Chest Pain
Intern Bootcamp 2015
Nathan Stehouwer, MD
Objectives: At the end of this
hour you will be able to…
Provide initial evaluation of a patient with chest
pain
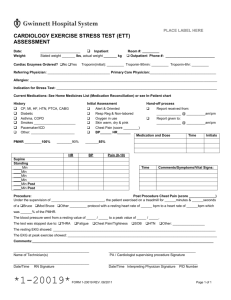
Know where to find key order sets
Locate old EKGs
List the initial management considerations for life
threatening causes of chest pain
Recite a few key pieces of Cleveland trivia
General approach:
First consider these…
Acute coronary syndromes
Pulmonary embolism
Aortic Dissection
Pneumothorax
Pericarditis with tamponade
Esophageal Rupture
Then take your time sorting out
these
Cardiac
MI
Pericarditis
Myocarditis
Aortic Stenosis
Vasospasm
Cocaine chest pain
Cardiac syndrome X
Stress cardiomyopathy
Pulmonary
PE
PNA
Asthma/COPD
Acute Chest Syndrome
Pleura
Pleuritis
Pneumothorax
Aorta
Dissection
Perforated ulcer
Chest wall
Costocondiritis/musculoskeletal
Sternitis
Tietze syndrome
Zoster
Esophagus
Esophageal Spasm
Eosinophilic Esophagitis
Esophageal Rupture/Perforation
GERD
Mediastinum
Mediastinitis
Mediastinal tumors
RUQ pathology
Pancreatitis
Hepatitis
Cholecystitis
choledocolithiasis
Panic attack
Typical vs. Atypical Chest Pain
Typical
Atypical
Characterized as
discomfort/pressure rather than
pain
Time duration >2 mins
Provoked by activity/exercise
Radiation (i.e. arms, jaw)
Does not change with
respiration/position
Associated with
diaphoresis/nausea
Relieved by rest/nitroglycerin
Pain that can be localized with
one finger
Constant pain lasting for days
Fleeting pains lasting for a few
seconds
Pain reproduced by
movement/palpation
Typical vs. Atypical Chest Pain
Cayley 2005
Tip:
ALWAYS have the patient point to
the pain!
The 1980 Cleveland Browns were
known by what nickname, after
winning multiple last-second
games?
Case 1
You are the orphan intern on Wearn team at 6PM. You
are called by the nurse because Ms. Z has developed
chest pain. Ms. Z is a 62 yo F with PMHx of CAD s/p
remote PCI to the LAD, COPD and right THA 3 weeks
ago who was admitted for a COPD exacerbation.
What would you do next?
Evaluation of Chest Pain
Case 1:
While on the phone: Ask nurse for most current
set of vital signs
Ask nurse to get an EKG
Obtain the admission EKG from the paper chart or
print baseline EKG from museweb
Go see the patient!
Evaluation of Chest Pain
Go to UH Portal->museweb and print
out an old EKG for comparison
Review prior discharge summaries
Extra prior
“0” before
MRN
Quickly review
cardiac work
up (9 digits total)
–echo, stress tests and cath reports
Go see the patient!
Sign in with: UHHS/username
and usual UH system password
Evaluation of Chest Pain
Once at bedside, determine if patient is stable or
unstable
Perform focused history and physical exam
Read and interpret the EKG. Compare EKG to old
EKG if available
If patient looks sick, has a convincing story, or has
concerning EKG findings, call your senior resident
for help/second opinion
Write a clinical event note
IF THE PATIENT APPEARS UNSTABLE OR VITALS ARE
CONCERNING, CALL A CODE WHITE!
Toolbox for workup of Chest Pain
EKG
CXR, unless patient clearly stable, having no dyspnea or
desats, and has pain that is clearly musculoskeletal or GI in
origin
Cardiac biomarkers, if patient has cardiac risk factors or
typical story
ABG, particularly if dyspneic or having desaturations
Therapeutic Trials (if you are not really sure)
Angina/ACS: try some sublingual NTG
GERD: Ranitidine, Maalox, BMX
Anxiety: anxiolytics
Costochondritis/MSK Pain: NSAIDs, ketorolac
Placement of patient: Telemetry/ICU?
Case 1
You go see the patient. She had been feeling better after
getting duonebs, but suddenly developed chest pain that is Lsided, 8/10 and worse with breathing. This pain is not like
her prior MI.
Vital signs: Afebrile, HR 120, BP 110/70, RR 28, O2 sat 89%
on 2L (was 95% on RA this morning)
Physical exam
Gen – in distress, using accessory muscles of respiration
Lungs – CTAB, no rales/wheezes
Heart – tachycardic, nl s1, loud s2, no mumurs, JVP at clavicle
sitting upright. Chest pain is not reproducible
Abd – soft, NT/ND, active BS
Ext – b/l LEs warm and well perfused
SKIN – no rash
What would you order next?
What is high on your differential?
Differential
Cardiac
MI
Pericarditis
Myocarditis
Pulmonary
PE
PNA
Asthma/COPD
Acute Chest Syndrome
Pleura
Pleuritis
Pneumothorax
Aorta
Dissection
Perforated ulcer
Chest wall
Costocondiritis/musculoskeletal
Esophagus
Esophageal Spasm
Eosinophilic Esophagitis
Esophageal
Rupture/Perforation
GERD
Mediastinitis
RUQ pathology
Panic attack
Case 1
Case 1
Modified Wells Criteria
Clinical symptoms of DVT (3 points)
Other diagnoses less likely than PE (3 point)
Heart Rate >100 (1.5 points)
Immobilization >/= 3 days or surgery within 4 weeks (1.5 points)
Previous DVT/PE (1.5 points)
Hemoptysis (1 point)
Malignancy (1 point)
Interpretation:
>6: high
2-6: moderate
<2: low
Or
>4: likely
</=4: unlikely
Diagnostic approach is simple if
you suspect PE…
Probability low: obtain D-DIMER
If positive: obtain CTPE
If negative: PE excluded
Probability moderate or high: obtain CTPE
Tests for PE
DDIMER: 95% sensitive, VERY nonspecific
ABG – Elevated A-a gradient fairly sensitive, highly
nonspecific
EKG – most commonly nonspecific changes (ST/T wave
changes, etc)
V/Q scan – helpful in patients with HIGH or LOW pretest
probabilities in whom a CTPE cannot be obtained (eg CKD)
LE Ultrasound: not sensitive to rule out PE
CTPE
Sensitivity 83%
Specificity 96%
Moderate - high clinical probability and positive CTPE: 92-96%
chance of PE
Pro Tip #2
A CT angiogram (important for evaluating for Pulmonary
Embolism or Aortic Dissection) requires EITHER:
1) At least a 20G peripheral IV
OR
2) A Power injectable central line
Case 1
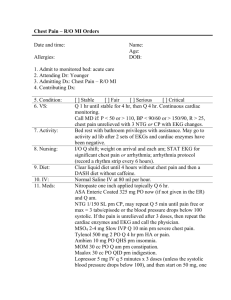
Acute Pulmonary Embolism
Management
Stabliize patient
oxygen
Fluids if hypotensive!
Anticoagulants
Preferred: LMWH or Fondaparinux
Enoxaparin 1.5mg/kg daily or 1mg/kg BID
Fondaparinux subcutaneous once daily (weight based)
Alternative: UFH (IV or SC) – select high intensity protocol
Hemodynamically unstable patients
High risk of bleeding (reversible)
GFR < 30
Can initiate warfarin on same day
IVC filter an alternative with mod-high bleeding risk
Search “enoxaparin
therapeutic”
Search “heparin infusion orders”
Pearl: If you have a moderate
or high suspicion of PE, you
can start anticoagulation while
awaiting full diagnostic workup
PE with hypotension
Thrombolysis
Administer over short infusion time
Catheter based thrombectomy/embolectomy
For failure of thrombolysis or likelihood of
shock/death before thrombolysis can take effect
(hours)
Surgical thrombectomy
Failure of above therapies
Who was the first African-American
player to play in the American
League, joining the Cleveland
Indians in 1947?
Larry Doby
Case 2
You are the long call intern on Hellerstein and
get a call to 67121 at 6:58PM. You have a new
patient in the ER, being admitted for ACS rule
out.
What’s your next move?
Evaluation of Chest Pain
Call to get report from ED physician about the
patient
Obtain most recent set of vital signs
Ask about EKG and CXR results
Ask what meds have been started in ER and how
patient responded
Case 2
Mr. M is a 67 yo man with of hypertension,
dyslipidemia, type II diabetes and coronary
artery disease s/p PCI in 2007. He presents
with new onset chest pain x 2 hours that is
retrosternal, 7/10, associated with nausea and
diaphoresis. Began 1 hour ago.
Case 2
VS: T 37 HR 108 BP 105/60 RR 20 O2 sat 93%
on RA
Physical exam:
Gen – uncomfortable from active chest pain,
diaphoretic
Lungs – crackles at bilateral bases
Heart – tachycardic, nl s1/s2, no mumurs or rub
Rest of the exam benign
Next Steps
Review EKG
Trial SL Nitroglycerin
Administer aspirin
Review CXR
Check Troponin
Case 2 Labs
CBC wnl
RFP wnl
Troponin = 0.05
Case 2
Case 2 Diagnosis: UA/NSTEMI
EKG changes in Acute Coronary Syndromes:
ST elevations
ST depressions
T wave inversions
“pseudonormalization” – inversion of previously inverted T
waves when compared with old EKG
New conduction block
Q waves
Importance of serial EKG monitoring: sensitivity of
single EKG is only 50% sensitive for acute MI
Just a reminder…
Don’t freak out! A positive troponin
does not necessarily equal ACS
Risk Stratification
Figure 2. Algorithm for risk stratification and treatment of patients with UA/NSTEMI.
Christopher P. Cannon, and Alexander G.G. Turpie
Circulation. 2003;107:2640-2645
Copyright © American Heart Association, Inc. All rights reserved.
UA/NSTEMI: Initial Management
“Stabilize” plaque
Dual antiplatelet therapy
Plavix load 600mg followed by daily 75mg
ASA 324mg chewable, then 81 daily
Anticoagulant
UF Heparin at low intensity protocol (order under Heparin Protocol)
Statin
Atorvastatin 80mg
Optimize Myocardial O2 supply/demand
Control HR -> Short acting metoprolol, can titrate quickly to HR
<60 if BP allows. Give 5mg IV, can repeat at 5-15min intervals.
Be wary of patients with heart failure!
Supplemental O2 if hypoxemic
SL nitroglycerin (0.4mg), repeat every 4-5 minutes
Morphine if still having active chest pain
Case 2 continued
You are now the nightfloat intern, and the
patient is signed out to you at 10PM. At
midnight, you are called for continued chest
pain. Improved from admission but still 5/10
severity.
Next steps
Vitals
Repeat EKG
Repeat SL nitro
Assess patient in person
Call your senior!
Dose additional morphine
start IV nitroglycerin after 3-4 doses of SL
nitroglycerin
Start 5 mcg/min
Increase by 5mcg/min every 20 minutes
Floor maximum: 30mcg/min
Pearl
Inability to ELIMINATE chest pain in a patient
with ACS using maximal medical therapy
=
Urgent call to cardiology for consideration of
immediate catheterization
Trivia
What typical ACS meds should you
NOT give this patient?
Pearl: Nitroglycerin contraindicated
in inferior MI
Other contraindications to NG:
Preload dependent states
Inferior MI
Aortic outflow obstruction (HOCM, severe AS)
Likelihood of hemodynamic instability
HR <50 or >100
SBP<90mmHg or more than 30mmHg below
baseline
Use of PGE inhibitors
What former Cleveland Public
Safety Director, famed for bringing
Al Capone to justice, has been
honored with his own Great Lakes
Brewing Co. beer?
Case 3
You are called on Hellerstein to admit a 65 yo man for ACS
rule out.
Mr Q is a gentleman with a history of DMT2, NASH, remote
NSTEMI, and HTN presenting with severe retrosternal chest
pain. Pain is different than prior MI but is very severe.
Radiates to neck. Began 3 hours ago; has subsided slightly
but is still 8/10 in severity.
You take report, quickly review
chart, and go to assess the patient
in the ER.
VS: T37.1, HR110, BP145/80 in R arm, RR16, Pox
98%RA
Focused Exam:
GEN: in discomfort but mentating well
HEENT mmm, JVP at clavicle
CV normal s1/s2, no murmurs
PULM ctab, no w/c/r
EXTR: cool
Bilateral BP: 145/80R, 110/60L
EKG identical to previous EKG which you printed
from portal
Thoracic aortic dissection
Diagnosis
CT angiography – first line
83-100% sensitive, specificity 87-100%
TEE – second line; good for proximal, cannot visualize
descending aorta well
MRI – useful for surveillance
Images:
reference.medscape.com
rwjms1.umdnj.eduen.wikipedia.org
en.wikipedia.org
Thoracic aortic dissection
Risk Factors
Hypertension
Atherosclerosis
Preexisting aneurysm (known history in 13% of patients)
Inflammatory conditions affecting aorta (Takayasu, Giant Cell
Arteritis, RA, syphilis)
Collagen disorders (Marfan, Ehlers-Danlos)
Bicuspid aortic valve
Aortic coarctation
Turner syndrome
History of CABG, AVR, Cardiac Cath
High intensity weight lifting
Cocaine use
Trauma
Excluding dissection
96% of patients have at least one of:
Abrupt onset thoracic or abdominal pain that is
sharp/tearing/ripping
Mediastinal widening
Variation in pulse or blood pressure >20mmHg
between left and right arms
D-DIMER has a good negative predictive value
in lower risk patients
Thoracic aortic dissection
Management
Type A
Surgery!
Do not delay surgery, even
for LHC
Beta blockers, titrate to HR
50-60 (labetalol, esmolol)
BP control (nitroprusside)
Type B
Beta blockers, titrate to HR
50-60 (labetalol, esmolol)
BP control – add
nitroprusside or similar agent
to SBP goal 100-120mmHg
Avoid Hydralazine
Surgery for those with end
organ damage or those who
do not respond to medical
therapy
Watch for hypotension – give
fluids if needed, consider
tamponade, MI, or rupture as
complications if hypotensive
What Cleveland DJ coined the
term “Rock and Roll” in 1952?
Case 4
You are on long call on VA Blue. You are called
to admit a 53 yo M from the ED for chest pain
and EKG abnormalities
PMHx:
HTN
Dyslipidemia
You go see the patient and he tells you that
he has had this chest pain for ~2 days, but
it has progressively gotten worse. His
chest pain is worse with breathing.
Case 4
VS: T 37.9 HR 104 BP 140/76 RR 20 O2 sat 95% on RA
Physical exam:
Gen – in mild distress due to chest pain, leaning forward while in
bed
Lungs – CTAB
Chest wall – no visible rash, chest wall NT to palpation
Heart – tachycardic, nl s1/s2, no rub
Rest of physical exam benign
Labs:
WBC = 14, RFP wnl, AMI panel x 1 = negative
CXR = negative
Case 4
EKG on admission:
Case 4 - Pericarditis
Refers to inflammation of pericardial sac
Idiopathic pericarditis typically preceded by
viral prodrome, i.e. flu-like symptoms
Classically, patients have sharp, pleuritic
chest pain relieved by sitting up or leaning
forward
Goyle 2002
Differentiation of ST elevations
Acute
Pericarditis
Acute MI
Benign Early
Repolarization
Diffuse ST
segment
elevation
ST elevation in anatomically
contiguous leads; possible
reciprocal ST depression
ST elevation
predominant in V2-V5,
may be widespread
ST elevations
concave
ST elevations convex
ST elevations concave
PR depression
No PR Depression
No PR Depression
T waves upright
T waves invert as infarction
evolves
T wave may be inverted
J point notching/slurring
Goyle 2002
Or, to put it more simply:
Scary
Not Scary
Case 4 - Pericarditis
Diagnostic criteria
UpToDate 2012
Case 4 – Pericarditis
Per 2003 ACC guidelines, all patients diagnosed with
pericarditis should receive echocardiogram
High risk features:
Fever and leukocytosis
Cardiac tamponade or a large pericardial effusion
Immunosuppressed state
Warfarin therapy
Acute trauma
Failure to respond to NSAIDS
Elevated cardiac troponin
Case 4 - Pericarditis
UpToDate 2012
Who was the first African-American
mayor of a major U.S. city, elected
by Cleveland in 1967?
Case 5
You are VA MICU intern, called to assess Mr. Jones. He is a
55 yro M with COPD admitted for exacerbation. On admission
he was given solumedrol, moxifloxacin, scheduled duonebs,
and placed on BiPAP due to CO2 retention.
He now is complaining of severe R sided chest pain, worse
with breathing.
Case 5
Case 5 - Pneumothorax
Management of Pneumothorax
100% O2 and observation in stable patients for
PTX < 3 cm in size
Needle aspiration in stable patients for PTX >3
cm
Chest tube placement if PTX >3 cm and if needle
aspiration fails
Chest tube placement in unstable patients
Tension Pneumothorax – don’t be afraid!
14G angiocath into 2nd intercostal space in
midaxillary line
Case 6
45 yo man with 3 days severe gastroenteritis presents with
worsening chest pain
Pain is 10/10, sharp, retrosternal, constant.
On exam, he is tachypneic, tachycardic and hypotensive.
Crepitus is palpated over anterior chest wall
Esophageal rupture
Precipitating events typically with positive intra-esophageal
pressure but negative intrathoracic pressure (ie retching)
Up to 25% have no history of vomiting
May be suggested by subcu emphysema or mediastinal
crackling on auscultation but these are insensitive and take
>1 hour to develop.
Can be noted by medistainal air on CXR but diagnosis is by
CT or contast esophogram
Esophageal rupture - treatment
Antibiotics
IV PPI
NPO
Surgical consultation
Drainage of fluid collections
Remove necrotic tissue
Consideration of surgical or endoscopic repair
Pearl
Great EKG Practice Site:
http://ecg.bidmc.harvard.edu/maven/mavenmain.asp