Lesson4_Host-Microbe interactions
advertisement

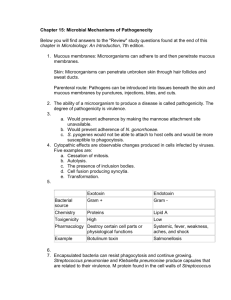
Immunology- 2011 Lesson Outline Infectious disease 2. Pathogenicity 3. How does host and pathogen interact? 4. Microbial Virulence Factors Antiphagocytic factors Exotoxins Endotoxins 1. Infectious disease occurs as the result of interaction between pathogen and the host Infections begin at some surface of the host- skin, conjunctiva, internal surface of the mucous membrane of respiratory tract, intestine etc. Many pathogens can selectively attach to particular host surface. pathogenic organism penetrates the body surface and gain access to the internal tissues Infections of microorganism becomes localized, growing near its point of entry into the body. Some pathogens cause generalized infection and microorganisms become widely distributed and grows through out the body. Pathogen capable of growth within the cell of the host disrupts the normal physiological process. What damages the body cells? Toxins by microorganisms. Virulence factors - combat various defense mechanisms of the host. what is pathogenicity? Is the capability of a microbial species to cause disease. various strains of a pathogenic species may differ with regard to their degree of pathogenicity and with regard to their virulence. highly virulent - only a few bacterial cells 2. less virulent - larger numbers of cells 3. avirulent - incapable of causing the disease even when large numbers. 1. what are attenuated strains? When virulent strains of many pathogens are repeatedly cultured on laboratory media or grown in vivo in hosts other than their normal hosts , they lose their virulence. widely used as vaccines to elicit immunity to various diseases. How to measure the virulence of an organism? By determining its LD50 dose for a laboratory animal. LD50 - defined as that number of organism which when administered to number of laboratory animals, kills 50 percent of them. LD100 Infection Represents the most intimate way in which a microorganism may cause disease. Host is invaded and multiply in close association with host’s tissue. Note: not all diseased caused by microorganisms are infections. Process of infection Pathogen must accomplish the following: It must enter the host It must metabolize and multiply on or in the host tissue It must resist host defenses It must damage the host. Process of Host pathogen interaction 1. Microbial adherence 2. Penetration/ entrance into the body 3. Events of infection following penetration 4. microbial virulence Microbial adherence first step in initiation of infection is by adherence of pathogens to some surface of the hosts. Attachment is selective. various pathogens attaches to certain tissues. Mode of attachment is not yet understood, for pathogenic fungi & protozoa. For bacteria: Neisseria gonorrhea - epithelial layer of human cervixpili. E. coli - mucosal lining of the intestine- pili. Streptococcus pyrogenes- epithelial cells by means of cell wall protein called M-protein. Virus: Influenza virus particle is studded with haemagglutinin spikes- to specific mucoprotein receptors on the surface of the host cell. Polio virus - to lipid and glycoprotein containing receptors on host cells. Penetration/entrance of pathogen Microorganism may merely multiply on the epithelial surface & cause damage without penetration into the body. Example: V. cholerae, causative agent of the severe diarrheal disease known as cholera, multiply on the epithelial layer of the small intestine where it produces a toxin that cause the loss of fluid from the epithelial cells and kills the cells. Penetration may be achieved not only actively but also passively . Actively - by the adherence and penetration mechanism of the pathogens itself. Passively - by mechanisms having nothing to do with the properties of the microorganism. portals of entry are the respiratory tract and gastrointestinal tract Any mechanically caused breach on the body surface can introduce pathogen directly . Events in Infection following penetration the microorganism multiplies resist the defense mechanism of the host, and begin to cause the tissue damage. may simply grow in the tissue in which it find itself, causing a localized infection Types of Infections: Example: Staphylococcous aureus infection where characteristic lesion is an abscess . a walled off cavity is formed in the tissue containing staphylococci and numerous blood cells (that collectively form a pasty mass called pus), and dead, disintegrating tissue cells that have been killed by the toxins elaborated from the staphylococci. the organism may not remain localized but may spread through the tissues. Example: An anaerobic bacterium C. perfringens causes the wound infection gas gangrene. As it grows, it elaborate toxins that kills some of the surrounding healthy tissues. dead tissues becomes anaerobic can support the growth of most Clostridia, which in turn elaborate more toxins. kills more tissues and allow the organism to spread further. Other Factor is the production of large amounts of hydrogen gas by the bacteria Hydrogen gas separates connective tissue sheaths from muscle tissue forming a space rapidly get filled in by Clostridia containing fluid. Bacteria invade the entire length of muscles. Amputation of affected limbs is often the only way to stop the spread of C. perfingens to the rest of the body Infection of lymphatic system microorganisms can spread form the initial site of infection to the lymphatic system. carried by lymphatic vessel to lymph nodes. channel within a node is lined with cells called Macrophages, can engulf and destroy the bacteria that enter the lymph node (Phagocytosis). lymph nodes removes nearly all of the bacteria that enter it, and it may become inflamed enlarged sore when infected called a bubo. In bubonic plague, such swollen lymph nodes are particularly prominent- exhudate filled with plague bacilli. Infection of blood by passive or active means, a pathogenic microorganism enter a blood capillary or venule there by gain direct access to the blood vascular system, cause in a Bacteremia ( presence of bacteria in the blood). carried to various parts of the body and cause localized infections. bacteria may actively multiply in the blood stream and produce toxic products and a condition known as septicemia. Septicemia infections range from chronic to acute. Example: anthrax a disease of animals and sometimes humans number of Bacillus anthracis organism may often exceed the number of erythrocytes in the blood. Microbial Virulence Factors: Antiphagocytic factors Virulence: degree of pathogenicity exhibited by a strain of microorganism. The virulence of many pathogenic bacteria is influenced by the presence or absence of a non-toxic polysaccharides material composing the capsules surrounding the cells. capsules can prevent the engulfment and destruction of the bacteria by the phagocytic defense . Capsular polysaccharides can be isolated in pure form. capsular polysaccharides of pneumococcal are injected into humans, stimulate the productions of antibodies protect against the type of Pneumococcus from which they were obtained. Some antiphagocytic factors made by pathogenic bacteria are not capsules but like capsules that are located on the outer surface of the bacterial cell wall is called M-protein Eg. M protein of S. pyogenes Toxins produce poisonous substances known as toxins. potency can be expressed in most precise terms of : A. LD50 -kills 50% of test animals that are injected with toxins. B. MLD minimum lethal dose or LD100 dose-kills 100% of test animals. Toxins are of two types: 1. exotoxins and 2. endotoxins. Exotoxin Toxic proteins that are secreted by living microorganisms have extraordinarily high potency with minute amounts being needed to kill animals. Not all exotoxins are lethal and merely cause unpleasant effects. Example: S. aureus produces toxin which when ingested by a human in quantities as little as 1μg gives rise to severe nausea and vomiting (Staphylococcus food poisoning). Types of Exotoxins Toxoids Exotoxin lose their toxicity when treated with formaldehyde but antigenic properties are retained . In this form they have the ability to stimulate the production of antitoxins (antibodies that react with toxins and neutralize them) in the body of a host animal- – called Toxoids. important in protection of susceptible host from disease caused by bacteria that produce exotoxin. Example: Toxoids are widely used as vaccines for immunization against tetanus and diphtheria. The ability of the bacteria to produce such exotoxin (toxigenicity) is due to a Chromosomal gene. Mechanism of action of Exotoxin Botulism Toxin In botulism toxin binds to the axon near the neuro muscular junction prevents the secretion of acetylcholine; thus the muscle cannot contract. If this paralysis extends to the muscles of the chest and diaphragm, death by respiratory may result. Endotoxins are lipopolysaccharides located in the outer membrane of the cell wall of many Gram Negative bacteria. All endotoxins exhibit similar pharmacologic effects. They are: pyrogenicity 2. blood change and 3. shock 1. 1. Pyrogenecity: Is the ability to cause change in the body temperature. In human it cause an increase in body temperature (i.e a fever response). Indirect effect: chemical agent endogenous pyrogen released from the blood leukocytes under the influence of endotoxins that causes the temperature change. pyrogen affects the hypothalamus for the brain which regulates body temperature. Blood changes: 1. 2. endotoxin damage blood platelets (thrombocytes) cause an increase in the permeability of blood capillaries causing them to leak the fluid portion of the blood . sometimes even whole blood (Hemorrhage) and these effect can cause serious change in the circulation and blood pressure. Shock When gram negative bacteria are present in large numbers or when endotoxin is injected intravenously, severe shock may occur as evidenced by: decreased blood pressure Feeble rapid pulse Decreased respiration and sometime unconsciousness. High dose can result in circulatory collapse and death. Other Virulence factor: 1.Coagulase Staphylococcus aureus produce an enzyme commonly called coagulase . reacts with an activator in plasma to cause clotting. 2. Deoxyribonuclease (DNase) an enzyme produced by S. pyogenes, S. aureus, C. perfringens and other pathogens. Its ability to destroy DNA would seem to indicate that it is a formidable cytotoxin. 3. Protein A Present on the cell wall of S. aureus has the ability to bind the antibodies regardless of their specificity. The antibody molecules are distorted so that their binding site for complement ( C) is exposed. 4. Hydrogen peroxide and Ammonia Bacteria of genera Mycoplasma and Ureaplasma adhere firmly to the epithelial tissue of the respiratory or urogenital tract. They secrete toxic by product of their metabolism H2O2 and NH3. Accumulate locally to high concentration thereby damaging the epithelial cells. 5 Microbial iron chelators aerobic microbial pathogens which has the ability to compete with a host for available iron has considerable bearing on microbial virulence. Aerobic or aero tolerant organisms are continually faced with the difficulty of obtaining enough iron for growth, required for biosynthesis of iron-containing enzymes such as cytochromes and catalase. Most of the iron that is available for aerobic or aero tolerant organisms is present in the oxidized ferric form, which is extremely insoluble. Aerobic organism have had to evolve ferric iron-binding compounds in order to solubilized and take up ferric iron. The iron-binding compound formed by microorganisms is termed siderophores. These generally belong to two major classes the phenolates and the hydroxalates. The role of microbial siderophores in virulence is to compete with the host for available iron. The host, being aerobic, also possesses iron-binding compounds, proteins known as Lactoferrin and transferrin, which can limit the amount of iron available to an invading pathogen.