DETAIL Slide Kit - LandmarkTrials.nl
advertisement

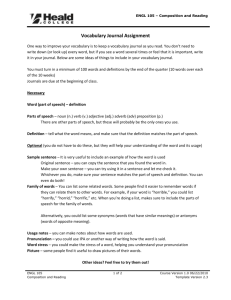
Diabetics Exposed to Telmisartan And enalaprIL Telmisartan in type 2 diabetic nephropathy: reducing long term decline in renal function through RAS Blockade Barnett et al. N Engl J Med 2004;351:1952–1961 Natural history of type 2 diabetic nephropathy Clinical type 2 diabetes Functional changes* Hypertension Microalbuminuria Macroproteinuria Structural changes† Decreasing GFR ESRD Cardiovascular death Diagnosis 2 years 5 years 10 years 20 years * Altered renal haemodynamics, glomerular hyperfiltration † Glomerular basement membrane thickening , mesangial expansion , microvascular changes +/- 30 years 2 Incidence of cardiovascular events (% of patients per year) Increasing albuminuria indicates increasing risk in type 2 diabetes 16 * 14 12 10 8 * 6 4 2 0 Normoalbuminuria *P<0.05 versus normoalbuminuria after adjusting for other risk markers Microalbuminuria Macroproteinuria Gimeno Orna et al. Rev Clin Esp 2003 3 Reduced GFR* increases cardiovascular risk Relative risk* in patients with impaired GFR (95% CI) 6,0 5,0 4,0 3,0 2,0 Increased risk 1,0 0,0 Reduced risk Major cardiovascular event Myocardial infarction *Relative risk of GFR 60 mL/min/1.73m2 compared with GFR >60 mL/min/1.73m2 Stroke Cardiovascular mortality Total mortality Ruilope et al. J Am Soc Nephrol 2001 4 Angiotensin II is central to the pathophysiology of renal disease Glomerular pressure injury Oxidative stress Inflammation Angiotensin II Hyperfiltration Glomerular capillary hypertension Chronic kidney disease Cell and tissue growth Reduction in nephron mass Glomerulosclerosis Brewster, Perazella. Am J Med 2004 5 Antihypertensive drug class recommendations Diuretic b-blocker CCB ACEI ARB Renal insufficiency ESH/ESC (loop) Non-diabetic nephropathy ESH/ESC WHO/ISH Type 1 diabetic nephropathy ESH/ESC WHO/ISH Type 2 diabetic nephropathy ESH/ESC WHO/ISH Proteinuria ESH/ESC Diabetic microalbuminuria WHO/ISH Chronic kidney disease JNC 7 ESH/ESC Guidelines. J Hypertens 2003 JNC 7. JAMA 2003 6 ACEIs in diabetic renal disease • ACEIs: proven to be effective in DM1 and nondiabetic kidney disease • Micro-HOPE: confirmed that ACEIs reduce risk of overt proteinuria and CV events in DM2 patients • Prior 2001, ACEIs considered first line therapy for diabetic patients with nephropathy • Today, ACEI most commonly used antihypertensive class used to treat hypertensive diabetics, with usage ranging from – 49% of patients in Japan – 73% of patients in Germany Lewis EJ, N Engl J Med 1993 GISEN group. Lancet 1997 Remuzzi et al. Ann.Intern.Med 2002 HOPE Study Investigators. Lancet 2000 Vivian et al. Ann Pharmacother 2001 Treatment Algorithms: Hypertension 3rd Edition. Datamonitor 2002. London UK 7 – 60% of patients in The Netherlands ARBs in diabetic renal disease • In major clinical trials, ARBs have demonstrated effective renoprotection in type 2 diabetic nephropathy – RENAAL (ARB vs placebo) – IRMA 2 (ARB vs placebo) – IDNT (ARB vs amlodipine) • Both ACEIs and ARBS are recommended for diabetic hypertension and for the treatment of renal disease in the medical literature and guidelines Parving et al. N Engl J Med 2001; Brenner et al. N Engl J Med 2001 Lewis et al. N Engl J Med 2001; ESH/ESC Guidelines. J Hypertens 2003 JNC 7. JAMA 2003; Johnson. Intern Med J 2004 American Diabetes Association. Diabetes Care 2004 National Kidney Foundation. Am J Kidney Dis 2002 National Kidney Foundation. Am J Kidney Dis 2004 8 ACEIs vs ARBs • ACEI and ARBs block RAS by different mechanisms that may have clinical significance • Prior to DETAIL, no direct clinical comparisons of the two most effective renoprotective therapies (ACEIs and ARBs) • The need for such a comparative study has been a recognized gap in evidence-based medicine • DETAIL is the first trial to address this gap Hostetter. N Engl J Med 2001 Thurman, Schrier. Am J Med 2003 Opie, Parving. Circulation 2002 9 Diabetics Exposed to Telmisartan And enalaprIL Telmisartan in type 2 diabetic nephropathy: reducing long term decline in renal function though RAS Blockade Barnett et al. N Engl J Med 2004;351:1952–1961 Renoprotective and antihypertensive efficacy of enalapril and telmisartan • Micardis and enalapril: comparable antihypertensive efficacy – Lower incidence of adverse events with Micardis • Micardis and enalapril reduce proteinuria similarly in patients with moderate renal failure – Fewer adverse events with Micardis • Micardis shown to reduce microalbuminuria and proteinuria • Enalapril stabilized GFR decline in normotensive type 2 diabetics over 5 years Lacourcière et al. Kidney Int 2000 Amerena et al. J Int Med Res 2002 Hannedouche et al. J Renin Angiotensin Aldosterone Syst 2001 11 Estacio et al. Diabetes Care 2000 Study overview • Investigator-led, with independent steering committee • Enrolment initiated in August 1997 • Last patient completed 5-year follow-up in 1Q 2004 • 39 centres in 6 countries: – Denmark – Finland – The Netherlands – Norway – Sweden – United Kingdom Barnett et al. N Engl J Med 2004;351:1952–1961 12 Objectives To compare long-term changes in GFR in patients with type 2 diabetes + hypertension + albuminuria using: – ACEI enalapril 10–20 mg or – ARB Micardis 40–80 mg Barnett et al. N Engl J Med 2004;351:1952–1961 13 GFR and cardiovascular outcomes Estimated event rate (%) 70 60 50 GFR ≥ 75.0 ml/min/1.73 m2 GFR 60.0–74.9 ml/min/1.73 m2 GFR 45.0–59.9 ml/min/1.73m2 GFR <45 ml/min/1.73 m2 40 30 20 10 0 Death from CV causes Reinfarction * Median follow-up 24.7 months CHF Stroke Resuscitation Composite end point Anavekar et al. N Engl J Med 2004 14 Value of GFR • Best overall index of renal function and a powerful predictor of cardiovascular disease • Albuminuria weakly correlates with GFR • Accurate GFR assessment only possible using direct measurement • No previous study of renoprotection with ARBs used direct measurement of GFR to estimate impact on renal function as primary endpoint National Kidney Foundation. Am J Kidney Dis 2002 Hostetter. N Engl J Med 2004 Go et al. N Engl J Med 2004 Anavekar et al. N Engl J Med 2004 MacIsaac et al. Diabetes Care 2004 15 Study design Prospective, multicentre, randomized, double-blind, doubledummy, parallel-group, forced-titration, 5-year treatment Micardis 80 mg* Micardis 40 mg Run-in period E n=250 R enalapril 10 mg enalapril 20 mg* 1 month 1 month *Optional dose-reduction to Micardis 40 mg or enalapril 10 mg after 2 months 59 months Barnett et al. N Engl J Med 2004;351:1952–1961 16 Inclusion criteria • Male or female, 35–80 years • Type 2 diabetes • ACEI for 3 months (ACEI tolerant) • Mild-to-moderate hypertension (BP 180/95 mmHg) • Normal gross renal morphology 12 months • UAER 11–999 µg/min • Serum creatinine 140 µmol/l; HbA1C <12% • GFR 70 ml/min/1.73 m2 (iohexol clearance) Barnett et al. N Engl J Med 2004;351:1952–1961 17 Exclusion criteria • Any condition (other than CVD) that could affect long-term survival of patient • Renal dysfunction not due to diabetes • Single kidney or known renal artery stenosis • NYHA functional class II–IV • Hypersensitivity to study drugs • History of angioedema Barnett et al. N Engl J Med 2004;351:1952–1961 18 Outcomes Primary endpoint • Change in GFR after 5 years Secondary endpoints • Changes in GFR after 1, 2, 3 and 4 years • Changes in UAER and serum creatinine after 1, 2, 3, 4 and 5 years • Incidence of clinical events (ESRD, MI, CVA, CHF) • All-cause mortality • Safety Barnett et al. N Engl J Med 2004;351:1952–1961 19 Statistical analysis • Non-inferiority study • Power calculation: – Assume 25% drop-out rate per year – SD of difference between treatment arms in change in GFR assumed to be 12 ml/min (estimate from literature) – Micardis judged to be non-inferior if lower bound of confidence interval for Micardis-enalapril five-year cumulative difference <10 ml/min/1.73 m2 Barnett et al. N Engl J Med 2004;351:1952–1961 20 Baseline patient characteristics* Males, n (%) Caucasians, n (%) Age (years), mean ± SD Body weight (kg), mean ± SD BMI (kg/m2), mean ± SD GFR (ml/min/1.73m2), mean ± SD UAER (µg/min), median Microalbuminuria, n (%) Macroalbuminuria, n (%) History of CVD, n (%) Micardis (n=120) Enalapril (n=130) 87 (73) 118 (98) 61.2 ± 8.5 90.6 ± 14.9 30.8 ± 4.4 91.4 ± 21.5 46.2 98 (82) 22 (18) 59 (49) 95 (73) 128 (98) 60.0 ± 9.1 90.6 ± 17.4 30.6 ± 5.1 94.3 ± 22.1 60.0 106 (82) 23 (18) 63 (49) *All patients who were enrolled and received at least one dose of study medication Barnett et al. N Engl J Med 2004;351:1952–1961 21 Risk factors at baseline* Micardis (n=120) Enalapril (n=130) Never smoked 41 (34.2) 47 (36.2) Ex-smoker 54 (45.0) 55 (42.3) Smoker 25 (20.8) 28 (21.5) Non-drinker 29 (24.2) 35 (26.9) Average consumption 90 (75.0) 94 (72.3) 1 (0.8) 1 (0.8) Smoking history, n (%) Alcohol history, n (%) Excessive consumption *All patients who were enrolled and received at lest one dose of study medication Barnett et al. N Engl J Med 2004;351:1952–1961 22 Duration of diagnosis at baseline* Micardis (n=120) Enalapril (n=130) 10.0 ± 8.3 8.7 ± 9.2 Median 8.0 5.5 Range 0–34 0–49 9.2 ± 6.6 9.1 ± 6.3 Median 8.0 8.0 Range 0–25 0–37 Hypertension (years) Mean ± SD Diabetes (years) Mean ± SD *All patients who were enrolled and received at least one dose of study medication Barnett et al. N Engl J Med 2004;351:1952–1961 23 Concomitant CV treatment Medication Micardis (n=120) Prior* During† Pts receiving therapy – no. (%) 104 (86.7) ARB 0 ACEI (ex. enalapril‡) 75 (62.5) Enalapril‡ 16 (13.3) Diuretics 25 (20.8) β-blockers 22 (18.3) Ca channel blockers 31 (25.8) Other antihypertensives and heparin 14 (11.7) Aspirin 21 (17.5) Statins 14 (11.7) 102 (85.0) 0 2 (1.7) 2 (1.7) 63 (52.5) 46 (38.3) 54 (45.0) 42 (35.0) 44 (36.7) 51 (42.5) Enalapril (n=130) Prior* During† 122 (93.8) 1 (0.8) 82 (63.1) 27 (20.8) 28 (21.5) 23 (17.7) 33 (25.4) 18 (13.8) 26 (20.0) 22 (16.9) 106 (81.5) 1 (0.8) 0 1 (0.8) 67 (51.5) 49 (37.7) 58 (44.6) 46 (35.4) 54 (41.5) 54 (41.5) * Concomitant medication received for a minimum of 6 consecutive months by any patient who was enrolled and received at least one dose of study medication † LOCF dataset ‡ Patients had to have received an ACEI for ≥3 months prior to enrolment Barnett et al. N Engl J Med 2004;351:1952–1961 24 Patient disposition 250 Telmisartan 120 Enalapril 130 Randomized 20 Discontinued due to adverse events 30 18 Discontinued for administrative reasons 14 5-year completers 82 62 103 38 5-year GFR LOCF GFR 86 40 74 113 25 Barnett et al. N Engl J Med 2004;351:1952–1961 Primary endpoint: GFR after 5 years* Total GFR 100 90 80 70 60 50 40 30 20 10 0 Change in GFR Telmisartan p=NS† Enalapril 0 -5 -10 -15 -20 -25 Telmisartan Baseline -14.8 -17.9 p=NS† Enalapril After 5 years * All patients, LOCF † p = NS, telmisartan vs enalapril Barnett. Presented at ESC 2004 26 GFR change from baseline (LOCF) 10 Enalapril Micardis Change in GFR (ml/min/1.73 m2) 5 0 -5 -10 -15 -20 -25 0 3 2 1 4 5 Year Number of Enalapril patients assessed Telmisartan (carried forward) 103 (0) 86 (0) 110 (22) 99 (23) 113 (23) 102 (21) 113 (30) 102 (31) 113 (39) 103 (41) Barnett et al. N Engl J Med 2004;351:1952–1961 27 Yearly change in GFR* Baseline to Year 1 Year 1 to Year 2 Year 2 to Year 3 Year 3 to Year 4 Year 4 to Year 5 2 Change in GFR (ml/min/1.73 m2) 0 -2 -4 -6 -8 Telmisartan Enalapril -10 * Patients in the study and with data for each yearly timepoint Barnett. Presented at ESC 2004 28 Systolic and diastolic BP* 155 90 Enalapril Micardis Enalapril Micardis Diastolic BP (mmHg) Systolic BP (mmHg) 150 145 140 85 80 75 135 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5 5 Year * All patients, LOCF 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5 5 Year Barnett et al. N Engl J Med 2004;351:1952–1961 29 Secondary endpoints at 5 years* Endpoint Micardis enalapril Difference P +8.84 +8.84 0.00 NS n 116 128 UAER – ratio‡ 1.03 0.99 1.04 NS* n 115 125 Mean change serum creatinine (µmol/l) UAER=urinary albumin excretion rates; NS=not significant; * All patients, LOCF † Determined from the logarithm of the individual change from baseline ‡ Ratio of treatment differences. Barnett et al. N Engl J Med 2004;351:1952–1961 30 Safety* Micardis Enalapril 115 (95.8) 61 (50.8) 20 (16.6) 2 (1.6) 6 (5.0) 1 (0.8) 6 (5.0) 2 (1.7) 9 (7.5) 9 (7.5) 6 (5.0) 3 (2.5) 130 (100.0) 57 (43.8) 30 (23.1) 0 (0.0) 6 (4.6) 3 (2.3) 6 (4.6) 2 (1.5) 7 (5.4) 6 (4.6) 6 (4.6) 2 (1.5) n Total AEs over 5 years Serious AEs Discontinuation due to AE Due to worsening of study disease Due to worsening of other disease Due to cough CVA Creatinine ≥200 µmol/l) CHF Non-fatal MI Deaths Due to CV event AE= Adverse event; *All patients who were enrolled and received at least one dose of study medication % n % Barnett et al. N Engl J Med 2004;351:1952–1961 31 Discussion – GFR • Age-related decline of GFR in healthy individuals is ~1 ml/min/1.73m2/year (NHANES III) • In diabetics with proteinuria without intervention, declines at 10–12 ml/min/1.73m2/year • In DETAIL, the initial steep decline stabilized by Micardis and enalapril to ≈2 ml/min/1.73m2/year after Year 3 National Kidney Foundation. Am J Kidney Dis 2002 Parving et al. Semin Nephrol 2004 Brenner. Kidney Int 2003 32 Micardis: stabilisatie nierfunctie 90 GFR (ml/min/1.73 m2) 80 70 60 50 40 No Treatment Ageing 30 20 Threshold for ESRD 10 0 Baseline 1 2 3 Year * All patients, LOCF 4 5 Barnett et al. N Engl J Med 2004;351:1952–1961 Parving et al . Semin. Nephrol. 2004 33 Micardis: stabilisatie nierfunctie 90 GFR (ml/min/1.73 m2) 80 70 60 50 Micardis No Treatment Ageing 40 30 20 Threshold for ESRD 10 0 Baseline 1 2 3 Year * All patients, LOCF 4 5 Barnett et al. N Engl J Med 2004;351:1952–1961 Parving et al . Semin. Nephrol. 2004 34 Renoprotective effects of ARBs: GFR decline in DETAIL, IRMA 2, IDNT and RENAAL RENAAL* IRMA2† IDNT† DETAIL† 3.4 years 2 years 2.6 years 5 years Losartan 100 mg Irbesartan 300 mg Irbesartan 300 mg Micardis 80 mg GFR decline (ml/min/1.73m2/year) 0 -1 -2 -3 -4 -5 -6 * Median † Mean -3,7 -4,4 -5,7 -5,5 Parving et al. N Engl J Med 2001; Brenner et al. N Engl J Med 2001 Lewis et al. N Engl J Med 2001; Barnett et al. N Engl J Med 2004;351:1952–1961 35 Discussion – mortality • Over 5 years, expected mortality rate in older type 2 diabetics is ~35% (micro) and ~50% (macro) • ARBs reduce ESRD, but not yet demonstrated significant reductions of CV endpoints in type 2 diabetes with nephropathy (IDNT, RENAAL) • ACEIs reduce CVD in type 2 diabetes (HOPE), but not yet demonstrated in nephropathy • In DETAIL, there were only 6 deaths (~5%) in each group, half of which were due to CV events Valmadrid et al. Arch Intern Med 2000 Lewis et al. N Engl J Med 2001 Brenner et al. N Engl J Med 2001 HOPE Investigators. Lancet 2000 36 Discussion – safety • DETAIL inclusion criteria required all patients to be tolerant of ACEIs • Therefore, no major differences in adverse events between Micardis and enalapril were anticipated • Nevertheless, there were fewer withdrawals due to adverse events with Micardis • This is in line with previous studies, in which Micardis showed a safety profile superior to enalapril Amerena, et al. J Int Med Res 2002 Hannedouche, et al. J Renin Angiotensin Aldosterone Syst 2001 37 Summary • First long-term study in patients with hypertension and early-stage type 2 diabetic nephropathy to compare ARBs and ACEIs • Using GFR, the most reliable indicator of kidney function and important predictor of cardio vascular disease • Micardis is comparable to enalapril in reducing GFR decline and providing renoprotection in patients with type 2 diabetes and nephropathy • Very low mortality rate (5%) 38 Conclusions • Results in accord with the proven renoprotective profile of ARBs and ACEIs • Consistent with emerging data supporting clinical equivalence of angiotensin-II–blockers and ACEIs in various states of high cardiovascular risk. • Micardis is therefore a valid choice for first-line treatment of hypertensive patients with type 2 diabetes and earlystage nephropathy 39