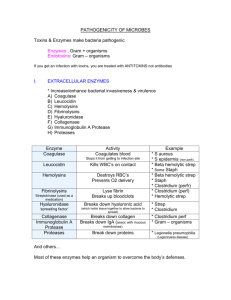
Bacterial Toxins
advertisement

Mechanism of Pathogenicity Pathogens & Disease Pathogens are defined as microbes capable of causing host damage. When host damage reaches a certain threshold, it can manifest itself as a disease. The evolution of an infectious disease in an individual involves complex interactions between the pathogen and the host. PATHOGENICITY & VIRULENCE Pathogenicity – the ability to cause disease by overcoming the defenses of the host Virulence – the degree or extent of pathogenicity Virulence factors – the various traits or features that allow or enhance the microorganism’s ability to cause disease. These take may forms and include: adhesion organelles, toxin production, evasion of the host’s immune response, resistance to antibiotics, ability to invade host tissues MECHANISMS OF PATHOGENICITY Portal of Entry Adherence Penetration/invasion of host defense Damage to host cell PORTALS OF ENTRY To cause disease, most pathogenic bacteria must gain access to the host including skin and mucus membranes cuts, surgical procedures, catheters, etc may allow bacteria entrance into the host Normal skin flora, including Staphylococcus aureus and Staphylococcus epidermidis, can enter through these barriers and establish an infection PORTALS OF ENTRY Many pathogens have preferred portals of entry that are necessary for disease production If they gain entrance via another portal, disease may not occur Salmonella typhi produces disease when swallowed but not if rubbed on the skin Streptococci that are inhaled can cause pneumonia but, if swallowed, generally do not produce disease Bacillus anthracis can initiate disease from more than one portal of entry (skin inoculation, GI, respiratory) ADHERENCE. Means attachment A necessary step in pathogenicity Attachment between pathogen and host is accomplished by means of adhesins or ligands. Most adhesins of microbes are glycoproteins or lipoproteins ADHERENCE The term pili (pilus) is also used to bind the host cells Gram positive organisms use other structures for adhesins (lipoproteins, etc). Streptococcus pyogenes uses lipoteichoic acid to bind to epithelial cells Once attached to target cells, many bacteria can then invade the cell ADHESINS ARE VERY DIVERSE. S. mutans plays a key role in tooth decay attaches to the surface of teeth by its glycocalyx E. coli have adhesins on fimbriae that adhere only to specific kinds of cells INVASION Not all bacteria are invasive. Invasive organisms attach and enter host cells by a number of mechanisms: Production of surface proteins called invasins Production of enzymes: collagenase which breaks down collagen in connective tissue hyaluronidase which breaks down hyaluronic acid that holds cells together (particularly connective tissue cells) Coagulase which converts fibrinogen to fibrin producing a clot (may be protective against phagocytes) Kinases which can break down clots decreasing the isolation of bacteria in clots (spreading effect) HOW BACTERIA DAMAGE HOST CELLS. Direct damage The production of Toxins Types of toxins: Exotoxins and Endotoxins. Bacterial Toxins Many different types of toxins Exotoxins Endotoxins Toxins are are not required for growth Genes for toxins are usually on plasmids EXO and ENDOTOXINS. EXOTOXINS. Produced inside some bacteria as part of their growth and metabolism and released into the surrounding medium Are proteins, and many are enzymes Most bacteria that produce exotoxins are grampositive The genes for most exotoxins are carried on bacterial plasmids or phages. Neurotoxin. Target the nervous system, and can interfere with normal nerve impulse transmission, e.g. C. tetani, C. botulinum. ENTEROTOXINS. Affect cells lining the gastrointestinal tract. E.g. V. cholerae, C. difficile. ACTION OF AN EXOTOXIN. Bacterial Exotoxins Exotoxins Initial location outside cells Transported into host cells Alter host cell physiology and metabolism Typical A – B toxins AB toxin enters cells via: 1) Receptor mediated endocytosis 2) Fusion of vesicle with lysosome 3) Acid environment of lysosome reduces disulfide bonds and releases A into cell 4) A has various cellular activities Corynebacterium diphtheriae Corynebacterium diptheriae Produces AB exotoxin Gram positive rod Significant cause of mortality until 1950s Common location upper respiratory tract Clostridium botulium Clostridium botulinum Produces AB exotoxin Produces irreversible muscle relaxation Flaccid paralysis Symptoms result entirely from toxin Anaerobic gram + rod Usually ingested in contaminated food Does not involve fever or sepsis Patients die of paralysis and respiratory failure Normal Neuronal Signaling Mechanism of Action of botulinum toxin NOTABLE EXOTOXINS. Diphtheria toxin. Erythrogenic toxins. Botulinum toxin. Tetanus toxin Vibrio Enterotoxin. Staphylococcal Enterotoxin. . Bacterial Endotoxins Endotoxins Toxin is not internalized Toxin is located on outside of microorganisms (Part of the outer portion of the cell wall of bacteria) LPS of gram – bacteria Lipoteichoic acid or gram + bacteria Only toxic at high levels Liposaccharide Exert their effects when the gram negative bacteria dies and their cell wall undergo lysis, thus liberating the endotoxin(e.g use of antibiotics) All endotoxins produce the same signs and symptoms Endotoxins can also induce miscarriage. Mechanism of Action of Endotoxins Endotoxins bind to Receptors on Macrophages Neutrophils Lymphocytes Proteins of complement Complement is a group of proteins which circulate at constant levels in the blood When activated complement is a powerful tool against invading pathogens Increased inflammation Bacterial Endotoxins Endotoxins Host cell receptors (TLR) bind to components of pathogen Pathogen associated molecular patterns PAMPS LPS – gram - cell walls Flagella Lipoteichoic acid – gram + cell walls Signal transduction pathways begin to make a cellular response Production of cytokines Bacterial Exoenzymes Enzymes secreted by bacterial cells into the extra cellular matrix of host Membrane Damaging Toxins Enzymes which act in the extra cellular matrix Enzyme destruction of host cell membranes Lyse red blood cells Membrane pore forming complex Spreading factors Breaks down connective tissue Attacks blood clots Enzymes which subvert drug therapy in patients Penicillinase Some Common Exoenzymes α toxin Pore forming toxin Common in Staphylococcus aureus Destroy red blood cells Streptolysins – group of hemolysins excreted by Streptococcus Streptokinase Attacks fibrin clots From Streptococcus pyogenes Hyaluronidase Hemolysins Breaks down hyaluronic acids in connective tissue Similar function for Collagenase Elastases DNase DNA is viscous Thins pus (DNA & debris) released from WBC Clostridium perfringens Clostridium perfringens Ananerobic gram + spore forming rod Widely distributed in nature Entry of spores by traumatic injury Not highly invasive so it requires exoenzymes for a supportive growth environment Exoenzymes Lecithinase lipase c – major toxin Lyses mammalian cells indiscriminately Substrate is phophatidylcholine Collagenase & hyaluronidase DNAase