Block 1 Unit 3 Practice Exam Questions
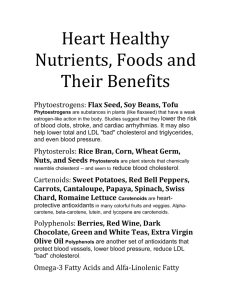
advertisement

Kevin Hogan Practice Exam Questions Gluconeogenesis Lipids 4 1. Which of the following class(s) of lipids is found in the cell membrane? A. Phospholipids B. Cholesterol C. Glycolipids D. All the above 2. What is an indicative factor that tells you that you are in the plasma membrane vs. the mitochondrial membrane? A. Outer leaflet with phosphotidyl ethanolamine B. Inner leaflet with phosphatidyl choline C. High cholesterol content D. Low cholesterol content 3. What is a phospholipid A. Steroid B. Phosphoglycerides C. Sphingolipids D. B & C E. All the above 4. What do all acyl-derived phosphoglycerides have in common ie.phosphatidylcholine…ethanolamine, serine, inositol, glycerol? A. Found on the inner leaflet of membrane B. Found on the outer leaflet of the membrane C. Ether linkage to the glycerol D. Ester linkage with the phosphate group 5. What phosphoglyceride can have two phosphatiidate molecules linked to a common backbone and is found in mitochondrial membranes? A. Phosphatidylinositol B. Phosphatidylcholine] C. Phosphatidylglycerol D. Phosphatidylethanolamine E. Phosphatidylserine 6. What is the main difference between phosphoglycerides and sphingolipids? A. An alcohol B. Different fatty scid composition C. Different backbones D. Linkage of the backbone E. All the above 7. What is the role of phosphoglycerides? 8. 9. 10. I II. III. 11. 12. 13. A. Respiratory role of alveoli B. Component of cell membranes C. Intracellular signaling D. All the above Which of the following is not a common step in the synthesis of phosphoglycerides? A. Formation of lysophatidate B. Use of CDP as an intermediate C. Addition of a 3rd acyl group D. Formation of phosphatidate E. None of the above What is the major pathway for phosphoglyceride formation in mammals? A. ATP-activated diacylglycerol intermediate B. CDP-activated diacylglycerol intermediate C. CDP-activated alcohol intermediate D. A & C E. B & C Which product’s synthesis began with dihydroxyacetone phosphate 1-Alkyl-2-Acyl Phosphatidylcholine Phosphatidyl choline Phosphatidal choline A. I B. II C. III D. I,III E. I, II What is the correct statement regarding plasmologens? A. Plasmologens have an acyl group at C1 B. Plasmologens have a double bond at C1 C. Plasmologens have an ether linkage and double bond at C2 D. Plasmologens’ synthesis begins with glycerol-3-phosphate E. Plasmologens have an ester linkage and double bond at C1 What is correct about platelet activating factor? A. It is a mediator of allergic hypersensitivity B. Has a acetyl group at C2 C. Has a palmitate at C1 via an alkyl bond D. It is involved in the release of serotonin from platelets E. All the above Which of the following is correct regarding sphingolipids? A. Spingolipids have a glycerol backbone B. Spingolipids aren’t phospholipids C. Spingolipids do not have a sugar chain D. Spingolipids are derived from palmityl CoA & serine 14. 15. 16. 17. 18. 19. 20. E. All the above What is the correct order first to last? A. Cerebroside, Sphingosine, Ceramide, Ganglioside B. Sphingosine, Ceramide, Cerebroside, Ganglioside C. Ceramide, Sphingosine, Cerebroside, Ganglioside D. Sphingosine, Cerebroside, Ceramide, Ganglioside Which sphingolipid involves the addition of phosphatidylcholine to nitrogen? A. Ceramide B. Cerebroside C. Gangliosides D. Sphingomyelin E. Sulfatides Which sphingolipid involves the addition of sugar using a high energy intermediate? A. Cerebroside B. Gangliosides C. Sulfatides D. Globosides E. All the above Which sphingolipid has a branched oligosaccharide without sialic acid? A. Sphingomyelin B. Sulfatides C. Ganglioside D. Ceramide E. Globoside What sphingolipid involves the addition of two or more sugars? A. Cerebrosides B. Gangliosides C. Globosides D. B & C E. All the above What autosomal recessive disease involves a deficiency in sphingolipid breakdown resulting in an accumulation of sphingomyelin? A. Tay-Sachs disease B. Gaucher’s disease C. Niemann-Pick disease D. Krabbe’s disease What disease involves lipid-filled lysosomes in neurons leading to blindness, deafness, paralysis, death by age 3? A. Tay-Sachs disease B. Gaucher’s disease C. Niemann-Pick disease D. Krabbe’s disease 21. What disease has a defect in β-N-acetylhexosaminidase A, which doesn’t allow gangliosides ending with GalNAc (GM2) to be degraded? A. Tay-Sachs disease B. Gaucher’s disease C. Niemann-Pick disease D. Fabry’s disease 22. Where is the defect in the disease that has three types characterized by an early childhood to late adult onset with common easy bruising, fatigue due to anemia, occasional lung & kidney impairment and more severe brain damage? A. β-N-acetylhexosaminidase B. glucocerebroside C. sphongomyelinase D. β-galactosidase 23. What do you think could be the explanation for different symptoms in type I vs. type II Gaucher’s disease? A. Patients who get type II have more glucose going to the brain due to gluconeogenesis B. Different tissue have different isoforms of glucocerebrosidase enzyme C. Obese children have more fatty acids to use instead of glucose, so they escape type II and get type I D. None of the above 24. What is the direct product(s) of phospholipase C in intracellular signaling? I. Arachidonic acid II. Prostaglandins III. Inositol phosphates IV. Diacylglycerol A. III B. III, IV C. I,III, IV D. I, II,III E. All the above 25. Which of the following is correct about the inflammation signaling pathway? A. Calcium-bound phospholipase C releases arachidonic acid from the plasma membrane B. Phosphorylated phospholipase A2 acts on the intracellular membrane C. IP3 activates protein kinase, which activates MAP kinase D. Ca++ activates G-protein allowing phospholipase C to cleave IP3 E. Ca++ binds to phosphorylated phospholipase A2 bringing it to the plasma membrane 26. Assuming that you have an inflammatory response triggered by activation of phospholipase C, which of the following could block the inflammation? A. An inhibitor of protein kinase C B. An inhibitor of Ca++ channels in the ER C. An inhibitor of phospholipase A2 D. All the above 27. What is the key regulatory enzyme in the formation of inflammatory response? A. Hydroperoxidase B. Cyclooygenase C. Prostacyclin synthase D. Thromboxane synthase E. Accolate 28. A patient enters your office with heightened levels of mast cell activity. You suggest a drug that specifically: A. Inhibits the synthesis of prostaglandin H2 B. Stimulates the synthesis of leukotrienes C. Stimulates the synthesis of prostacyclin D. Stimulates the synthesis of prostaglandin H2 E. Inhibits the synthesis of leukotrienes 29. The beneficial effect of low dose aspirin therapy in preventing recurrence of myocardial infarction is related to inhibition of production of: A. Leukotrienes B. Prostacyclins C. Sphingosine D. Thromboxanes E. Arachidonate 30. What drug blocks the hydrophobic channel where arachidonate enters the active site of cyclooxygenase? A. Ibuprofen B. Acetaminophen C. Aspirin D. Accolate E. None of the above 31. What drug lacks peripheral anti-inflammatory and ant-clotting effects, but can reduce fever and raise pain threshold? A. Aspirin B. Ibuprofen C. Advil D. Motrin E. None of the above 32. A drug company is looking to make a new anti-inflammatory drug that reduces the negative side effects seen in aspirin and ibuprofen. What should their target be? A. Block Cox-2, used to maintain normal body function B. Block Cox-2, induced with inflammation C. Block cyclooxygenase D. Block Cox-1, induced with inflammation E. Block Con-1, used to maintain normal body functions Lipids 5 1. What is the function(s) of cholesterol in the body? A. Cholesterol modulates membrane fluidity in the cell membrane B. Cholesterol is a precursor of steroid hormones C. Cholesterol is a precursor for synthesis of bile salts D. Cholesterol has branch points in its biosynthesis that lead to other important isoprene products E. All the above 2. What compound (s) has isoprene as a building block? A. Cholesterol B. Dolichol C. Ubiquinone D. Heme A E. All the above 3. What is the main regulatory enzyme for cholesterol synthesis? A. HMG-CoA synthase B. HMG-CoA reductase C. Acetyl-CoA thiolase D. Acetyl-CoA carboxylase E. None of the above 4. Where in the cell does the synthesis of HMG- CoA for cholesterol synthesis occur? A. mitochondria B. Golgi apparatus C. cytoplasm D. Endoplasmic reticulum E. None of the above 5. Which two processes would be expected to occur simultaneously A. Cholesterol synthesis & β- oxidation B. Cholesterol synthesis & ketogenesis C. Cholesterol synthesis & adipose lipolysis D. Cholesterol synthesis & fatty acid synthesis 6. Uptake of LDL-cholesterol into the adipose cells via receptor-mediated endocytosis has the following effect(s): A. Down-regulates HMG-CoA reductase B. Up-regulates HMG-CoA reductase C. Up-regulates LDL receptor production D. A & C E. B & C 7. Lovastatin, as well as many other statin drugs, work to lower cholesterol specifically by: A. Cleaving SREBP translocating to the nucleus B. Activating SRE stimulating transcription of HMG-CoA Reductase C. Irreversibly inhibiting the LDL receptor D. Competitively inhibiting HMG-CoA reductase E. None of the above 8. Which of the following things would you expect to occur in the liver of a patient with familial hypercholesterolemia (genetic defect that results in decreased number of functional LDL receptors)? A. Increased activity of HMG-CoA synthase B. Increased uptake of LDL cholesterol C. Increased activity of HMG-CoA reductase D. Decreased activity of HMG- CoA reductase 9. What reaction allows mevalonate to move further along in the formation of cholesterol. A. Two rounds of decarboxylation to HMG-CoA B. Three rounds of phosphorylation using CTP to form 3-Isopentenyl pyrophosphate C. Three rounds of reduction using NADH to form mevalonol D. Three rounds of carboxylation to HMG-CoA E. Three rounds of phosphorylation using ATP to form 3-Isopentenyl pyrophosphate 10. What substrate is the primer for the building of the 10 carbon chain in cholesterol synthesis? A. Dimethylallyl pyrophosphate B. Isopentenyl pyrophosphate C. Geranyl pyrophosphate D. Farnesyl pyrophosphate E. None of the above 11. Give the order of formation from 5 C-10C-15C-30C in the synthesis of cholesterol? A. Isopentenyl-PP, Farnesyl-PP, Geranyl-PP, Squalene B. Farnesyl-PP, Isopentenyl-PP, Geranyl-PP, Squalene C. Isopentenyl-PP, Geranyl-PP, Farnesyl-PP, Squalene D. Geranyl-PP, Isopentenyl-PP, Farnesyl-PP, Squalene 12. What occurs in the final stage(s) of cholesterol synthesis? A. Cyclization of squalene B. Formation of an epoxide C. Formation of 7-Dehydrocholesterol (precursor of vitamin D) D. A & C E. All of the above 13. What is true about bile salts? A. Produced in the gall bladder B. Non-polar derivative of cholesterol C. Facilitates the digestion of lipases D. It is excreted in feces once it has been utilized E. All the above 14. What is the major bile salt formed from condensation of an activated cholesterol derivative with glycine? A. Glycosterol B. Taurocholate C. Progesterone D. Glycocholate E. Cortisol 15. Match the following steroid hormones with their specific tissues. A. aldosterone-corpus luteum, estrogen-ovary, androgen-testes, progesterone-adrenals B. aldosterone-adrenals, estrogen-ovary, androgen-testes, progesterone- corpus luteum C. estradiol-adrenals, estrogen-ovary, cortisol-adrenals, testosterone-testes D. progesterone-adrenals, estrogen-ovary, cortisol-adrenals, aldosterone-adrenals 16. Progesterone is the precursor to what steroid hormone(s)? A. Aldosterone B. Cortisol C. Estrogen D. A&B E. All the above 17. Which of the following statements about the synthesis of steroid homones is incorrect? A. Aldosterone and Cortisol use enzymes 11 &21 hydroxylase B. Aldosterone can readily be converted to Cortisol using 17 hydroxylase C. Estrogen is synthesized from androgen using aromatase D. After pregnenolone is oxidized, 17 hydoxylase adds an OH and there is a cleavage of C17 to form androgen E. None of the above 18. What is the role of cytochrome p450? A. Mixed function oxidase that utilizes NADPH and O2 B. Detoxification of foreign substances and drugs C. Used to accept electrons in the electron transport chain D. A&B E. All the above 19. Which of the following would be a symptom of 17-Hydroxylase Deficiency? A. Hypotension (decreased blood pressure) and loss of Na+ in the urine B. Failure to develop secondary sex characteristics C. Inability to produce progesterone D. All of the above Lipid Digestion & Transport 1. Which of the following is true regarding cholesterol A. Dietary cholesterol makes up very little of our daily cholesterol input B. Most dietary cholesterol is formed into cholesterol esters C. Cholesterol is synthesized in the pancreas and sent into the bloodstream D. Cholesterol in cells affects the risk of cardiovascular disease E. All of the above 2. What enzyme is responsible for lipolysis of triglycerides in the stomach? 3. 4. 5. 6. 7. 8. A. Pancreatic Lipase B. Cholesterol esterase C. Gastric lipase D. Cholecystokinin E. None of the above Cholecystokinin stimulates the contraction of the gall bladder in the presence of fat, which forced bile where? A. Pancreas B. Duodenum C. Jejunum D. Ileum Bile salts emulsify dietary lipids using what enzyme(s) I.Pancreatic lipase II.Hydroxylase III.Colipase A. I B. II C. I, II D. I, III E. I,II,III Match up the structure with the function A. Jejunum-fat digestion, duodenum-fat absorption, ileum-absorption of bile acids B. Jejunum-absorption of bile acids, duodenum-fat digestion, ileum-fat absorption C. Ileum-fat digestion, jejunum-fat absorption, duodenum- absorption of bile acids D. Ileum-absorption of bile acids, duodenum-fat digestion, jejunum-fat absorption Orlistat (obesity drug) targets the activity of what enzyme involved in fat digestion? A. Cholesterol esterase B. Gastric lipase C. Hydroxylase D. Pancreatic lipase The endproducts of lipid digestion are incorporated into what structure essential for lipid absorption A. Intestinal wall B. Micelles C. Liposomes D. Lipid Bilayers E. Bile salts Which of the following is incorrect with regards to absorption of lipids? A. Fatty Acids activated by CoA and ATP can be combined with Glycerol-3-P to make Triglycerides B. A fatty acid is added to cholesterol making cholesterol ester C. Bile acids are taken up with acyl-CoA transferase in the jejunum D. 2- Monoacylglycerol can be added to an activated fatty acid to make triglycerides E. None of the above 9. What is the strategy for lowering blood cholesterol? A. Dietary phytosterols inhibiting cholesterol uptake into micelles B. Ezetimibe inhibiting the cholesterol transport C. Bile acid sequestrants reduce recycling of bile acids to the liver D. All the above 10. What is a difference between triglyceride digestion and cholesterol digestion? A. Way they are hydrolyzed B. Incorporation into micelles C. Way of transport across the intestinal epithelium D. Packaging for transport throughout the body E. None of the above 11. What is not a component of the chylomicrons? A. A high density protein composition B. Single layer of polar lipids C. Interior of nonpolar lipids D. Protein component E. None of the above 12. Match the following processes with their respective locations: synthesis of apo B48 and apoA; incorporation of TG, CE, C, PL; chylomicrons packaged into secretory vesicles; and the fusion of secretory chylomicrons. A. RER, SER, Golgi, Plasma membrane B. SER, Golgi, RER, Plasma membrane C. Golgi, RER, SER, Plasma membrane D. Plasma membrane, Golgi, SER, RER 13. Why are Medium Chain Triglyceride (MCT) good dietary supplements for patients unable to digest Long Chain Fatty Acids (LFCA) due to pancreatic, biliary, or intestinal problems? A. They are packaged into micelles B. They change the conformation of the CPT I in the carnitine shuttle C. They can enter the mitochondria without the carnitine shuttle D. None of the above 14. What apoprotein on the chylomicron’s surface binds to lipoprotein lipase activating it to hydrolyze fatty acids from triglycerides? A. Apo A B. Apo C-II C. Apo B-48 D. Apo E 15. What apoprotein is found in low-density lipoproteins and is involved in cholesterol transport? A. Apo B100 B. Apo C-II C. Apo B-48 D. Apo A Amino Acids: Part 1&2 1. What amino acid is an essential amino acid required in large amounts for the production of cysteine? A. Arginine B. Histidine C. Methionine D. Serine E. Phenylalanine 2 What non-essential amino acid is readily made from pyruvate? A. Alanine B. Asparagine C. Apartate D. Methionine E. Phenylalanine 3. Amino acids are taken into the small intestine using: A. Chylomicrons B. LDL lipoproteins C. Enterocytes D. Acyl carrier protein 4. What is the nontoxic water-soluble carrier of nitrogen taking it to the liver for urea synthesis? A. Alanine B. Glutamine C. Urea D. Ammonium 5. What properties of urea make it a well-suited carrier of nitrogen? A. Nontoxic nature B. Used only for excretion of excess nitrogen C. Highly water soluble D. Regulation of pH excreting bicarbonate E. All the above 6. What is the main function of glutamate dehydrogenase in nitrogen metabolism? A. Release of ammonia for urea synthesis B. Transfer of amino groups to α-ketoglutarate to make glutamate C. Generates apartate that provides one nitrogen for urea synthesis D. Involved in pyrimidine synthesis that uses glutamine E. Transfer of an amino group from amino acid to a keto acid 7. Under what conditions are ammonium ions excreted in relatively high concentrations in the urine? A. Normal pH B. Alkalosis environment C. Acidosis or uncontrolled diabetes D. None of the above 8. What enzyme plays an important role under conditions when ammonium ions are excreted? A. Glutaminase B. Glutamate dehydrogenase C. Transaminase D. Glutamate synthetase 9. 10. 11. 12. 13. 14. 15. 16. 17. E. None of the above What is correct with regards to the glucose alanine cycle operating in inter-organ metabolism? A. Provides transport of nitrogen from amino acid metabolism B. Produces pyruvate C. Its endproduct is used in gluconeogenesis in the liver D. All of the above E. None of the above Which of the following is incorrect with regards to the mechanism of transaminases? A. They transfer an amino group from an amino acid to a keto acid B. They use pyridoxal phosphate as a nucleophile for covalent catalysis C. They are essential in the elimination of urea D. Their catalytic scheme involves the use of a Schiff base E. None of the above What is the key regulatory enzyme of the urea cycle? A. Ornithine transcarbamylase B. Arginase C. Urease D. Carbamoyl phosphate synthetase What is the significance of the malate-aspartate shuttle in the urea cycle? A. Take ornithine made in the cytosol into the mitochondria B. Transport apartate into the mitochondria and glutamate out C. Transport aspartate into the mitochondria to be combined with citrulline D. Used as a symport for malate and aspartate E. None of the above What is the linkage between the urea cycle and the TCA cycle? A. Fumarate from the urea cycle can be used in the TCA cycle B. Asparate from oxaloacetate in the TCA is combined with citrilline in the urea cycle C. Glutamate from the urea cycle can be used to make α ketoglutarate in the TCA cycle D. A & B E. B & C Describe how the urea cycle is short term regulated: A. High protein diet causes an elevated synthesis of urea cycle enzymes B. N- acetylglutamate allosterically activates carbamoyl phosphate synthetase activity C. High protein turnover due to starvation increases urea synthesis D. All of the above Why is ammonia toxic? A. Inhibits glucagon release B. Depletes intracellular ATP C. Depletes α-ketoglutarate in the skeletal muscle D. Decreased calcium uptake by the mitochondria E. All the above What TCA intermediate is depleted in the brain during ammonia intoxication? A. Oxaloacetate B. Citrate C. α-ketoglutarate D. Succinyl CoA E. None of the above Which of the following is not a consequence of ammonia intoxication? A. Increased ATP synthesis B. Depletion of glutamate C. Activation of the N-methyl-D-apartate receptor causing increased Na+/K+ ATpase activity D. Increased calcium uptake by the mitochondria E. Reduction in the level of reduced glutathione 18. What is a treatment of ammonia intoxication? A. Low protein, high carb diet B. Increase in ammonium excretions using levulose C. Antibiotics D. A & C E. All the above 19. What is an example of an amino acid that yields precursors to fatty acids or ketone bodies? A. Alanine B. Arginine C. Leucine D. Glutamate E. Aspartate 20. What amino acid is metabolized to pyruvate? A. Alanine B. Serine C. Cysteine D. Glycine E. All the above 21. Someone with a defect in the branched chain keto acid dehydrogenase aka Maple syrup disease would expect which of the following? A. An decrease in the carboxylation of keto acids from leucine, isoleucine, and valine B. An accumulation of α-ketoisocaproate,α-keto-β-methylvalerate, and α ketoisovalerate C. Severe mental retardation in an isolated community D. B & C E . All the above 22. What is the defective enzyme in alkaptonuria and what accumulates? A. Homogentisate oxidase- Homogentisate B. α-ketoacid dehydrogenase- α-keto acids C. Methionine synthase- homocysteine D. Methylmalonyl-CoA mutase-methyl malonyl CoA E. Phenylalanine hydroxylase- phenylalanine 23. What is true about S-adenosyl methionine? A. It is formed from methionine in the presence of GTP B. It donates a methyl group to norepinephrine C. The enzyme used to catalyze it is the B12 enzyme methyl malonyl-CoA mutase D. Its structure has an adenosine attached to a cysteine E. All the above 24. What coenzyme abundant in the liver is needed to regenerate methionine from homocysteine? A. NAD+ B. TPP C. Coenzyme Q D. B 12 E. B 6 25. A patient comes into your office with chest pain and ischemia. You do tests on him and realize that he has elevated serum levels of homocysteine. What enzyme is defective in this case? A. Methylmalonyl –CoA mutase B. Methionine synthase C. Cystathionine β-Synthase D. Methionine adenosyl transferase E. Homogentisate oxidase 26. This same patient after diagnosis of homocystinuria is given vitamin B6, folic acid, and vitamin B12, but the serum levels of homocysteine remain elevated. You have to decide what to do next. What should you do? A. Give the patient only vitamin B12 B. Restrict the intake of methionine C. Add more methionine to the diet D. Supplement the patient with more homocysteine-derivatives E. None of the above 27. Which of the following about the synthesis of α ketoglutarate is incorrect? A. NAD is reduced B. NADPH is oxidized C. Ammonia is released from glutamate in the liver D. Glutamate dehydrogenase is activated by ADP and GDP E. None of the above 28. What is the role of the kidneys in the synthesis of arginine? A. Synthesis of citrulline from glutamate B. Take up citrulline C. Arginase activity needed for the urea cycle D. Transamination of glutamate to ornithine E. All the above 29. What disease involves a defect in the hydroxylation of an amino acid and sometimes a defect in the dihydrobiopterin cofactor? A. Alkaptonuria B. Ammonia Intoxication C. Cystinuria D. Maple syrup disease E. Phenylketonuria 30. What is the effect of nitric oxide formed from the reaction between arginine and citrulline? A. Relaxation of endothelial cells B. Prevents aggregation of platelets C. Reduces adhesion of white bloods cells in the vessels D. Neuromodulator in the brain E. All the above Lipoprotein Metabolism 1. What apoprotein made in the liver is bound to the LDL receptor? A. ApoB-100 B. VLDL C. ApoB-48 D. ApoA E. ApoE 2. If you have a patient with high LDL-Cholesterol, what are some ways of treating your patient? A. Supplement their diet with more saturated fatty acids B. Change their diet to one rich in phytosterols C. Use of statins D. B&C E. All the above 3. What is a way(s) of decreasing the levels of cholesterol in the blood? A. Decreasing cholesterol synthesis B. Increasing the transcription of LDL receptor proteins C. Decreasing the activity of HMG CoA reductase D. A & B E. B & C 4. What is responsible for the formation of plaques on the arterial wall? A. Oxidation of the LDL-Cholesterol B. Scavenger receptors C. Formation of foam cells D. LDL-Cholesterol taken up by macrophages E. All the above 5. Insulin regulates lipid metabolism by: A. Controlling the entry and exit of FA from adipocytes B. Inhibits lipoprotein lipase activity for fatty acid entry C. Stimulated hormone-sensitive lipase to stimulate release of fatty acids D. A & B E. All the above 6. When in the fasting state, hormone sensitive lipase is: A. Phosphorylated B. Converting triglycerides to 3 FA and glycerol C. Increases the amount of fatty acids in the blood D. B & C E. All the above 7. What type of fatty acid is most susceptible to lipid peroxidation? A. Saturated FA B. Trans FA C. Monounsaturated FA D. Cis FA E. Polyunsaturated FA 8. What enzyme is responsible for the elevated synthesis of TG-rich VLDL ? A. Cholesterol ester transfer protein B. Hepatic lipase C. Lecithin Cholesterol Acyl Transferase D. HMG CoA reductase E. None of the above 9. What lipoprotein have the highest atherosclerotic risk? A. Small LDL B. Large LDL C. Lipoprotein A D. Small HDL E. VLDL Lipids & Coronary Heart Disease 1. How does the accumulation of cholesterol result in coronary heart disease? A. LDL-Cholesterol is entrapped within the endothelium of the arterial walls B. LDL-Cholesterol is oxidized C. LDL- Cholesterol is taken up by macrophages to make foam cells D. Leads to plaque formation E. All the above 2. What is the correct progression in atherosclerosis with age? A. Fibrous plaque, fatty streak, occlusive plaque, thrombus B. Occlusive plaque, fatty streak, fibrous plaque, thrombus C. Thrombus, occlusive plaque, fibrous plaque, fatty streak D. Fatty streak, fibrous plaque, occlusive plaque, thrombus E. Fatty streak, occlusive plaque, fibrous plaque, thrombus 3. How do the arteries counteract the progression of atherosclerosis A. HDL- Cholesterol transports cholesterol back to the liver B. Arterial remodeling C. Expand the lumen D. A&B E. All the above 4. What is an effect(s) of atherosclerosis? A. Myocardial infarction B. Angina C. Loss of blood supply to the heart D. Leg Ischemia E. All the above 5. What is a risk factor (s) of Coronary Heart Disease? A. Obesity B. Inflammation C. Decreased lipid in the blood D. A& B E. All the above 6. Which of the following is incorrect with the regard to atherosclerosis? A. Oxidized LDL decreases NO synthetase activity B. Angiotensin II activity increases causing vasoconstriction C. CRP associated with inflammation causes CVD D. Immune cells in plaque release inflammatory cytokines E. Rupture of a plaque can result in an MI 7. What is the difference between a stable plaque and a vulnerable plaque? A. Stable have a thicker fibrous cap B. Vulnerable is less lipid-poor C. Stable has a lipid-rich plaque D. A & C E. All the above\ 8. What are some ways of reversing atherosclerosis? A. Statins B. Stress reduction C. Exercising D. 10% fat E. All the above Cell Signaling 1. What signal(s) is involved in rapid signaling? I. Peptide hormones II. Steroid hormones III. Catecholamines A. I, II B. I,III C. I D. II E. I,II,III 2. What signaling scheme involves a signal carried via the bloodstream to a distant target cell? A. Endocrine B. Paracrine C. Autocrine D. Synaptic E. None of the above 3. What type of signal-based communication is present in immune response with T cells? A. Gap junctions B. Contact C. Secretion D. Endocrine E. None of the above 4. What type of signal mechanism uses two molecules of acetylcholine to bind and allow the entry of ions? A. G-protein-linked B. Receptor tyrosine kinase C. Intracellular receptors D. Ligand-gated channels 5. What type of signal mechanism uses negatively charged amino acids to prevent the entry of anions and facilitates the entry of cations? A. G-protein-linked B. Receptor tyrosine kinase C. Intracellular receptors D. Ligand-gated channels 6. What is incorrect with regards to insulin signaling? A. It involves 2 α hormone binding chains and 2 β tyrosine kinase chains B. Insulin bound to the receptor causes an autophosporylation on the tyrosine residue C. IRS-I phosphorylated PI3K leading to the MAP kinase cascade D. IRS-I phosphorylates Shp, leading to activation of Ras E. IRS-I phosphorylated PI3K leading to the conversion of glucose to glycogen 7. What type of signaling mechanism is involves the regulation of gene expression? A. G-protein-linked B. Receptor-tyrosine kinase C. Intracellular steroid receptor D. Ligand-gated channels 8. What is incorrect about the G-protein linked receptor? A. It is has an extracellular amino terminus where neurotransmitters and catecholamines bind 9. 10. 11. 12. 13. 14. B. It is a 7 pass transmembrane protein C. Its αs chain binds and hydrolyzes ATP activating adenylate cyclase D. Its β/γ chains anchors the αs chain to the cytoplasmic face of the plasma membrane E. None of the above What is incorrect with regards to the cAMP mediated G-protein signaling? A. Generation of cAMP by Adenylyl cyclase is reversible using pyrophosphatase B. cAMP binds to Protein kinase (R2C2) C. Protein kinase releases a catalytic subunit that phosphorylates substrates D. Phosphodiesterase and dephosphorylation of substrates inactivates the response E. None of the above What is incorrect with regards to Ca++/ Phosphoinositide signaling? A. Acetylcholine is a main signaling molecule B. GTP bound G-protein activates Phospholipase C C. Cleaved Inositol trisphosphate triggers Ca++ D. DAG on the plasma membrane activates protein kinase C E. None of the above What drug could be used to mimic a protein in a mechanism leading to an increase of cellular pH and proliferation? A. Β arrestin B. Phorbol ester C. Calcium ionophores D. Atorvastatin E. Catecholamines An increase in the hormones bound to the G-protein receptor in the Ca++/ Phosphoinositide signal pathway leading to; A. Smooth muscle contraction B. Nitric oxide synthase activity C. Increease in cellular pH D. Activation of transcription factors controlling gene expression E. All the above What is correct with regards to down-regulation of insulin receptors? A. At early stages of hormone binding, receptors and peptide hormones are degraded B. Peroxisomes are responsible for the degradation insulin C. Prolonged exposure of insulin leads to the receptor degradation D. Down-regulation occurs because of overstimulation of insulin in a fast manner E. None of the above What mechanism(s) is used to inactivate G-protein signaling? A. Internalization of the G-protein receptor by lysosomes B. Phosphorylation of G-protein receptor C. Phosphorylation receptor bound by β arrestin D. A &C E. B & C Dyslipidemia Diet & Drug Therapy 1. In a clinical assessment of dyslipidemia, you take a lipid profile of a patient after a 12 hour fast with a total cholesterol measure of 400 mg/dL, a triglyceride measurement of 300 mg/dL, and a HDL-cholesterol measurement of 240 mg/dL. What amount of LDL-cholesterol does this patient have? A. 60 mg/dL B. 160 mg/dL C. 100mg/dL D. 140 mg/dL E. None of the above 2. What is the primary target for therapy in atherosclerotic disease? A. VLDL-cholesterol B. HDL-cholesterol C. Triglycerides D. IDL- cholesterol E. LDL-cholesterol 3. What is the best predictor of Coronary Heart Disease using a lipid profile? A. Low HDL-cholesterol B. High LDL-cholesterol C. Higher LDL/HDL D. Higher Total/HDL E. C &D 4. What is the type of dyslipidemia involves the overexpression of chylomicrons and abnormal level of triglycerides? A. Dyslipidemia I B. Dyslipidemia IIa C. Dyslipidemia IIb D. Dyslipidemia III E. Dyslipidemia IV 5. What is a common classification(s) of Dyslipidemia based on serum lipid levels? A . Hypercholesterolemia B. Hypertriglyceridemia C. Low HDL-cholesterol D. Mixed dyslipidemia E. All the above 6. What amount of LDL-cholesterol has the highest risk of heart disease? A. <100 mg/dL B. 100-129 mg/dL C. 130-159 mg/dL D. 160-189 mg/dL E. ≥ 190 mg/dL 7. What is a main risk factor (s) used in the assessment of Coronary Heart Disease? A. Family history B. Smoking C. Diabetes D. Age E. All the above 8. A patient with a family history of heart disease, atherosclerotic disease, diabetes and several other risk factors for coronary heart disease is having his serum lipids measured. He should do which of the following to reduce his risk for a heart attack? A. He should keep his LDL-cholesterol below 160 mg/dL B. He should keep his non-HDL- cholesterol below 190 mg/dL C. He should keep his LDL-cholesterol below 50 mg/dL D. He should keep his non-HDL-cholesterol below 100 E. None of the above 9. What is the best predictor of Coronary Heart disease using apoliprotein assessment, which is better than a lipid profile? A. High Apo B B. Low Apo A-1 C. High Apo A-1/ Apo B ratio D. High Apo B/ Apo A-1 E. Low Apo B/Apo A-1 10. What raises LDL-cholesterol far more than any other dietary factor? A. Saturated fats B. Trans fats C. Polyunsaturated fats D. A & B E. B & C 11. How does these fats raise the LDL-cholesterol? A. Increase the amount of hepatic LDL receptors B. Increase the absorption of LDL into adipocytes C. Downregulates hepatic LDL receptors D. Downregulates pancreatic lipase E. None of the above 12. A patient suffering from Hypertriglyceridemia and Low HDL Cholesterol should do which of the following to change his diet? A. A diet higher in fat B. A diet with fat high in mono and polyunsaturated fatty acids C. A diet lower in carbohydrates D. B & C E. All the above 13. Omega 3 fatty acids in fish have which of the following effects? A. Increases blood triglycerides B. Increases blood platelet adhesion C. Increases nitic oxide production D. Increases ischemic myocardial damage E. None of the above 14. Alcohol has which of the following effect(s)? A. Lowers HDL cholesterol B. Increases platelet adhesion C. Increases blood triglycerides D. A & C E. All the above 15. How does sitosterol (plant sterols) lower LDL cholesterol? A. Decreases the amount of triglycerides in the cells B. Competes with intestinal cholesterol C. Decreases fecal excretion of biliary and dietary cholesterol D. Decreases the amount of HDL-cholesterol absorbed E. All the above 16. Homocysteinemia , which is accumulation of homocysteine, leads to a higher risk of Coronary Heart Disease has a deficiency of: A. Vitamin B6 B. Folic Acid C. Vitamin B12 D. A & B E. All the above 17. What drug binds to receptors on the surface of adipocytes inhibiting lipase action on triglycerides and has the greatest effect of reducing LDL-C and triglycerides and increasing HDL-C? A. Statins B. Niacin C. Bile acid sequestrants D. Ezetimibe E. Fibrates 18. What drug has the greatest effect at lowering LDL-cholesterol? A. Statins B. Niacin C. Fibrates D. Bile acid sequestrants E. Ezetimibe Red Blood Cell Metabolism 1. 2. 3. 4. 5. Erthropoesis is stimulated in the kidney by which of the following conditions? A. End-stage kidney disease B. Lack of carbon dioxide C. Lack of oxygen D. A & C E. None of the above Erthropoietin has which of the following effect? A. Stimulated growth of red cell precursors B. Suppresses apoptosis C. Stimulates globin synthesis D. A & C E. All the above There is a decreased production of red cells in: A. Cancer patients undergoing chemotherapy B. HIV patients treated with reverse transcriptase inhibitors C. Patients post invasive surgery D. A & C E. All the above What is the function of Glutathione? A. Detoxification of hydrogen peroxide B. Oxidation of reduced protein thiols C. Oxidation of Met Hb (Fe+3) to Hb (Fe+2) D. A& C E. All the above What are the component(s) needed in the synthesis of glutathione? A. Glutamate B. Cysteine 6. 7. 8. 9. 10. 11. 12. C. Glycine D. ATP E. All the above How is reduced glutathione produced enzymatically from oxidized glutathione? A. Glutathione reductase couples the reduction of glutathione with oxidation of NADH B. Glutathione peroxidase reduces hydrogen peroxide while reducing glutathione C. NADP is used to reduce glutathione D. NADH is used to reduce glutathione E. NADPH is oxidized and reduces glutathione\ Which of the following is true with regards to synthesis of 2,3 diphosphoglycerate? A. 2,3 DPG is synthesized from 1,3 diphosphoglycerate using 2,3 diphosphoglycerate phosphatase B. When storing blood, 2,3 DPG levels remain constant C. Diphosphoglycerate mutase is inhibited by 2,3 DPG D. 2,3 DPG concentration in the red blood cell is much less than the amount of hemoglobin E. All the above Which of the following statements is incorrect with regards to 2,3 DPG? A. 2,3 DPG decreases Hb affinity for O2 by stabilizing the T state B. 2,3 DPG concentrations are lower in the tissues C. 2,3 DPG prevents the excessive accumulation of ATP D. 2,3 DPG acts as an effector of phosphofructokinase stimulating glycolysis E. None of the above What genetic condition reduces the concentration of 2,3 DPG increasing its binding affinity at the tissues? A. Pyruvate kinase deficiency B. Hexokinase deficiency C. Glucose-6-phosphate dehydrogenase defieciency D. Methemoglobin Anemia E. None of the above In red blood cells, there is a need for ATP, NADH, 2,3 DPG, and NADPH. How are all of these needs met in the red blood cells? A. Glycolysis B. TCA cycle C. Pentose Phosphate Pathway D. A & C E. All the above What happens during the pentose phosphate pathway that is necessary as energy utilization for the red blood cell? A. Four electrons from oxidation of glucose 6-P and 6-P-gluconate are used to reduce NADP to NADPH B. Fructose 6-P and glyceraldehydes 3- P are produced C. Oxidative metabolism used to reduce glutathione D. Pathway activity increases with oxidation of glutathione E. All the above What way(s) is methemoglobin reduced? A. Methemoglobin reductase using NADH B. Methemoglobin reductase using NADPH C. Glutathione reduction 13. 14. 15. 16. 17. 18. 19. 20. D. A&C E. All the above What enzyme is responsible for reducing methemoglobin (Hb-Fe3+) to hemoglobin (Hb-Fe2+) using NADH ? A. Methemoglobin reductase I B. Cytochrome b5 reductase C. Diapherase I D. All the above What conditions can increase the concentrations of methemoglobin? A. High oxygen B. Smoking C. Toxic oxidants D. B & C E. All the above Which of the following is used to deal with the oxidative stress of highly reactive oxygen species by accelerating the bimolecular reaction through one electron reduction to hydrogen peroxide and an electron oxidation to oxygen? A. Superoxide dismutase B. Ascorbate C. Vitamin E D. B & C E. All the above Glucose 6-phosphate dehydrogenase deficiency has which of the following effect on red blood cells? A. Lipid oxidation B. Destruction of spectrin C. Production of methemoglobin D. A & B E. All the above Hemolysis in Glucose 6-phosphate dehydrogenase deficiency can be induced by which drug (s)? A. Antibiotics B. Ibuprofen C. Antimalarial drugs D. Ascorbate E. All the above Which of the following conditions increases concentration of 2,3 DPG in the red blood cells? A. Hypoxia B. Heart Failure C. Fetal Hb D. A & B E. All the above What phospholipids are primarily found on the external leaflet on the red blood cell membrane? A. Phosphatidyl ethanolamine B. Phosphatidyl choline C. Spingomyelin D. B &C E. A & C Intrinsic membrane proteins: 21. 22. 23. 24. 25. 26. 27. A. Are not typically associated with the hydrocarbon layer B. Can be removed with salt or pH change C. Is spectrin D. Is band 3 E. None of the above Which of the following statements is incorrect about spectrin? A. Consists of a α2β2 tetramer B. Forms an antiparallel coiled coil triple helix C. Forms part of the cytoskeleton on the outer face of the membrane D. Forms links between band 3 and glycophorin c E. Maintains the shape of the erythrocyte What is the defect that causes hereditary spherocytosis? A. β-spectrin B. α-spectrin C. ankyrin D. defects in interaction with band 3\ E. All the above What is the role of band 3? A. Forms the cytoskeleton on the inner membrane B. Used to exchange Na+ and K+ C. Used to exchange water D. Used to exchange chloride and bicarbonate E. None of the above Which of the following is incorrect with regards to anion exchange proteins? A. AE proteins allow cells to overcome the energy barrier with a more favorable transport B. They are highly specific for solute C. They are very different from enzymes D. Oxygen and carbon dioxide readily pass through the membrane E. They are antiporters The use of anion exchange proteins is used in conjunction with what enzyme involved in pH balance in cells? A. Carbonic anhydrase B. Hexokinase C. Carboxykinase D. Acetyl CoA reductase E. None of the above What happens in red blood cells at the tissues? A. Haldane effect B. Formation of carbamino hemoglobin C. Bicarbonate enters the cells and chloride leaves the cells D. CO2 is released from the red blood cells E. There is an increase in pH Glut 1 : A. Is stimulated by insulin B. Requires ATP C. Has six membrane spanning αhelices D. Is a intrinsic membrane protein E. All the above 28. Phoshorylated Na+K+ ATPase allows what to happen? A. High intracellular K+ to leave the cell B. 3 Na+ to exit the cell C. 2 K+ to enter the cell D. High extracellular Na+ to enter the cell E. None of the above 29. What is correct with regards to old damaged erythrocytes? A. Reactive oxygen species are the cause of damage B. Damaged cells are cleared by macrophages in the spleen C. When damaged, hemoglobin binds to the N-terminus of band 3 forming an aggregate D. Epitopes on cell surface bind to IgG E. All the above 30. Which of the following about glycophorin is incorrect? A. Glycophorin is a single pass protein B. Glycophorin has a negative charge on sialic acid on red blood cell surface C. Individuals lacking glycophorin A and B have an increase in glycosylation of band 3 D. Glycophorin is the site of determinants for MNs blood group antigens E. Glycophorin B is the most abundant 31. What blood type has an H substance with a glycosylation of a GalNAc? A. A B. B C. AB D. O 32. Where in the body is most of the iron found? A. Freely soluble throughout the body B. White blood cells C. In the intestines D. Bound to hemoglobin E. None of the above 33. What is the function(s) of iron? A. Oxygen transport and release B. Electron transport C. Aconitase D. Peroxidase activity E. All the above 34. What is an indicator of iron deficiency? A. Hemoglobin levels B. Mean corpuscular volume C. Total iron binding capacity D. Serum ferritin E. All the above 35. What physiological condition (s) have most of the iron bound to transferring? I. Late pregnancy II. Iron deficiency III. Β thalasemia major IV. Hemochromatosis A. I, II B. I, III, IV 36. 37. 38. 39. 40. 41. 42. 43. C. III, IV D. II E. II, III What dietary constituent(s) inhibit iron absorption? A. Vitamin C B. Fiber C. Fructose D. Citric acid E. All the above What dietary constituent(s) promote iron absporption? A. Methionine B. Tannins C. Oxalic acid D. Divalent metals E. All the above What physiological states promote iron uptake? A. Infection and inflammation B. Anemias C. Inadequate production of stomach acid D. A & B E. None of the above What physiological states inhibit iron uptake? A. Hypoxia B. Hemolysis C. Erythropoiesis D. A & B E. None of the above Which of the following is incorrect with regards to iron? A. Iron is important in pregnancy B. Iron is toxic in large amounts C. Iron is broken down and excreted using iron oxidase D. Iron is involved in redox reactions generating reactive oxygen species E. Iron is freely soluble at acidic pH What is true with regards to the uptake of iron by mucosal enterocytes A. Ferric reductase on the apical surface reduces Fe+2 to Fe+3 B. Hephaestin on the apical surface oxidizes Fe+3 to Fe+2 C. Divalent metal transporter on the apical surface is a proton coupled transporter of Fe+2 D. Ferritin is an iron binding protein found on the basolateral surface E. Stimulator of iron transport (SFT) is a transporter of Fe+2, not Fe+3 What enzyme is needed in the absorption of heme iron that is not found in the uptake of uncomplexed iron? A. Ferroxidase B. Heme reductase C. Ferric reductase D. Heme oxidase E. None of the above Which of the following is a negative regulator of release of iron and its synthesis is induced by inflammation and infection+ 44. 45. 46. 47. 48. A. Interleukin 6 B. Hepcidin C. Hephaestin D. Ceruplasmin E. Ferritin What is the soluble copper ferroxidase in plasma that is involved in the delivery of iron to various tissues? A. Ceruplamin B. Ferroportin C. Hepcidin D. Hephaestin E. Aconitase Which of the following iron stores in the insoluble form? A. Ferritin B. Hemosiderin C. Ceruplamin D. Hepcidin E. Hephaestin Which of the following is incorrect with regards to transferrin? A. Has two iron binding sites per subunit specific for ferric iron B. Required bound bicarbonate to bind C. Binds ferric iron which is released on the basolateral surface of enterocytes D. Apo-transferrin releases iron under acidic conditions E. Each subunit has covalently bound palmitate Under conditions where there is low cellular iron, what occurs? A. IRE allows for ferritin mRNA translation B. Transferrin receptor mRNA is degraded C. IRP (Aconitase)binds to transferrin receptor mRNA stabilizes it and translates D. A &B E. A & C A patient is diagnosed with genetic hemochromatosis. What are the following effect(s)? A. Excessive iron absorption B. Defect in the glycoprotein associated with transferring receptor affinity for tranferrin C. Accumulation of iron D. A & B E. All the above Clinical Nutrition 1. Which of the following causes of death is the second most deaths next to tobacco use in the United States? A. Alcohol consumption B. Motor vehicles C. Poor diet D. Firearms E. Illicit drug use 2. According to the CDC, since 1900 life expectancy has increased by 30 year. Of those years, how many years were due to the public health and prevention measures? A. 5 3. 4. 5. 6. 7. 8. 9. 10. B. 10 C. 15 D. 25 E. 27 What is the CDC’s definition of a healthy diet? A. Meats low in cholesterol B. Diet low in saturated and trans fats C. Plant-based D. No red meat diet E. Low carbohydrates What increases the risk of heart disease, stroke, diabetes the most from birth? A. Large birth size B. Obesity as an adult C. Low birth weght D. A & B E. B & C Which of the following is incorrect regarding diets? A. Eating a diet high in sugar increases blood triglycerides B. Eating a diet high in saturated fat increases cholesterol levels C. Eating omega-6 fatty acids can decrease mRNA of several interleukins that increase inflammation D. Eating certain foods can affect gene expression E. None of the above A patient’s body mass index is taken and the result is a BMI of 35.1? A. Underweight B. Overweight C. Obesity I D. Obesity II E. Obesity III Of the comoribities, which of the following has the greatest risk at higher BMIs? A. Type II diabetes B. Cholelithiasis C. Hypertension D. Coronary heart disease E. Type I diabetes What is the effect of saturated fat in a patient suffering from Type II diabetes? A. Depresses the activation of PPARa B. Reduces the activity of peroxisomes C. Increases inflammation D. A& B E. All the above Why is visceral fat more of a risk for Type II diabetics? A. Visceral fat is higher in LDL cholesterol B. Visceral fat has more pancreatic lipase C. Visceral fat causes more fatty acids to be in circulation D. Visceral fat is linked to dementia E. None of the above Which of the following increases the risk of diabetes 11. 12. 13. 14. 15. 16. 17. A. Lack of physical activity B. Abdominal obesity C. Maternal diabetes D. High saturated fat intake E. All the above What is a possible reason why obesity can be linked to cancer? A. IGF-1 is an activator of AKT, an inhibitor of apoptosis B. Obesity mobilizes the differentiation of various carcinogens C. Saturated fat increases the free radicals in the cell leading to undifferentiated cell growth D. A& C E. All the above Which of the following factors does not increase salt sensitivity A. Age B. Women C. Smoking D. African Americans E. Renal insufficiency Which of the following is not true with regards to salt? A. High salt intake increases calcium loss in urine B. Higher in salt foods are lower in potassium C. Very little dietary salt comes from added salt D. Salt restriction increases efficacy of medications E. Salt restriction reduces blood pressure in all hypertensive subjects Which of the following lifestyle modifications does not seem to lower blood pressure in hypertensive patients? A. Have a drink of alcohol a day B. Physical activity for a half hour a day C. Reduce sodium intake to no more than 2400 mg D. Reduce intake of dietary magnesium E. Reduce intake of dietary saturated fat and cholesterol Which of the following is incorrect with regards to the DASH diet? A. DASH diet is high in fiber B. DASH diet emphasizes a diet with no saturated fats C. DASH diet plan emphasizes a diet 2 or less lean protein D. DASH diet plan with salt restriction has the most effective for lowering blood pressure E. DASH diet plan emphasizes a diet of 4-5 servings of nuts per week A 58 year-old female patient has been recently diagnosed with small amounts of bone loss. What is a recommendation of treatment you can make to reduce the progression of osteoporosis? A. 400-800 IU Vitamin D supplement B. 1,000 mg of calcium C. Thyroid hormone D. Blood cholesterol reducers E. Immunosuppresant drugs to reduce the breakdown of bone In order to reduce the risk of chronic disease, a patient should not do which of the following: A. Workout 30-45 minutes a day B. Have a diet high in protein, low in saturated fat with emphasis on plants C. Reduce the intake of sodium to 2300 mg D. Get their BMI to a level below 24.9 E. Have minimal amount of sugar Heme Metabolism 1. 2. 3. 4. 5. 6. 7. Which of the following is not a function of heme in heme proteins? A. Transport and retention of O2 B. Subsequent release of O2 in the tissues C. O2 activation of cytochrome c oxidase D. H2O2 activation in peroxidase E. Cytochromes in mitochondria involved in electron transport Which of the following is incorrect with regards to cobalamin? A. Cobalamin has a porphyrin with a cobalt in the center B. Cobalamin is also known as vitamin B12 C. Cobalamin is involved in rearrangements from internal group transfer D. Methionine synthase is an example of cobalamin involved in the conversion os homocysteine to methionine E. Methyl malonyl-CoA mutase is an example of cobalamin used to convert methylmalonyl-CoA to succinyl-CoA What is the regulatory enzyme for the committed step in heme synthesis? A. γ-aminolevulinate dehydratase B. Ferrochelatase C. Protoporphyrin oxidase D. γ-aminolevulinate synthase E. Porphorobilinogen deaminase What is true about the committed step in the heme synthesis? A. It is localized in the cytosol B. Lysine forms a Schiff base reacting with succinyl CoA making γ-aminolevulinate C. ALAS 2 are expressed in the liver D. The enzyme in synthesis of γ-aminolevulinate uses vitamin b 6 E. ALAS 1 on the X chromosome is expressed in erythroid cells What enzyme is responsible for the transfer of ALA from the mitochondria to the cytoplasm forming porphobilogen from 2 ALA and has an active site with Zn that is displaced with Pb? A. γ-aminolevulinate dehydratase B. Ferrochelatase C. Protoporphyrin oxidase D. γ-aminolevulinate synthase E. Porphorobilinogen deaminase What enzyme is responsible for the formation of hydroxymethylbilane from successive porphobilinogen units using dipyrromethane prosthetic group attached through a cysteine? A. γ-aminolevulinate dehydratase B. Ferrochelatase C. Protoporphyrin oxidase D. γ-aminolevulinate synthase E. Porphorobilinogen deaminase Which of the following is incorrect with regards to the steps to the production of heme from hydroxymethylbilane? 8. 9. 10. 11. A. Hydroxy-methylbilane forms an enzyme-bound spiro-intermediate protoporphorin IX B. Uroporphyrinogen III is decarboxylated four times to coproporphyrinogen III C. Coproporphyrinogen III oxidase decarboxylates coproporphyrin twice and oxidizes D. Ferrochelatase inserts ferrous iron to make heme E. Ferrochetalase is upregulated in erythroid cells Which is of the following is true about lead poisoning? A. ALA is found in urine B. Lead inhibits protoporphyrin oxidase C. Interferes with iron transport into the mitochondria D. There is an accumulation of Zn-protoporphyrin IX E. All the above Match up the following hepatic porphyrias with the correct enzyme defect A. Acute intermittent porphyria-PBG deaminase; ALA dehydratse deficiency-ALA dehydratase; Erthropoietic protoporphyria-ferrochelatase B. Acute intermittent porphyria-ALA dehydratase; ALA dehydratase deficiency- PBG deaminase; Erthropoietic protoporphyrin-ferrochelatase C. Acute intermittent porphyria- Protoporphyrinogen oxidase; ALA dehydratase deficiencyALA dehydratase; Hereditary coproporphyria- coproporphyrinogen oxidase D. Acute intermittent porphyria- PBG deaminase; ALA dehydratase deficiency- ALA dehydratase; Hereditary coproporphyria- coproporphyrinogen oxidase Which of the following to true with regards to regulation of heme synthesis? A. High heme inhibits activity of ALAS 2 B. High heme inhibits the mitochondrial import of ALAS2 C. Iron enhances the transcription of ALAS 2 D. A & C E. B & C Under conditions of low iron, which of the following occurs? A. Iron regulatory protein is activated B. ALAS 2 translation is suppressed C. Protein kinase HRI is activated phosphorylating eIF-2 D. Inhibition of translation of globin α and β chain mRNA. E. All the above Bile 1. What occurs to the erythrocyte membrane with time that promotes their clearance? A. Oxidative damage to the membrane phospholipids B. Sialic acid masks the erythrocytes C. Band 3 oligomerizes D. Glycophorin is desialated E. All the above 2. What is a pathway for clearance of senescent erythrocytes? A. Lysosomes insert hydrolase into erythrocytes causing apoptosis B. Autoantibodes bind to the surface of senescent erythrocytes and are phagocytized C. Phosphatidyl serine on the outer leaflet targets macrophage for destruction D. B & C E. All the above 3. What is the role of haptaglobin in heme transport? A. Complexes with αβ dimmers mediating the uptake of hemoglobin by the liver B. Binds to hemin forming methemalbumin 4. 5. 6. 7. 8. 9. 10. 11. C. Binds to hemin and is taken up by liver parenchymal cells D. Binds to methem and goes to the liver E. None of the above What is not true with regards to the first enzymatic step in heme degradation? A. Enzyme is membrane bound in the Golgi B. Heme oxygenase is the enzyme that catalyzes this reaction C. Ferric heme is reduced using NADPH D. Reaction produces CO E. Enzyme has three isozymes What enzyme is responsible for the conversion of biliverdin to bilirubin? A. Heme oxygenase B. Bilrubin reductase C. Bilirubin glucuronidase D. UDP-glucuronosyl transferase E. ALA synthase How is the inducible form of heme oxygenase stimulated in the liver and spleen? A. Hemoglobin B. Methemalbumin C. Splenectomy D. Hypoxia E. All the above Which of the following is the physiological role of bilirubin? A. Product of the heme oxygenase reaction B. Scavenger of peroxyl radicals C. Activates guanylate cyclase D. Inhibits proinflammatory processes and endothelial cell apoptosis E. Neurotransmitter In order for bilirubin to be transported into bile, what must occur? A. Hydrogen bonds added to the bilirubin Z conformer B. Unconjugated, or indirect bilirubin enters the bile ducts by diffusion across the membrane C. Glucuronic acid is conjugated to bilirubin D. A& B E. A & C What happens to bilirubin glucuronides once they enter the large intestine? A. Turned into urobilinogen excreted in the feces B. Turned into urobilinogen, reabsorbed, and passed to the liver C. Turned into urobilinogen, reabsorbed, and passed to the kidney D. A & B E. All the above What is the rate limiting step in bile metabolism? A. Conversion of heme to biliverdin B. Conversion of biliverdin to bilirubin C. Conversion of bilirubin to diglucoronides D. Secretion of bilrubin diglucoronides to bile E. Release of bile into the small intestine What disease is characterized by the increase in both direct and indirect bilrubin found in the plasma with elevated ALT and AST serum levels? A. Hemolytic Jaundice B. Hepatocellular Jaundice C. Obstructive Jaundice D. Gilbert’s syndrome E. Crigler-Najjer syndrome 12. What is an effective way to treat neonatal jaundice converting bilrubin to a more soluble form without glucorides? A. Phorbol ester therapy B. Vitamin E supplement C. Phenobarbital D. Liver transplant E. Phototherapy 13. Tin-protoporphyrin is also used to treat neonatal jaundice by inhibiting what enzyme? A. Heme oxygenase B. Biliverdin reductase C. UDP-glucuronosyl transferase D. Plasma alkaline phosphatase E. Plasma amino transferase 14. What disease is caused by reduced or absent UDP-glucuronosyl transferase leading to excessive bilirubin in the blood? A. Kernicterus B. Gilbert’s syndrome C. Crigler-Najjer syndrome D. B & C E. All the above Disorders of RBC 1. Which of the following is an incorrect classification of anemias classified morphologically? A. Mean corpuscular volume B. Shape C. Hypoplastic D. Red blood cell distribution width E. None of the above 2. What type of cells are characterized by residual RNA? A. Spherocytes B. Spur cells C. Pronormoblasts D. Schizocytes E. Reticulocytes 3. Anisocytes are characterized by what? A. Minimal surface area for a given volume B. Increase in membrane lipids C. Myeloid: Erythroid ratio 1:1 D. Clotheslined red blood cells E. High RDW 4. Acanthocytes are characterized by what? A. Minimal surface area for a given volume B. Increase in membrane lipids 5. 6. 7. 8. 9. 10. 11. C. Myeloid: Erythroid ratio 1:1 D. Clotheslined red blood cells E. High RDW Schizocytes are characterized by what? A. Minimal surface area for a given volume B. Increase in membrane lipids C. Myeloid: Erythroid ratio 1:1 D. Clotheslined red blood cells E. High RDW Marrow erythroid hyperplasia is charachterized by what? A. Minimal surface area for a given volume B. Increase in membrane lipids C. Myeloid: Erythroid ratio 1:1 D. Clotheslined red blood cells E. High RDW What anemia disorder has large immature nucleus, well –hemoglobinized cytoplasm, and lack of mature normoblasts? A. Marrow erythroid B. Folate deficiency C. Β-thalassemia D. Aplastic anemia E. Hyperplastic anemia What type of cells are expressed the most in Hemolytic Anemia trying to compensate for the loss of RNA? A. Normoblasts B. Granulocytes C. Neutrophils D. Reticulocytes E. Platelets Why are there more white blood cells than red blood cells in normal bone marrow? A. White blood cells’ lifespan is only 6 hours B. Red blood cells have a small storage pool C. White blood cells need to present to react to infection or inflammation D. B & C E. All the above What anemic disorder is characterized by a marked decrease in the red blood cell precursors and white blood cell precursors? A. Marrow erythroid hyper B. Folate deficiency C. Β-thalassemia D. Aplastic anemia E. Hyperplastic anemia What anemic disorder is characterized by a 9:1 hematopoietic cell to fat cell ratio? A. Marrow erythroid hyperplasia B. Folate deficiency C. Β-thalassemia D. Aplastic anemia E. Hyperplastic anemia 12. Why is it important that red blood cells lose their nucleus? A. Cardiac work decreases B. Pliability of the nucleus C. Decreases the whole blood viscosity D. A & B E. All the above 13. Which of the following is true with regards to reticulocytes? A. Same size as mature red blood cells B. Contain RNA, ribosomes, and mitochondria C. Dependent on glycolysis D. Can’t synthesize own hemoglobin E. Can’t take up iron with transferring receptor 14. Which inherited disorders are associated with hemolysis? A. Hemoglobinopathies B. Enzymopathies C. Membranopathies D. All the above 15. Which of the following is incorrect with regards to hemoglobinopathy? A. It is a result of impaired solubility of hemoglobin in hereditary spherocytosis B. Unstable hemoglobin leads to denatured aggregates called Heinz bodies C. Imbalanced globin chain synthesis leads to β-thalassemia D. Hemoglobin F may persist hereditarily E. Increase in oxygen affinity leads to polycythemia 16. Which of the following is incorrect with regards to enzymopathies? A. May impair synthesis of heme B. May impair the reduction of Met Hb C. May impair protection from oxidants due to G-6-PD deficiency D. May impair ATP production due to pyruvate kinase deficiency E. None of the above 17. Which of the following diseases disruption of the vertical interactions with mutations in β spectrin, ankyrin, band 3 and has a high level of osmotic fragility leading to hemolysis? A. B thalassemia B. Hereditary elliptocytosis C. Hereditary spherocytosis D. Hereditary pyropoikilocytosis E. RBC fragmentation syndrome 18. Which of the following diseases disruption of the horizontal interactions with mutations in α spectrin, protein 4.1, glycophorin C which doesn’t lead to hemolysis? A. Disseminated Intravascular Coagulation B. Hereditary elliptocytosis C. Hereditary spherocytosis D. Hereditary pyropoikilocytosis E. Alloantibody-mediated hemolysis 19. Which type of membranopathy is involved in the Rh disease in the fetus or during blood transfusions? A. Disseminated Intravascular Coagulation B. Hereditary elliptocytosis C. Hereditary spherocytosis D. Hereditary pyropoikilocytosis E. Alloantibody-mediated hemolysis Clinical Nutrition/Weight Management 1. What is a cause(s) of obesity? A. Genetics B. Poor Diet C. Lack of physical activity D. Reaction to certain foods E. All the above 2. What is a medical complication due to obesity? A. Pulmonary disease B. Osteoarthritis C. Cataract D. Coronary Heart disease E. All the above 3. Besides BMI, what is an additional risk factor(s) for cardiovascular disease? A. Large waist circumference B. 5 kg or more weight gain since age 20 C. High lean body mass D. A & B E. All the above 4. A patient enters your office and is diagnosed with pre-diabetes. What should you recommend to the patient do in order to improve insulin sensitivity? A. Increase the amount of HDL- Cholesterol in the diet B. Maintain a stable BMI C. Lose weight D. B & C E. All the above 5. Weight lose decreases all the following except: A. Blood pressure B. Apnea ev ents C. HDL-cholesterol D. LDL-cholesterol E. Hb A1C 6. All of the following are true with regards to physically active person’s energy expenditure except: A. The energy expenditure on digestion is less B. The energy expenditure on physical activity is more C. The energy expenditure for metabolism is more D. The energy expenditure for the entire body is more E. None of the above 7. Regulation of food intake is affected by all of the following except: A. Emotions B. Central signlas C. Peripheral signals D. Food characteristics E. None of the above 8. When beginning to put a patient on a weight loss regimen, you should first assess: A. Motivation B. Psychiatric issues C. Goals for large reduction in weight D. A & B E. All the above 9. The obesity treatment for a patient with a BMI between 27-29.9 and a family history of hypertension, diabetes, and coronary heart disease should be which of the following? A. Diet and Exercise B. Drug therapy C. Surgery D. A &B E. All the above 10. Which of the following is incorrect with regards to physical activity? A. Diet as well as physical activity reduces loss of fat-free mass B. Physical activity alone results in a high amount of weight loss C. High physical activity with behavorial therapy has a large effect on weight loss D. Decreasing sedentary activity in children works the best at decreasing overweightness E. Multiple short bouts of exercise have a greater effect than does single long bouts 11. What drug approved by the FDA for treating Diabetes long-term prevents fat digestion and absorption by binding to gastrointestinal lipases? A. Orlistat B. Sibutramine C. Diethylpropion D. Phentermine E. Benzphetamine 12. What drug approved by the FDA for treating Diabetes long-term is an appetite depressant by blocking the reuptake of serotonin and other neurotransmitters, but has many side effects including increased blood pressure? A. Orlistat B. Sibutramine C. Diethylpropion D. Phentermine E. Benzphetamine 13. What drugs can cause weight gain? A. Insulin B. Β-adrenergic receptor blockers C. Psychotropic medications D. Steroid hormones E. All the above 14. A patient comes to your office with a BMI of 36 with a family history of diabetes and atherosclerosis. What treatment would you recommend? A. Diet and exercise B. Sibutramine C. Portion size consult D. Bariatric surgery E. All the above Disorders-heme synthesis & catabolism 1. Which of the following is always a factor of iron deficiency anemia in adults? A. Pica, or strange cravings for strange things B. Fatigue C. Excessive bleeding D. Loss of apetite E. Koilonychia 2. Which of the following is not always diagnostic of iron deficiency? A. Low ferritin in the absence of inflammation B. Increase in the total-iron binding capacity of transferrin C. Low serum iron D. Decrease in mean corpuscular Hb concentration (hypochromic) E. Hemosiderin in marrow significantly decreases 3. Which of the following is not a compensatory feature for Iron deficiency anemia? A. Increase in iron absorption B. Increase in hepcidin C. Increase in iron transport D. Decrease in porphyrin synthesis E. Decrease in synthesis of α and β chains 4. Which of the following is not a non-specific response to hypoxia? A. Increase in serum erythropoietin B. Decrease in cardiac output C. Increase in arterio-venous PO2 difference D. Increase in red blood cells 2,3 BPG production E. None of the above 5. Which of the following cause the oxyhemoglobin dissociation curve shift to the right? A. Decrease in temperature B. Increase in 2,3 BPG C. Alkalosis D. Increase in ventilation E. Methemoglobin 6. Which of the following occurs in response to Hypoxia Inducible Factor (HIF-1) A. In normoxia HIF-1 is hydroxylated and ubiquitinated-sent to proteosome B. In hypoxia, αβ dimer forms C. Binds to regulatory element increase Erythropoietin gene D. Downregulates Hepcidin transcription and serum level iron drops E. All the above 7. Which mechanism goes wrong in sideroblastic anemia? A. Impaired respiratory chain activity B. Sequestration by mitochondrial ferritin C. Decreased export of Fe-S cluster proteins D. A & B E. All the above 8. What type of porphyria has an defect in uroporphyrinogen decarboxylase A. ALA dehydratase porphyria B. Acute intermittent porphyria C. Cogenital erythropoietic porphyria D. Porphyria cutanea tarda E. Lead poisoning 9. CO monoxide is : A. Metabolized in the liver B. Produced by the catabolism of heme C. When combined with hemoglobin lowers the affinity for O2 D. Excreted in urine E. Used in sensing hypoxia by depolarizing the membrane when levels are high 10. Which of the following statement is incorrect? A. Sideroblasts have iron-loaded mitochondria and are prone to apoptosis B. Iron must be in the ferric state to cross mitochondrial membrane C. Deposition of porphyrins in the skin cause photosensitivity D. Early-labeled peak of CO and bilirubin increases in the ineffective erythropoiesis E. Hemolytic states and ineffective erythropoiesis have increase rates of production of heme, CO, and bilirubin Metabolic Syndrome/Diabetes 1. What is the cause of Type 2 Diabetes? A. Beta cells in pancreas make too much insulin due to insulin resistance B. Beta cell becomes dysfunctional C. Beta cells are destroyed by autoimmune reaction D. A & B E. All the above 2. How does TZD work? A. Decreases insulin sensitivity in skeletal muscle by binding to PPAR γ B. Increases free fatty acids in circulation C. Inhibits activity of proinflammatory cytokines D. Enhances the expression of adhesion molecules E. Decreases the amount of adipocytes made in the body 3. Which of the following is not a risk factor for metabolic syndrome? A. Abdominal obesity B. Low HDL-cholesterol C. High LDL-cholesterol D. High blood pressure E. High fasting glucose 4. What is a symptom of diabetes? A. Thirst B. Frequent urination C. Glucose reacting with Hb (HB A1C) D. Glucose in urine E. All the above 5. A male patient has a fasting blood sugar between 100-125 with a waist circumference of 42 in. What is his diagnosis? A. Type I diabetes B. Hyperglycemia C. Pre-Type II Diabetes D. Type II Diabetes E. Normal 6. The atherogenic triad in Type II diabetes includes: I. High TG II. III. IV. Small LDL Large LDL Low HDL A. I, II, III B. I, III, IV C. I, II, IV D. II, III, IV 7. All the following occurs during insulin resistance except: A. Increased lipolysis in adipocytes B. Apo B stabilizes free fatty acids in the liver C. Lipoprotein lipase activity is increased D. CETP transfers triglycerides from VLDL to HDL E. Increase in small dense LDL-cholesterol leading to atheromas 8. Insulin resistance occurs by mechanisms of: A. Inflammatory response B. Fatty oxidation reduction C. Autoimmune reaction D. A & B E. All the above 9. Metformin has all the following effects on the body except? A. Decreases hepatic gluconeogenesi B. Activates AMP-activated protein kinase to upregulate insulin targets in skeletal muscle C. Reduces cardiovascular complications D. Decreases hyperglycemia E. None of the above Case studies in Anemia, Iron and Heme Metabolism 1. Which of the following is not true with Beta thalassemia? A. Excess alpha chains B. RBC hyperplasia C. Forming a β4 tetramer D. Iron-loading causing hemochromatosis E. Excess ferritin in plasma 2. `