Oxazolidinones for Tuberculosis
advertisement
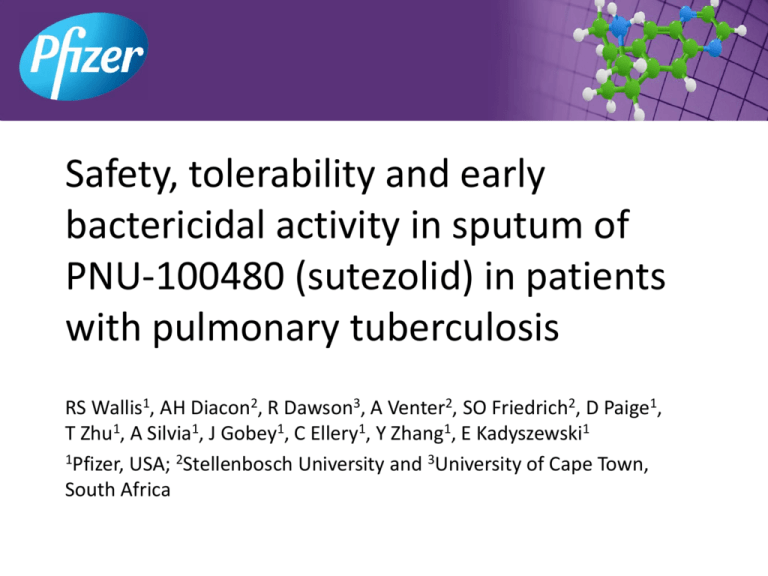
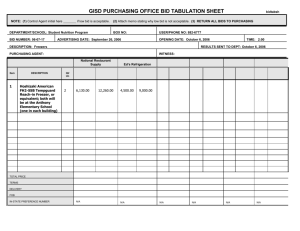
Safety, tolerability and early bactericidal activity in sputum of PNU-100480 (sutezolid) in patients with pulmonary tuberculosis RS Wallis1, AH Diacon2, R Dawson3, A Venter2, SO Friedrich2, D Paige1, T Zhu1, A Silvia1, J Gobey1, C Ellery1, Y Zhang1, E Kadyszewski1 1Pfizer, USA; 2Stellenbosch University and 3University of Cape Town, South Africa PNU-100480 (sutezolid) • Oxazolidinone antimicrobial – Sulfur-containing linezolid analog with an active sulfoxide metabolite – Bind 23S RNA and inhibit microbial protein synthesis – No cross resistance, neither inhibits nor induces CYP3A4 • Preclinical findings – Superior bactericidal activity vs. linezolid in mouse and whole blood TB models regardless of LZD dose or concentration – Earlier sterilization (1-2 months) when combined with standard TB drugs • Phase 1 findings – Doses to 600 mg BID generally safe and reasonably well tolerated to 28d – No significant safety signals, incl. hematology, biochemistry, QT • Potentially can address 4 major unmet medical needs in TB – DR, HIV, DS, suspected DR-LTBI • The present phase 2a study is its first in TB patients Study inclusion criteria • Men and women aged 18-65 years • Pulmonary tuberculosis – CXR consistent with pulmonary tuberculosis – Positive sputum acid-fast smears – Culture or molecular confirmation of drug-susceptible Mtb • Either HIV-1 uninfected, or HIV-1 infected with CD4 T cell counts >350/mm3 and not currently receiving ART • Reasonably normal renal, hepatic, metabolic function • Willing to provide written informed consent according to ICH guidelines 3 Study exclusion criteria • Significant hemoptysis • TB treatment within the preceding 6 months – Or positive test for urinary isoniazid metabolite at the time of screening • Treatment with MAO inhibitors, tricyclic antidepressants, or adrenergic agonists such as pseudoephedrine or phenylpropanolamine within the preceding 7 days – Due to potential MAO-B activity 4 Randomization and treatment • Subjects were recruited at 2 sites in South Africa, and were randomly assigned in blocks of 7 to: – PNU-100480 600 mg BID – PNU-100480 1200 mg QD – Fixed dose combination tablets consisting of isoniazid, rifampin, ethambutol, and pyrazinamide (Rifafour© e275) • Neither subjects nor investigators were blinded to assigned treatment • Treatment duration was 14 days – After which all patients commenced standard TB treatment – Final safety evaluation was on day 42 5 Subject characteristics Number of subjects Age (years, mean±SD) Sex (male/female) Race (Black/other) Weight (kg, mean±SD) Height (cm, mean±SD) BMI (kg/m2, mean±SD) Baseline log CFU/ml (mean±SD) 600 mg BID 25 32.3±9.0 20/5 11/14 54.6±6.5 167.4±8.2 19.6±2.9 6.88±1.11 Treatment arm 1200 mg QD 25 34.1±11.7 20/5 8/17 51.1±6.7 167.0±6.1 18.3±1.8 6.91±1.20 HREZ 9 33.8±11.8 7/3 3/6 51.3±7.5 166.5±11.8 18.4±0.5 7.22±0.71 Safety and tolerability Subjects evaluable for adverse events Number of adverse events Subjects with adverse events Subjects with serious or severe adverse events Subjects discontinued due to adverse events Subjects with dose reduced or temporary discontinuation due to adverse events 600 mg BID 25 23 (44%) 15 (60%) 1200 mg QD 25 17 (33%) 12 (48%) 9 12 (23%) 5 (56%) 1 0 0 0 0 0 0 0 0 HREZ 7 Adverse events (all causes) PNU 600mg BID (n=25) PNU 1200mg QD (n=25) CARDIAC GASTROINTESTINAL GENERAL INFECTIONS INVESTIGATIONS METABOLISM MUSCULOSKELETAL NERVOUS SYSTEM PSYCHIATRIC RENAL AND URINARY REPRODUCTIVE RESPIRATORY SKIN TOTAL Mild 0 2 0 1 0 2 2 2 0 0 0 0 6 15 Mod 0 1 0 1 4 0 0 0 0 0 0 0 2 8 Sev Mild Mod 0 1 0 No effect on 0 QTc0 interval0 0 -4.2±141 ms 1 BID: ALT increase 0 -3.1±12 0ms 0 QD: 2-3x 0 ULN 0 3 0 0 0 0 1 0 0 2 0 0 1 1 0 0 0 0 0Hemoptysis 0 1 1Day 28 1 0 2 1 1 11 7 Sev 0 0 0 0 0 0 0 0 0 0 0 0 0 0 HREZ (n=9) Mild 0 2 1 1 0 0 2 0 0 0 1 1 1 10 Mod 0 0 0 0 0 0 0 0 0 1 1 0 0 2 Sev 0 0 0 0 0 0 0 0 0 0 0 0 0 0 Early Bactericidal Activity log CFU 0 • Both PNU dosing schedules resulted in significant log CFU reductions from baseline over the 14 day period of treatment. – 600 mg BID: -0.09 log/d, 90% CI -0.06 to -0.11 – 1200 mg QD: -0.07 log/d, 90% CI -0.04 to -0.09 • A trend was apparent toward superior responses with BID dosing -1 -2 1200 QD 600 BID HREZ -3 0 2 4 6 8 10 12 14 day Shading indicates 90% confidence interval by mixed effects model repeated measures analysis Treatment-emergent ALT increases 300 ALT (U/l) • 7/50 PNU-treated 250 TB patients (14%) 200 • No apparent pre150 disposing factors • ALT increased to 100 2-3x ULN, accom50 panied by smaller 0 AST increases 0 7 14 21 • No changes in bilirubin or AP day • No cases met Hy’s Law criteria • All were asymptomatic and resolved quickly 28 35 42 10 Glutathione (GSH) depletion hypothesis • Drug-induced liver injury is common in TB (10-20%) – HRZ all are implicated • GSH, which ordinarily protects against oxidative injury, is decreased in TB – GSH is decreased in TB animal models and in TB patients – Palanisamy, PLoS ONE 2011, and Venketaraman, Microb Path 2008 – Apparently is consumed to protect host cells from the cellular antimicrobial host response (peroxides, superoxides, NO) – Lowest levels are in TB patients with drug-induced liver injury – Chowdhury, Indian J Gastro 2001 • Liver injury due to HRZ can be prevented by supplementation with N-acetylcysteine (NAC) – (Baniasadi, Eur J Gastro Hepatol 2010) 11 Summary • Treatment with PNU-100480 at doses of 600 mg twice daily or 1200 mg once daily for 14 days resulted in significant reductions in sputum bacillary burden – A trend toward superior bactericidal effect was apparent when given twice daily • Both dosing schedules were generally safe and relatively well tolerated • New TB regimens containing PNU-100480 can potentially address major unmet medical needs in TB treatment Contact: robert.wallis@pfizer.com Questions? • • • • • LZD NAC MPS Parent – metabolite Proposed clinical plan EBA comparison with linezolid Drug Dose and duration* Linezolid 600 mg BID and QD days 0-7 mean log/d Study (90% CI) -0.082 Dietze, (-0.054 to -0.110) AJRCCM 2008 Sutezolid 600 mg BID days 0-6 -0.146 (current study) (-0.102 to -0.191) * Both LZD doses appeared equivalent, and here are combined to increase precision. LZD data indicate effects over the entire treatment period (7 days). Sutezolid data were limited to days 0-6 for comparison, as log CFU data were not collected on day 7. Caution is warranted when comparing with historical data. Human Pulmonary Tuberculosis Extracellular infection Intracellular infection • Cavities contain large numbers of log phase bacilli that can give rise to resistance • Inadequate treatment results in failure • Eradication is termed bactericidal activity • Granulomas contain small numbers of semi-dormant bacilli that can give rise to persistence • Inadequate treatment results in relapse • Eradication is termed sterilizing activity Plasma concentration/MPS IC50 PNU-100480 Linezolid 5 Fold MPS IC50 Fold MPS IC50 5 4 3 2 1 0 4 3 2 1 0 0 6 12 18 Hours 1200 mg QD 600 mg BID 300 mg BID 100 mg BID 24 0 6 12 18 Hours 600 mg BID 300 mg QD Wallis, AAC 2011 24 Intracellular bactericidal activity ex vivo whole blood culture 0.4 LZD PNU log/d 0.2 0.0 -0.2 -0.4 -0.6 0 1 2 Concentration ( g/ml) 3 Linezolid, sutezolid & metabolites PNU-101244 Sutezolid PNU-101603 Linezolid Linezolid Sutezolid PNU-101603 PNU-101244 MIC (mg/ml) 0.5 MPS IC50 (mg/ml) 5.5 Plasma conc vs. parent - Critical activity 0.25 0.5 0.5 15.5 4.4 5 5X 0.1X Intracellular Extracellular - 2-mo culture status highly related to relapse-free cure 3 A Location Treatment Africa Hong Singa- India modification Kong pore relapse rate (log ratio) 2 1 T added Z added R added S added IP shortened 3x/wk 2x/wk S removed, IP lengthened 0 -1 -2 E->Z Wallis, Lancet ID 2010 -3 -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) Intensive phase shortened relapse rate (log ratio) 3 Intermittent treatment 3 B 2 Pyrazinamide added 3 C 2 1 Streptomycin added 3 D 2 1 Rifampin added 3 E 2 1 1 0 0 0 0 0 -1 -1 -1 -1 -1 -2 -2 -2 -2 -2 -3 -3 -3 -3 -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) F 2 1 -3 -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) -0.2 0.0 0.2 0.4 2-month conversion rate (log ratio) Sutezolid Clinical Plan Compound 1 Ph1 EBA* Compound 2 Ph1 EBA* Compound 3 Ph1 EBA* Compound 4 Ph1 2-mo regimen selection trial: PNU-100480 (U) Bedaquiline (J) plus one of: SQ109 PA-824 Clofazimine Imatinib Rifabutin/PZA Confirmatory trial: Selection of regimens & durations Novel DR regimen Novel DS regimen (UJRbZ) vs. SOC 2-mo status 2-mo status 3 yrs Nonrelapsing cure Adaptive licensing / Accelerated approval EBA* XDR *or alternative MDR Outcomes Registry DS NAC Supplementation Prevents TB Drug-Induced Liver Injury AST ALT 300 T Bili 200 2.5 2.0 150 mg/dl U/l U/l 200 100 100 50 0 1 2 1.0 0.5 0 0 1.5 0.0 0 Week 1 2 Week HREZ HREZ+NAC 0 1 2 Week 12/32 0/28 P =.002 Baniasdai, Eur J Gastro Hepatol 2010 23