userfiles/140/my files/powerpoint presentations
advertisement
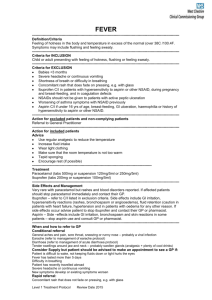
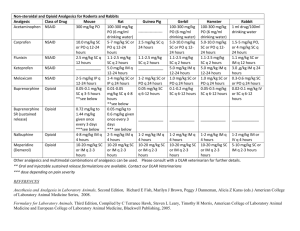
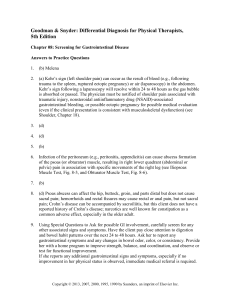
Pharmacology Application in Athletic Training History of Drugs and Pharmacy Around 2100 BC: Recorded references to drug therapy ~250 vegetables, 120 mineral drugs 1500 BC Egyptians: Ebers Papyrus 22yrd document: 700+ drugs listed 600-330 BC Greeks: developed pharmacopeias Defined preparation, action of drug,etc Middle Ages: Pharmacy recognized as a separate profession from medicine Early 20th Century - History of Drugs Virtually no laws to govern the sale of drugs Coca Cola: A tonic that contained cocaine Aid respiration and digestion Paregoric acid: Contained opium Given to teething babies U.S. History of Pharmacology 1646: 1st American Pharmacy 1821: Philadelphia College of Pharmacy 1852: American Pharmaceutical Association Begins 1870: American Pharmaceutical Assoc developed regulations U.S. Legal Foundations 1906: Food and Drug Act 1938: FDA and Food, Drug, and Cosmetic Act 1952: Durham-Humphrey Amendment 1962: Kefauver-Harris Amendment 1970: Poison Prevention Packaging Act 1970: Comprehensive Drug Abuse Prevention and Control Act 1984: Anti-Tampering Act 1992: “Fast-track” drug approval process Pure Food and Drug Act: 1906 Prohibits contamination & misbranding Ineffective: 1937: Sulfanilamide Elixir (oral anti-biotic) – liquid version contained diethlyene glycol (antifreeze) >100 people died FDA & Food, Drug, and Cosmetic Act: 1938 FDA = Food and Drug Administration Created in 1938 to enforce the Food, Drug and Cosmetic Act of 1938 ○ All drugs must be safe before marketed ○ Labels w/ warnings, strength/purity, & directions Ensure the safety of drug production, consumption, and distribution Drug companies must get approval by the FDA prior to marketing their drug products FDA regulates adverse drug reactions Durham-Humphrey Amendment: 1952 Distinction between prescription and OTC drugs Warning Label for Prescription Drugs: “Caution: Federal law prohibits dispensing without a prescription” Thalidomide Popular sleeping pill taken by pregnant women in Europe (1950’s) FDA refused to approve sale in US Thousands of children were born with seallike deformity Took 10 yrs to find connection www.thalidomide.ca Kefauver-Harris Amendment: 1962 In response to the Thalidomide tragedy Requires manufactures to test products for safety and efficacy Also required testing of drugs manufactured between 1938-1962 As a result, many were withdrawn from market Poison Prevention Packaging Act: 1970 Prevent the accidental poisoning of children Prescription drugs must be dispensed in child-resistant containers 80% of children under 5 must not be able to open the container 90% of the adults must be able to open the container Controlled Substance Act - 1970 Regulates distribution of drugs w/ potential for addiction/abuse Schedule: I – V Schedule I – most abuse potential Schedule V – least abuse potential Schedule I: Heroin, LSD Schedule II: Morphine, Dexedrine, Adderall, OxyContin, Demerol, Percocet, Ritalin Schedule III: Tylenol w/ Codeine, Vicodin Schedule IV: Darvocet, Valium, Ativan, Xanax, Ambien Schedule V: Robitussin A-C Anti-Tampering Act:1984 A number of people died in the 80’s after taking Tylenol laced with cyanide All OTC products must be sold with tamper-resistant packaging Plastic seal over cap or aluminum seal over opening FDA Drug Approval Process ~1/5000 drugs tested get to the market Around 12 yrs, costs millions of dollars Other countries may last 1yr and have lower standards 1992: FDA created “fast track” to decrease approval time for important therapeutic drugs Allows marketing before the last phase of clinical trials (safety and efficacy portion) Follow-up studies must be performed Unknown risks are balanced by urgent need for drug FDA Approval Process 1. 2. 3. Lab/Animal Studies (up to 3 yrs) Company files for investigational new drug Clinical Study: 1. Phase I: Human volunteers (1 yr) 2. Phase II: Human Patients (2 yrs) 3. Phase III: Human Patients (3 yrs) 4. 5. FDA Review (2-3 yrs) FDA Approval of New Drug (~12 yrs after initiation) Name of Drugs Chemical name N-acetyl-para- aminophenol Generic Brand name name Acetaminophen Tylenol® Brand vs Generic Brand-name drugs usually have a patent, granted by FDA, for 17 years After 17 yrs, other companies can make generic equivalent Generic drugs must have the same active ingredient, strength, & dosage as the brand name drug Generic drugs must be tested for safety & efficacy & produce the same therapeutic effects as the brand name drug Pharmacodynamics: how drugs affect the body Pharmacokinetics: does to the drugs what the body What is a Drug? A chemical that alters physiological functions by replacing, interrupting, or potentiating (enhancing) existing cellular functions Exp: Caffeine can produce a stimulating effect on the CNS by attaching to CNS receptors and overriding fatigue messages Drug Properties Drugs cannot give cells properties they do not already possess Drug-receptor interaction: drugs must bind to a receptor on a cell in order to produce an effect “Lock and key” analogy: Occasionally several drugs or “keys” can unlock a single receptor Definitions – a drug that binds to a receptor and produces an effect Antagonist – a drug that binds to a receptor but does not produce an effect (blocker) Threshold – lowest dose capable of producing an effect Max effect – greatest response produced regardless of the dose (efficacy will not increase) Efficacy - the capacity to illicit a response Potency – amount of drug needed to produce an effect Agonist Definitions – the force that makes two agents bind together Latency – “onset of action” – time required for a drug to produce an observable effect Therapeutic Index – range in which desired effects are produced (narrow therapeutic index drugs have more potential to cause toxicities) Duration of Action – period of a single dose drug response Affinity Half-life (T ½) The time required to reduce the amount of drug concentration in the body by 50% Helps to determine how frequently a drug should be administered Motrin ~ 4 hours Claritin ~ 15 hours Vicodin ~ 3-4 hrs Pharmacokinetics What does the body do to the drug? Absorption Distribution Metabolism Excretion Absorption Most drugs must be absorbed into the blood stream in order to get to the site of action Methods of administration: Sublingual Oral Intravenous Transdermal (topical) Inhalation Distribution Mouth GI Tract Bloodstream Liver Bloodstream (to entire body) Intravenous Administration Target site Metabolism Process of breaking down drugs to be eliminated from the body First pass metabolism: Oral drugs get absorbed in the gut, then travel to liver – part of the drug gets broken down Primary organ of metabolism = Liver Produces enzymes that break down drugs Not all active drugs will reach their target site Exp: Lidocaine, if given orally, will be completely broken down by the liver Excretion Primary organ of excretion = Kidney Water-soluble drugs easily excreted Too much vitamin C…flushed down the toilet Lipid-soluble drugs are reabsorbed Vitamins D,E,A,K: Fat-soluble, stored in liver, toxic in large quantities Factors that affect drug response Infants/Children Enzymes do not fully develop until12 y/o Older Adults Elderly have decreased kidney function Timing of Food Before, during, after meal Person’s weight (fat distribution) Anti-Inflammatory Meds Billion Dollar Industry Approximately 1% of US population uses NSAID’s daily 14,000 cases each year of GI toxicity based on 70 million NSAID prescriptions filled (1991) HS FB Study: 75% used NSAID’s in previous 3 mo Inflammatory Response Inflammation signals the start of the healing process 3 stages: Acute inflammation phase Repair-regeneration phase Maturation phase Within 48 hrs of injury, fibroblasts begin process of wound repair & collagen synthesis (‘glue’) Allows the influx of leukocytes and macrophages to the area Remove damaged tissues or foreign substances Acute vs Chronic Inflammation The initial inflammatory response is essential for the resolution of an injury Excessive edema and vascular damage can disrupt oxygen flow, which can lead to further tissue damage Injury Cycle Cellular injury signals the release of chemical mediators, which (mostly) cause vasodilation: Histamine Serotonin Leukotrienes Prostaglandins Thromboxanes (causes vasoconstriction and promotes clotting) Cell Membrane Disrupted/Damaged Phospholipids Released Block 2: NSAID’s block production of prostaglandins Arachidonic Acid Cyclooxygenase Lipooxygenase Prostaglandins/ Thromboxane Leukotrienes Inflammation Swelling Pain Inflammation (Respiratory) Block 1: Corticosteroids block production of arachidonic acid Block 3: Lipoox inhibitors block metab of arach acid to reduce inflam Leukotrienes Bronchoconstriction, attracts inflammatory cells Have no role with systemic anti-inflam medications Leukotriene Inhibitors: Currently used to treat asthma only Zyflo, Accolate, Singulair Prostaglandin Inhibits clotting Inhibits stomach acid secretion Stimulates the mucus lining of the stomach Fever If hypothalamus senses increase in prost, it will elevate body temp Uterine muscle contraction Contractions during birth Released at end of menstrual cycle to help shed uterine lining (causes pain) Thromboxane Promotes platelet aggregation (clot formation) Potent vasocontrictor History of NSAID’s Bark of Willow trees used for 2000+ yrs Late 19th century: chemists came up w/ aspirin Late 20th century: came up w/ aspirin derivative (NSAID’s) Same effects w/ less severe side-effects All NSAID’s inhibit cyclooxgenase activity Effects of each NSAID varies per person If one drug doesn’t work within 1-2 wks, try another Effects of NSAID’s All NSAID’s inhibit cyclooxgenase activity Effects of each NSAID varies per person If one drug doesn’t work within 1-2 wks, try another Cell Membrane Disrupted/Damaged Phospholipids Released Block 2: Arachidonic Acid Aspirin/NSAID Cyclooxygenase Prostaglandins/ Thromboxane Inflammation Swelling Pain Lipooxygenase Leukotrienes Inflammation (Respiratory) Aspirin Acetylsalicylic acid from bark of Willow tree 1st created by Bayer in 1899 Mechanism of action: blocks the activity of the cyclooxygenase enzyme Dose: ~3,000-5,000mg/day Aspirin – Side Effects Side-effects: 2-40% of patients Gastric bleeding, ulcers Prevention: take w/ food or use coated aspirin (buffering action) Prolonged bleeding times Inhibits thromboxane (promotes clotting) Irreversible bond w/ Cyclooxygenase Decreased platelet function last 4-6 days (life span of platelets) after aspirin intake ○ Since the bond is irreversible Aspirin – Reye’s Syndrome Rare condition: impairs mitochondrial function, leads to liver & brain damage Sx’s & Sy’s: vomiting, lethargy, delirium, hyperventilation, coma, seizures No definitive cause & effect Linked to aspirin intake in children w/ viral infections Prudent to DC aspirin in patients <18y/o w/ a viral infection NSAID’s Motrin ®, Advil ® = ibuprofen Aleve®, Naprosyn® = naproxen Relafen® = nabumetone Indocin® = indomethacin Mechanism of action: reversibly bind to COX (cyclooxgenase) Ibuprofen Most frequently used NSAID Includes advil, motrin, and nuprin Introduced OTC in 1985 Among the most beneficial NSAID in relieving pain assoc w/ dsymennorhea (~400mg every 6hrs) Still see decreased clotting due to thromboxane inhibition Ibuprofen Analgesic, antipyretic, anti-inflammatory Most popular NSAID/Lowest risk of GI sy (1015% DC) T1/2 = 2 hours Onset = 15-30 minutes Dose: 200-400mg every 4-6 hours 600mg every 6 hours 800mg every 8 hours Anti-inflam: 800-1000mg t.i.d (2,400-3,200/day) Should not exceed 3,200mg/day Naproxen Chemically similar to ibuprofen Better @ decreasing jt inflam Naproxen sodium concentrates in joint synovium 20% more potent than aspirin 2x’s more cases of GI bleeding than Ibuprofen Avail Doses: OTC: 220mg/Rx: 250, 375, 500mg T1/2: 12 hours Onset: 2-4 hours Dose: 375-500mg b.i.d Maximum daily dose = 1,000mg Ketorolac Only NSAID that can be used for IM, IV or oral use Has antipyretic & anti-inflam effects, but typically used as an analgesic 2002: 28/30 NFL teams used IM on game days for pain relief Pain relief potency similar to opiats w/o dependency issues Onset: 30-50 min Dose: 15-60 mg Side-effects limit its’ use (< 5 days) Renal failure, gastric lining damage, GI bleeding COX-2 Inhibitors 2001: Bextra came onto the market, followed by Vioxx & Celebrex 2004: FDA recalled Bextra - higher incidence of heart attack & stroke Vioxx was voluntarily withdrawn soon after Linked w/ increased risk of myocardial infarction by 300% Only Celebrex remains on the market w/ warning Side-Effects of NSAIDS GI = #1 - nausea, vomiting, stomach cramping, ulcers, intestinal bleeding Renal toxicity Hepatic failure CNS – headache, confusion, tinnitus Hypersensitivity reactions Decrease side-effects: Take w/ food and avoid abuse!!! NSAID Drug Interactions Taking NSAID’s w/ anti-coagulants, aspirin, corticosteroids, or ALCOHOL: Increase risk of serious GI pathology NSAID’s will diminish effects of antihypertensive meds Allergy Note Patient’s that have a known allergy to aspirin should avoid other NSAID’s They share a common chemical structure Recommend: Tylenol (acetaminophen) Acetaminophen Effective fever and pain reducer Anti-pyretic and analgesic Not an anti-inflam because it cannot inhibit cyclooxygenase No GI issues or prolonged bleeding time Abreviation: APAP Sometimes combined w/ other meds Percocet = oxycodone + APAP Mechanism of Action: acts directly onto the CNS Acetaminophen Dose: 325-650mg every 4 hrs Regular strength: 325 mg Extra strength: 500mg Maximum strength: 650mg Toxicity: 5,000mg/day 5,000-8,000mg/day for several days = severe liver damage/death Onset: < 1hr T ½ = 2 hours Duration: 4-6 hours Question A basketball player goes up for a rebound and gets his feet cut out from underneath him and hits his head on the court. He has a mild headache and no other symptoms. What would you give him for pain? Acetaminophen (Tylenol) or Ibuprofen (Motrin) Glucocorticosteroids Produced in the adrenal gland Inhibits phospholipase (beginning of cascade) Blocks both pathways Used to tx asthma, chronic inflammation, and juvenile rheumatoid arthritis Method of delivery: Oral, IM, US, E-stim Phonophoresis (US), iontophoresis (e-stim) Use of Corticosteroids in Sports Medicine No controlled studies to validate practices surrounding use Use in reducing inflam is controversial, but widely practiced by physicians Recommended: 2 wks between injections & no more than 3 injections @ each site Linked to collagen breakdown 10-14 days of “relative rest” after injection ’85 & ’08 articles Typically it’s 1-3 days of rest before full RTP Complications GI upset (oral) Immune system suppression Risk of infection Fat necrosis Tendon Rupture: most feared 1999 study found irreversible damage to muscle when used to tx muscle contusions Atrophy and decrease force generation Due to inhibition of inflammatory phase of healing Indications Bursitis Rheumatoid Arthritis Severe Osteoarthritis Elbow epiconylitis (tennis elbow) Plantar fasciitis De Quervain’s tenosynovitis Trigger finger Chapter 4 Muscle Spasm vs Spasticity Spasm: Loss of range of motion, increased pain, & involuntary tension Athlete is unable to completely relax muscle Typically result of trauma Pain-spasm-pain cycle: Increase in pain from muscle sent to CNS = increase in tension = pain Central-Acting Drugs Central-acting – works on the CNS Mechanism: Depression of CNS/Reduce CNS nerve impulses ○ Results in overall relaxation Sedative effect allows athlete to rest & the muscle to repair = decreased muscle spasm Typically combined w/ an analgesic (aspirin, Tylenol) Onset: 30-60 min Duration: Most 4-6 hrs, some 12-24 hrs Does not cure muscle injury, just relieves symptoms! Side-effects Drowsiness, Confusion, Lack of muscle coordination Will be unable to practice/compete while taking relaxants! Encourage athletes to DC as soon as they can function without them Headache, Dizziness, Blurry vision, Nausea, Vomiting Allergic reactions Addiction Watch for signs of abuse Most commonly abused drug by health-care professionals In combination with alcohol = death Increased sedative effect Chapter 5 Type II Oral Agents Stimulate insulin release or help the body with glucose uptake Taken Most once a day or just a.c. popular: Glucophage (Metformin) Beware of hypoglycemia Need to eat regular meals when on medication Insulin Subcutaneous injection Upper arm, thigh, abdomen, buttocks Insulin pump More precise College & HS athletes have played sports w/ pump ○ Precautions must be taken to protect pump for contact sports Doses are individualized to the person Four types of insulin: Rapid acting: <15min a meals Short acting: 30-60min a meals Intermediate: b.i.d Long acting: once daily Chapter 7 Asthma Medications “Rescue inhalers” – broncodilators Rescue or control Corticosteroids – controls inflammation Controlling Agent Athletes should have a controlling agent for inflam & a rescue inhaler for broncoconstriction Albuterol Inhaler Bronchodilators Target Beta-2 agonists in bronchial smooth muscle specifically, causing them to relax Works within minutes, Most commonly used only lasts ~4 hrs Brand Names: Ventolin HFA® Proventil HFA® Proair HFA® 2 puffs: 30 min a exercise to prevent onset of sx Used as “rescue” inhaler, as needed Proper Inhaler Use 1) 2) 3) 4) 5) 6) Shake the albuterol inhaler Breath out deeply Place mouth piece to your mouth Press the canister down at the same time you breath in Hold breath for about 10 sec, or as long as you can Wait 1 min before repeating Anti-inflammatory Medications Corticosteroids: used to prevent inflammation associated w/ chronic asthma Not used as rescue therapy Advair®: Combine corticosteroids w/ long acting beta-2 agonist Must be taken everyday to work properly & prevent asthma attacks Corticosteroid Medications Corticosteroid: Flovent ® – fluticasone Asmanex ® – mometasone Pulmicort ® – budesonide Corticosteroid w/ Beta-2 Agonist: Advair ® – fluticasone + salmeterol Other Types Prednisone: Tablets or liquid Short tx course to reduce inflam p an attack ○ ~ 5 days Singulair: Disrupt the ability of leukocytes to increase inflammation Oral tablets Treatment for Asthma Attack Stay calm 2) Have them in a sitting position 3) Let them use their inhaler: 3-4 puffs 4) Talk to them, encourage them to control their breathing 5) If no improvement in ~ 30 min, call 911 1) 1) Only call 911 if sy’s don’t respond to medicine 6) 7) Keep using the albuterol inhaler every 20 min for up to 1 hr If they pass out, use mouth to mouth Antihistamine - Allergies 1st Generation: Benadryl (Night time) 4-6 hrs sx relief Cause drowsiness Dry mouth 2nd Generation: Claritin, Zyrtec, Allegra (Day time) Up to 12 hrs sx relief Less drowsiness Nasal Decongestant (+ psuedoephedrine): ○ Claritin-D & Allegra-D Steroidal Nasal Sprays (RX only) Used specifically for allergic rhinitis Not effective for viral conditions (common cold) Effective for decreasing nasal congestion, sneezing, & rhinorrhea Few side effects due to their direct action Epistaxis, nasal irritation, dryness Flonase Nasonex Expectorants vs Antitussives Ingredients in cough syrups Expectorant: Promotes removal of mucus from airway Productive cough: Guaifenesin Exp: Mucinex, Robitussin Chest Congestion Antitussive: Suppress action of coughing Dry cough: Dextomethorphan (DM) ○ DM is most common ingredient in cough syrup OTC’s Exp: Robitussin, Tylenol Cold products, & NyQuil Chapter 9 Antibiotics Used to treat bacterial infections Choice of antibiotic is based on type of bacteria Narrow-spectrum: target specific microorganisms Broad-sprectrum: active against many categories of bacterial microorganisms Bacteriocidal: kills bacteria Bacteriostatic: prevents multiplication Tests for Bacteria Gram stain test: identifies the type of bacteria Blue: Staphylococcus, Streptococcus Red/Pink: E. Coli, Salmonella Disk-Diffusion & Broth Dilution: assess drug sensitivity Antibacterial Drugs Mechanisms of action: Inhibit cell wall synthesis Inhibit protein synthesis Inhibit DNA synthesis Inhibit folic acid synthesis Penicillin Inhibits cell wall synthesis 1928 – discovered by Alexander Fleming He noticed mold growing in a petri dish of bacteria The bacteria were dying as they came in contact with the mold Thus, penicillin was discovered Penicillin Passes through small pores in the bacteria’s cell membrane & binds to penicillin-binding proteins (PBP) Penicillin inhibits enzymes needed to construct the bacteria’s cell wall Without the cell wall, the bacteria loses its’ protection & gets broken down Since human cells do not have a cell wall, the penicillin does not affect our own cells Penicillin Structure All penicillin’s have same basic chemical structure: beta lactam ring The ring is very weak Some bacteria produce an enzyme: beta lactamase that cleaves the ring structure and inactivates the antibiotic Penicillin Drugs Penicillin VK Amoxicillin Methicillin Used primarily to Strep throat Pneumonia Skin infections Ear infections tx: Penicillin Allergy One of the most commonly reported drug allergy is penicillin Mild reactions: Rash, itching, hives, swelling Severe reactions: Bronchospasm, laryngeal edema MRSA Methicillin Resistant Staphylococcus Aureus “Superbug” Resistant to beta-lactam antibiotics Methicillin, Penicillin, and Amoxicillin Cephalosporins – Exp: Keflex (Cephalexin) – 1st Gen. Four generations: tx different types of bacteria Inhibits bacteria cellular wall synthesis Have a beta lactam ring, similar to penicillin Also susceptible to beta-lactamase producing bacteria Many pt’s w/ pen. allergy can take cephalosporins Used to tx: Skin & soft tissue infections, respiratory tract infections, & meningitis Inhibit Protein Synthesis Binds to bacterial ribosomes & block production of amino acids Suppress bacteria growth Classes: 1. Tetracyclines 2. Macrolides 3. Clindamycin 4. Aminoglycosides Tetracyclines Broad spectrum antibiotic Effective against wide variety of conditions: Lyme disease Acne Tooth infections Pneumonia, respiratory infections Chlamydia, gonorrhea, syphilis Macrolides Similar coverage as penicillins: Pneumonia, strep, skin infections, chlamydia, syphilis Can be used in patients w/ penicillin allergy Exp: Erythromycin Clarithromycin Azithromycin (Z-Pak) Clindamycin Only agent in its class Used to treat wide variety of infections: Pneumonia, respiratory track infections, skin infections, acne Inhibit Folic Acid Synthesis “Sulfa” drugs Bactrim (sulfamethoxazole) Suppress bacteria growth Mostly used for UTI’s Caution in patients w/ sulfa allergy Most common side effect is hypersensitivity Minor Skin Infections: OTC Topical Anitbiotics 1. Bacitracin: Bacitracin zinc: inhibits DNA synthesis 2. Triple Antibiotic & Neosporin: Polymyxin B sulfate: inhibits cell wall Neomycin sulfate: inhibits protein synthesis Bacitracin zinc: inhibits DNA synthesis Viral Infections & Vaccines Vaccine available: Polio Small pox, chicken pox, shingles Rabies Measles, Mumps, Rubella (MMR) Hepatitis A, B, D HPV Flu (yearly) No Vaccine available: Common cold, HIV, Mono, Herpes simplex, Hepatitis C, E, F, G Chapter 10 Pain Management Severity of Pain Drug Use to moderate NSAID’s or acetaminophen Moderate to Severe Low dose Opioid Severe High dose Opioid plus nonopioid Mild Analgesics - Opioids Derived from opium poppy plant Morphine & codeine (most common) Heroin can be extracted w/ further processing No medically accepted use Can cause severe psychological & physical dependence Common Uses: Cancer patients Surgery Severe trauma Opioid Mechanism of Action Decreases neurotransmitter activity Which produces analgesic effect All opioid drugs are considered controlled substances Class I (Street drug): Heroin Class II (Highest level of abuse): Morphine, Oxycodone (Percocet®) Class III (Moderate potential for abuse): Hydrocodone ○ Vicodin®, Lortab® Hydrocodone Hydrocodone c acetaminophen Most commonly prescribed pain medicine in 2000 Vicodin & Lortab Time to Onset: 10-30min Duration: 4-6hrs Oxycodone Typical Brand Names: Oxycontin Percocet Percodan Oxycodone Time to Onset: 15-30min Duration: 4-6hrs Percocet: Oxycodon + Acet Doses: 5/325 mg (5 mg oxycodone + 325mg APAP) 7.5/325 10/650 Take 1 tablet every 4-6 hours as needed for pain Can be taken c or w/o food Don’t exceed 4g/day (4000mg) limit for acetaminophen Codeine Exp: Tylenol #3: 3mg codeine + 300mg APAP Uses: Mild to moderate pain or dental use Sometimes used as an antitussive for individuals w/ a severe cough Time to Onset: 10-30min Duration: 4-6hrs Codeine can be further processed into morphine Morphine One of the most effective drugs known for pain relief Used to treat moderate to severe pain Can also be used to alleviate severe coughing Morphine may be used to ease pain before, during & after surgery Can cause psychological & physical dependence With the same addiction potential as heroin Time to Onset: 15-60min Duration: 3-7hrs Side Effects Addiction Sedation Nausea/Vomiting Constipation CNS/Respiratory Depression Combined c alcohol can be lethal! Local Anesthetics To induce a partial or complete loss of sensation Ice, injection of drug, topical (skin irritants) Action of Drug: Diminishes ability of the nerve fiber to conduct an action potential Inhibits number of nerve endings that can transmit impulses to CNS Commonly Used Local Anesthetics Novocaine: Onset: 10-30 min Duration: 30-60 min Lidocaine: Onset: <10 min Duration: 1-3 hrs Cocaine: Still used (rarely) during nasal surgeries Warning Using pain relievers or local anesthetics during sports participation may cause further injury!