.pdf Hand Washing Hand washing • 15 to 20 seconds with warm water and soap for the time it takes to sing “Happy Birthday” twice • Avoid kissing, touching or holding hands • Elbow cover cough – droplets spread several feet http://www.caringforkids.cps.ca/handouts/colds_in_children Pertussis Prevention • Also known as whooping cough • 25 infant deaths in the USA in 2010 – majority spread from adults • Adults age 19–65 require a Tdap booster • Adults over 65 require a booster if they will be in close contact with an infant • Pregnant woman not already vaccinated should receive a booster in the late 2nd semester or 3rd trimester http://www.adultvaccination.org/whooping_cough_vaccine_pertussis_vaccination_adult_immunization.htm Cough and Cold • Health Canada Guidelines • As of the fall of 2009 all products containing traditional antihistamines, antitussives, expectorants and decongestants are to be labelled “Not for use under age 6” • Why the restriction? • Lack of evidence for these products in this age group • Reports of misuse, overdose and adverse effects which include the following: increased heart rate, convulsions, decreased level of consciousness, abnormal heart rhythms and hallucinations Why Restrictions? • Body weight: children aged 2-6 can weigh the same as children under age 2 in whom these medications have not been indicated • Increased exposure due to higher incidence of coughs and colds in this age group • Children less likely to communicate adverse effects from these medications to caregivers Standard Treatment Measures Health Canada feels that most colds resolve in 6-10 days and that there is no “cure” for the common cold Pharmacists can feel comfortable suggesting the following: • Clear nasal passages and ensure that the child gets enough rest • Ensure the child gets plenty of clear fluids (e.g., diluted nonsweetened fruit juice, or clear soups)—this prevents dehydration, reduces congestion and keeps the throat moist • Provide a comfortable environment with enough humidity Which Humidifier To Use? Humidifiers add moisture to the air, which helps ease coughing and congestion due to a cold • Safety-Cool mist preferred to avoid burns • Effectiveness Warm-mist and cool-mist humidifiers are equally effective. When water vapor reaches the lower airways, the temperature is the same. Aim away from bed and sheets. • Cost Cool-mist humidifiers are less expensive than are warm-mist • Cleaning clean to prevent the growth of bacteria and molds. Wiping down the humidifier daily with a 10 percent bleach solution — 9 parts water to 1 part bleach — is one way to safely keep it clean http://www.mayoclinic.com/health/cool-mist-humidifiers/AN01577 Clearing Nasal Passages • Suction with rubber bulb • Squeeze the bulb syringe to expel air • Insert the tip of the bulb about 1/4 to 1/2 inch (0.64 to 1.27 centimeters) into baby's nostril, pointing toward the back and side of the nose • Release the bulb, holding it in place while it suctions the mucus • Remove the syringe and empty the contents onto a tissue by squeezing the bulb rapidly while holding the tip down. • Clean the bulb syringe with soap and water http://www.mayoclinic.com/health/common-cold-in-babies/DS01106/DSECTION =lifestyle-and-home-remedies Nasal Aspiration • First may use saline solution to dilute secretions • Wash device with warm water • Insert filter • Insert bulb into nostril while placing mouthpiece in caregiver’s mouth for inhalation • Remove filter and clean device Saline Solutions Benefits of rinsing: flushes out thickened mucus and irritants, may help ease swelling in the lining of nasal passages Irrigation solution preparation: dissolve 1/8 teaspoon of table salt into 8 ounces of warm water Commercially available products use sodium chloride 0.9%; sea salt based products use a deiozinizing process to bring to isotonic while leaving natural minerals Homeopathy: View of the CPS • Canadian Paediatric Society reviewed PubMed, CAM on PubMed, the Cochrane Library and Health Canada’s websites. • No trials analyzing the effects of over-the-counter pediatric homeopathic preparations were found. • There are only a few good studies showing possible benefits of homeopathy when prescribed by trained practitioners for a selected number of specific conditions in children. • Therefore, more rigorous studies showing efficacy need to be completed before it can be recommended as a credible complementary or alternative therapy for the pediatric population. Homeopathy: View of the College of Family Physicians of Canada • “It is important to keep in mind that, when used appropriately, natural health products can be a key part of a person’s health management.” • “Consumers can identify a Health Canada authorized natural health product by the eight-digit Natural Product Number (NPN) or Drug Identification Number for Homeopathic Medicine (DIN-4HM) on the label. These products are also required to have clear labeling on appropriate use, including dosing, risk information and whether they can be used safely in children.” http://www.cfpc.ca/cough and cold medications frequently asked questions More Comments • 1997, by K. Linde et al. (Munich University) published meta-analysis of 135 clinical trials which compared homeopathic drugs with a placebo concluded that "the results of this meta-analysis are not compatible with the hypothesis that the clinical effects of homeopathy are completely due to placebo." 1997, by K. Linde et al. (Munich University Natural Health Product Options Coryzalia • Approved from one month – 6 years of age • Indications: nasal congestion, runny nose and sneezing • Dose: unit dose liquid vial t.i.d. for 5 days Euphorbium • Open, multicenter, prospective, active-controlled cohort study in patients with inflammatory processes and diseases of the upper respiratory tract.The primary outcome was to demonstrate non-inferiority of the homeopathic complex remedy to xylometazoline. • Results: comparable efficacy and tolerability profile of Euphorbium compositum nasal drops SN and xylometazoline in patients with inflammatory processes and diseases of the upper respiratory tract (rhinitis/sinusitis). http://www.ncbi.nlm.nih.gov/pubmed/15772459 Euphorbium • In vitro study using virus plaque reduction assays examined the effect of Euphorbium compositum SN against pathogens causing various viral infections: influenza A virus, respiratory syncytial virus (RSV), human rhinovirus (HRV) and herpes simplex virus type 1 (HSV-1). • Euphorbium showed antiviral activity of against RSV and HSV-1. In addition, an antiviral effect against influenza A virus and HRV. http://www.ncbi.nlm.nih.gov/pubmed/11574744 Euphorbium Dose • Nasal Spray: Age 2 to 12 years,1 spray into each nostril 3 times a day • Oral Drops: Age 2-6, 5 drops 3x/day Age 6-12, 7 drops 3x/day • Acute Dosage: May use drops every 60 minutes up to 12x/d 30- Natural Health Products Viburcol • Indicated for infants and children for: teething, pain, colic, infections with or without fever, sleeplessness and restlessness • Dose: Age 0-2, 5 drops 3 x/day Age 2-6, 8 drops Age 6-12, 10 drops Acute – every 30-60 minutes Suppository: 1 b.i.d. – 0-12 yrs Acute use every 1-2 hours Viburcol Nonrandomized observational study of 38 Belgian centers practising homeopathy and conventional medicine Children <12 years old comparable to acetaminophen for poor eating, cramps, distress, sleep, crying and temperature Cough • An RCT with 139 children (24 to 60 mo) suffering from cough due to upper respiratory tract infection reported that 2.5 mL of honey before sleep improved cough frequency and severity, as well as sleep quality in a mean of 59% of children • Honey was significantly superior to no treatment or honey-flavoured DM cough frequency and severity, bothersome nature of the cough, and the child/parent sleep quality, as rated by the parents http://www.cps.ca/en/documents/position/treating-cough-cold Honey in Infants Younger Than 1 Year • Only food linked to infant botulism • Infant botulism is caused by bacteria called Clostridium botulinum • If honey is contaminated: spores toxins paralysis • Bacteria and toxins are odourless, colourless, tasteless and not destroyed by cooking Health Canada is advising parents and caregivers not to feed honey to children younger than 1 year of age • http://www.hc-sc.gc.ca/fn-an/securit/kitchen-cuisine/infant-botul-infantile-eng.php http://www.hc-sc.gc.ca/fn-an/securit/kitchen-cuisine/infant-botul-infantile-eng.php Fever Normal temperature ranges Method Normal temperature range • Rectal 36.6°C to 38°C (97.9°F to 100.4°F) • Ear 35.8°C to 38°C (96.4°F to 100.4°F) • Oral 35.5°C to 37.5°C (95.9°F to 99.5°F) • Axillary 34.7°C to 37.3°C (94.5°F to 99.1°F) http://www.cps.ca/en/documents/position/temperature-measurement Measurement Methods Summary of recommended temperature measurement techniques Age Recommended technique • Birth to 2 years 1. Rectal (definitive) Axillary (screening low risk children) • 2 to 5 years 1. Rectal (definitive) Axillary, Tympanic (or Temporal Artery if in hospital) (screening) • Older than 5 years 1. Oral (definitive) Axillary, Tympanic (or Temporal Artery if in hospital) (screening) 2. 2. 2. • Canadian Task Force on Preventive Health - Strength of Recommendation B, II [39] http://www.cps.ca/en/documents/position/temperature-measurement Oral • Measures temperature of lingual arteries • Influenced by food/drink and oral breathing • Relies of mouth sealed and tongue depressed for 3-4 minutes • Mercury thermometers are no longer recommended http://www.cps.ca/en/documents/position/temperature-measurement Rectal • Gold standard measurement • Slower to change based on core temperature changes • Affected by insertion depth and stool presence • Rectal perforation rare occurance- caution in neonates (1 in 2 million measurements) • Cleaning needed to prevent spread of fecal contaminants http://www.cps.ca/en/documents/position/temperature-measurement Axillary • Inaccurate estimate of core temperature in children • Exact placement over axillary artery required • Environmental influences • Suggested as a screening in neonates by the American Pediatric Society Tympanic • Measures thermal radiation emitted from the tympanic membrane • Crying, otitis media and wax do not affect readings • Ideal location for core temp. determination • Instrument design, depth of insertion and shape of ear canal can all cause variations • Size of device may affect accuracy in children under 2 years When to Treat • Fever is a sign that the body is working to fight infection – should not be feared • Fever has a purpose and may resolve viral infections sooner • Treatment mainly to provide comfort and reduce parent anxiety • Do not wake a sleeping child to give them a fever reducer • Hydration and watching behavioural change emphasized • No evidence fever reduction reduces morbidity and mortality or decreases the recurrance of febrile seizures When To Refer • Child with fever is less than 6 months old • Fever for longer than than 72 hours • Child is excessively cranky, fussy or irritable • Child is excessively sleepy, lethargic or does not respond • Child is persistently wheezing or coughing • Fever accompanies rash or any other signs of illness that are concerning http://children.webmd.com/news/20110228/new-advice-fighting-fever-children Treatment Choices Acetaminophen • Dose: 10-15 mg/kg per dose q4-6h • No proof that a loading dose of 30 mg/kg works better • Onset of Action: 30-60 minutes • Risk of hepatotoxity with doses over 15mg/kg or at intervals less than 4 hours • Combination treatment may offer slight benefit http://pediatrics.aappublications.org/content/127/3/580/T1.expansion.html Treatment Choice Ibuprofen • Dose: 10mg/kg/ dose every 6-8 hours • Does not worsen asthma symptoms • Can cause gastritis, bleeding and ulcers- less common in acute illness • Nephrotoxicity – renal insufficiency can develop; concern in dehydration where prostaglandin synthesis needed for renal blood flow.- caution in cardiac and renal patients • Not to be used in infants younger than 6 months http://pediatrics.aappublications.org/content/127/3/580/T1.expansion.html American Academy of Pediatrics Variable Acetaminophen Ibuprofen • Decline in temperature, °C 1–2 1–2 • Time to onset, h <1 <1 • Time to peak effect, h 3–4 3–4 • Duration of effect, h 4–6 6–8 • Dose, mg/kg 10–15 every 4 h • Maximum daily dose, mg/kg 90 mg/kg 40 mg/kg • Maximum daily adult dose, g/d 4 2.4 • Lower age limit, mo 3 10 every 6 h 6 http://pediatrics.aappublications.org/content/127/3/580/T1.expansion.html Combination Treatment • Studies indicate combination therapy may be more effective in reducing fever • May not improve discomfort • Caution safety of combination treatment • Dosage confusion can lead to overdose • Generally not recommended http://pediatrics.aappublications.org/content/127/3/580/T1.expansion.html Fighting the Virus Oscillococcinum • RCT showed benefit over placebo in complete resolution or clear improvement in 48 hours (48% vs 63%) • Give one unit dose tube of pellets every 6 hours for 3 doses at the onset of symptoms. Ages 2 y and up (separate from food/toothpaste) Papp R, Schuback G, Beck E, et al. Oscillococcinum in patients with influenza-like syndromes: a placebo-controlled, double-blind evaluation. Br Homeopath J 1998;87:69-76 Fighting the Virus Sambucol • In an RCT – reduced flu symptoms to 3-4 days; influenza antibodies increased and TNF-alpha production increased (44.9 fold) • Study concluded that, in addition to its antiviral properties, Sambucol Elderberry Extract and its formulations activate the healthy immune system http://www.ncbi.nlm.nih.gov/pubmed/11399518; The effect of Sambucol, a black elderberry-based, natural product, on the production of human cytokines: I. Inflammatory cytokines Sambucol Daily maintenance Children 1-6 years of age: take 1 teaspoon (5 mL) daily Children 7-12 years of age: take 2 teaspoons (10 mL) daily Intensive use Children 1-6 years of age: take 1-2 teaspoons (5-10 mL) twice daily Children 7-12 years of age: take 2-3 teaspoons (10-15 mL) twice daily Fighting the Virus Engystol • RCT and observational studies show comparable results to acetaminophen in reducing symptoms and phagocytic activity improved • Children (6 to 12 years) 1 tablet 2 times daily. In acute cases, 1 tablet every 1 to 2 hours, up to 8 times a day • Young children (2 to 6 years) ½ tablet 3 times daily. In acute cases, 1 tablet every 1 to 2 hours, up to 6 times a day • Babies (0 to 2 years) ½ tablet 2 times daily. In acute cases, 1 tablet every 1 to 2 hours, up to 4 times a day • Dissolve slowly in the mouth or in a teaspoon of water before administering to a young child or baby http://www.homotoxicology.net/Documents/Brochures/Engystol.pdf Other Options Echinacea • 2006 Cochrane review identified 16 controlled trials on the effect of echinacea for cough—no sufficient data to suggest the effectiveness of echinacea in children. The use of echinacea for eight to 12 weeks as a prophylactic measure did not result in effective prevention of the common cold (Source: CPS) http://www.cps.ca/en/documents/position/treating-cough-cold Other Options Zinc • Some studies showed benefits, especially if used within 24 h of the onset of common cold symptoms • Other studies showed no benefit • At the present time, the use of zinc in children with cough and cold is not recommended (Source: CPS) http://www.cps.ca/en/documents/position/treating-cough-cold Vaccinations • Use of anti-pyretics before vaccination may reduce the immune response • Sugar water preferred to reduce discomfort before vaccination • To make sugar water, mix one packet of sugar (1 teaspoon) with 10 ml of water (2 teaspoons). Administer with a cup, spoon or syringe just before the needle and discard the unused portion http://www.toronto.ca/health/immunization_children/pdf/howtoreducepain.pdf Making a Difference Providing information to parents regarding the care of their sick child is a vital service pharmacists provide to the community Take the time to share your knowledge We all benefit!!