3 - Becker's Hospital Review
advertisement

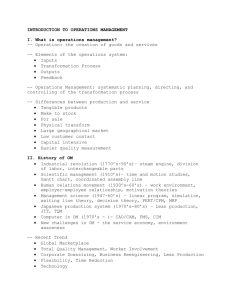
Lake Health’s Lean Journey Innovative Improvement for Independence A little bit about us Cleveland Ohio • • • • • • Team Members = 3,000 Inpatient Beds = 270 Adult Admits = 17,000 Births = 1,900 Surgical Cases = 14,000 ER Visits = 76,000 Presentation Roadmap 1. Reason for Action: Why did we decide to embark on this journey? 2. Initial State: Where were we when we started? 3. Target State: Where do we want to be in 3…5…10 years down the road? 4. Identifying Gaps: What are the major barriers that must be overcome? 5. Solutions: What needed to be done to overcome those barriers? 6. Rapid Experiments: Early successes/failures along the way? 7. Completion Plan: Getting started on our journey! 8. Confirmed State: Have we moved the dial? 9. Insights: Lessons learned 1. Reason for Action What is LEAN? Toyota Business System The practice and process of identifying and removing waste Waiting Unnecessary Motion Defects The concept and practice of continuous improvement The power of respect for people (Front line decisions) 1. Reason for Action Organizations Practicing LEAN? 3M Boeing Avery Dennison Dow Chemical Virginia Mason Mayo Clinic ThedaCare General Electric Denver Health Ford Motor Company Stanford Hospital & Clinics Sears Lake Health!! GlaxoSmithKline GEICO US Army, Navy, Air Force and Marines 1. Reason for Action Why did we decide to embark upon this journey? Desire to remain an independent, community-based health system Recognition that the status quo or incremental changes in quality, cost and patient experience would not be sufficient to achieve goals Require a shared disciplined approach to innovative improvement, that will transform the way we do business Success of the transformation will ultimately depend on the participation of all team members, volunteers and physicians 1. Reason for Action May 14-16, 2012 Leadership Retreat 7 2. Initial State Where were we when we started? Operating in a dynamic/competitive market Desiring to improve clinical quality and patient experience. Needing to extend focus beyond acute episodic care to continuum of care Reimbursement not keeping pace with increasing expenses Mediocre team member engagement Average community perceptions 3. Target State Where do we want to be in 3…5…10 years down the road? Improved patient and family value through: higher quality lower cost improved safety Waste eliminated from processes Instill a culture of continuous improvement 4. Identifying Gaps What are the major barriers that must be overcome? Availability of space Staff Support Budget Structure “Program of the Month” Conflicting Priorities 5. Solutions Deciding where to begin… Identify potential areas to begin Identify the criteria for areas selected Number of patients touched Opportunities for improvement Highest impact on the organization Select ones that complement each other 5. Solutions What needed to be done to overcome those barriers? If We: Then We: Identify and harvest value streams #7, #8, Metrics will improve Utilize A3 thinking #1, #2, We will hardwire PI Develop a lean office #1, #3, #6, #7 Track results to True North metrics #1, #8, What gets measured gets results Create steering teams for guidance (enterprise, value streams) #2, #4, #6, #7, #8 Provide coaching to leadership team #1, #2, #6, #7 Have leaders participate on RIE’s, every year #1, #5 Communication Plan #1, #2, #5, #7, #8 Physician engagement #1, #2, #5, #7, #8 Develop common terms/language #1, #2, #3, #4, #5, #6, #7, #8 5. Solutions Addressing Space/Staffing 5. Solutions Addressing Structure Define Measure Pre-work Analyze Improve Sustain RIE Follow-up Lean overview Review Pre-work Educate Observations Validate observations Tweak final changes Stakeholder analysis Brainstorm solutions Sustain new process RIE planning Try-storm solutions Continuously improve through MDI Validate improvements 5. Solutions Addressing Structure RIE – Change Based on Knowledge of the World’s Greatest Experts Those doing the work Monday Tuesday Wednesday Thursday Friday Current Condition Gemba Waste Observation Waste Analysis Map Future State Generate Solutions Run Rapid Experiments Problem Solving Run New Process Document Standard Work Report Out 6. Rapid Experiments Early successes/failures along the way? Nurse to Nurse Handoff Initial: • Average time from ED to inpatient bed 79 minutes and up to 250 • ED staff took patient to inpatient unit then had to find the nurse Solution: • Inpatient nurses pull the patients from the ED within 15 minutes • Developed new clinical summary screen to facilitate face to face handoff Benefit: • Reduced time to inpatient bed from 79 minutes to 40 • Improved perception of care from patients • Improved quality and safety of hand off. Second Pass improvements Solution: • Time reduced an additional 20 minutes! 6. Rapid Experiments Early successes/failures along the way? Periops Initial: • Increasing Cost/UOS • Different patient types cared for by same staff • Causing uneven patient flow through SDS • Need to expand SDS area to support patient volume $3M project Solution: • Developed flow/standard work based on procedure • Identified specific locations in SDS for each patient type Benefit: • Improved flow avoided need for additional SDS beds. • Saved $2.5M in capital. 6. Rapid Experiments Early successes/failures along the way? Physician First Initial: • Median time Door to Doc was 40 minutes • Protocol Care creating excessive ordering • Patient satisfaction for arrival less than desired Solution: • Implement Physician first concept at peak volume times • Triage by physician • Earlier implementation of care Benefits: • Patient satisfaction with arrival improved by 57% • Door to Doctor time decreased by 48% 7. Completion Plan Never complete… Review the System-wide Transformational Plan of Care Integrate into System-wide plan. Looking to expand to new areas within the system Expanding the number of facilitators Implemented Management for Daily Improvement Boards Managing for Daily Improvement (MDI) is focused on implementing a management system that creates, accommodates, and sustains a culture of continuous improvement The MDI System facilitates an ongoing transformation to a data driven, action oriented, engaged & empowered lean organization 7. Completion Plan Daily Activities Manage “Flow” of process outputs (Visually) Identify and prioritize anomalies of performance and make improvements Encourage associates to identify and eliminate waste Create an environment where associates are responsible for identification (and assisting in the elimination) of waste 7. Completion Plan MDI Goals Convert from being a reactive firefighter, whose attention and priority is focused on the self- perpetuating, never-ending fires whenever they occur (always on the edge of out of control) TO… A proactive Lean thinker who is managing and controlling his priorities and ultimately his destiny 21 7. Completion Plan Incremental daily improvement supplemented with Rapid Improvement Events Improvement Level RIE Events RIE Events Daily MDI Activity Event based improvement Incremental Daily Improvement (coupled with events) 8. Confirmed State Have we moved the dial? 20 months into our journey… $5.9M in Hard Dollar Savings Patient satisfaction with the arrival process improved by 57% Avoided $2.5M in capital expense by improving patient flow Falls reduced by 55% 9. Insights Lessons Learned? 1. Reason for Action: Leadership focus on the “what” not the “how” 2. Initial State: Must have 100% commitment from all (especially physicians). 3. Target State: Double the good…or…half the bad 4. Identifying Gaps: Focus on the process…not the people 5. Solutions: - Creativity over capital 6. Rapid Experiments: The best laid plans… 7. Completion Plan: A disciplined approach 8. Confirmed State: Hope is not a strategy…countermeasures 9. Insights: Some people will want to get off the bus…let them. 9. Insights “Committed and trained senior leadership, without question, is the key component in successfully transforming an organisation through lean initiatives” “Having a great partner, like Simpler, is essential to guiding an organization through such a transformative process.”