Collaborative Staging for Colon Cases
advertisement

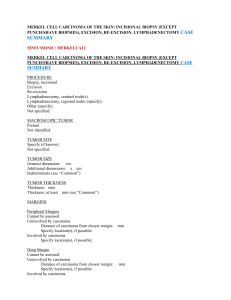
Nicole Catlett, CTR KCR Abstractor’s Training April 21-23, 2015 1 Discussion about collaborative staging data items: Tumor Size Extension Tumor size/Extension Eval Lymph Nodes Lymph Node Eval Mets @ DX Mets Eval 2 General Rules: 1. Code largest primary tumor size documented. 2. Code primary tumor size from pathology report when patient has a resection. 3. Code largest primary tumor size prior to neoadjuvant treatment unless tumor is more extensive after treatment. 4. Code largest primary tumor size from radiology or endoscopy when no surgery is performed. 3 Record the tumor size in millimeters You will convert cm to mm by multiplying by 10 4 Pathology report states: 3.9 cm mucinous adenocarcinoma located in the cecum. CSTS = Colonoscopy states: 6 cm tumor in the sigmoid colon suspicious for malignancy. CSTS = 5 Do not code the size of a polyp, cyst or ulcer, only the size of the cancer. EXAMPLE #1: Pathology report states tubulovillous adenoma 2 cm in size. Size of invasive carcinoma: 1.1 cm CSTS = ? Answer: 011 EXAMPLE #2: Pathology report states 1.9 cm tubular adenoma with foci of adenocarcinoma. (HINT: review tumor size extension table) CSTS = ? Answer: 990 Foci 6 Rounding rules for coding tumor size when described in fractions of millimeters. EXAMPLES: 1. Tumor 3.7 mm = 004 mm 2. Tumor 0.9 mm = ? Answer = 001 3. Tumor 5.1 mm = ? Answer = 005 NOTE: If the tumor size is a fraction of a millimeter you will round up to 1 mm, you will not round down Example: Tumor 0.3 mm = 001 mm. 7 Using “stated as” codes EXAMPLES: Tumor stated to be “between 4 and 5 cm CSTS = 995 Tumor stated to be less than 1 cm CSTS = ? Answer: 991 8 General Rules 1. Code the farthest tumor extension documented. 2. Code pathologic tumor extension when patient does not receive neoadjuvant treatment. 3. Code clinical tumor extension when patient does receive neoadjuvant treatment unless the tumor extension is worse after neoadjuvant treatment then you use pathologic extension. 4. Code tumor extension based on list of ambiguous terms to be used to determine involvement. 9 The complete list of ambiguous terminology that can be used to determine involvement are listed on page 23 of Section I, Part I of CS manual. 10 SOME TERMS THAT CAN BE USED: - Compatible with - Consistent with - Favors - Most likely - Probable - Presumed - Suspected - Suspicious SOME TERMS NOT TO BE USED: - abuts - approaching - attached - encased/encasing - equivocal - possible - questionable - worrisome 11 Identifies contiguous growth (extension) of the primary tumor within the organ of origin or its direct extension into neighboring organs. When coding tumor extension you are documenting the depth of tumor invasion through the colon wall layers. Now lets take a look at the colon layers 12 Layers from inside out… Lumen (interior surface of colon "tube") Mucosa Surface epithelium Lamina propria or basement membrane— dividing line between in situ and invasive lesions Muscularis mucosae 13 Submucosa—lymphatics; potential for metastases increases Muscularis propria Subserosa—sometimes called pericolic fat, subserosal fat, mesenteric or retroperitoneal fat Serosa—present on ascending, transverse, sigmoid only (also called the visceral peritoneum) SEER Training Modules, Colon Module, U. S. National Institutes of Health, National Cancer Institute, 1/13/12. <http://training.seer.cancer.gov/>. 14 SEER Training Modules, Colon Module , U S National Institutes of Health, National Cancer Institute. 1/13/12 <http://training.seer.cancer.gov/>. 15 Lets review the CS Extension codes located in the extension table: 000 In-situ, intraepithelial, noninvasive 050 Adeno(carcinoma), noninvasive in a polyp or adenoma 100 Invasive tumor confined to mucosa, nos including intramucosal, nos (pTis) 110 Invasive tumor confined to lamina propria, including lamina propria in the stalk of a polyp 16 120 Confined to and not through muscularis mucosae, including muscularis mucosae in a polyp 130 Confined to head of polyp, NOS 140 Confined to stalk of polyp, NOS 150 Invasive tumor in polyp, NOS 160 Invades submucosa (superficial invasion), including submucosa in stalk of polyp 170 Stated as T1 with no other information 17 18 200 Invasion of muscularis propria OR stated as T2 with no other information 19 20 400 Extension through wall, NOS, Invasion through muscularis propria or muscularis, NOS, Subserosal tissue/(sub)serosal fat invaded, Transmural, NOS, Wall, NOS 450 Extension to: Adjacent tissue(s), NOS Connective tissue Mesenteric fat Mesentery Pericolic fat 21 458 Extension to fat, NOS 470 Stated as T3 with no other information 22 23 500 Invasion of/through serosa (mesothelium) (visceral peritoneum); Tumor penetrates to surface of visceral peritoneum 550 500 + (450, 458) *COMBINATION CODE* 560 Stated as T4a with no other information 565 Adherent to other organs or structures clinically with no microscopic examination OR Tumor found in adhesion(s) if microscopic examination [T4b] 24 25 570 Adherent to other organs or structures, NOS 600 Greater omentum, small intestine (*site specific) 655 Abdominal wall or retroperitoneum (excluding fat) *except sigmoid which is code 675 660 Kidney or ureter *see note about sites applicable 700 Fallopian tube or Ovary or Uterus 750 Adrenal (suprarenal) gland Bladder Diaphragm, Fistula to skin Gallbladder Other segment(s) of colon/rectum via serosa 26 800 Kidney Liver Ureter Other contiguous extension 850 Stated as T4b with no other information 900 Stated as T4 [NOS] with no other information 950 No evidence of primary tumor 999 Unknown Extension not stated Primary tumor cannot be assessed Not documented in patient record 27 Coding extension examples: Your path report states “invasion of muscularis propria into the pericolic fat with extension to serosal surface”. What code would be used? CSEXT = 550 Pathology report states “invasion through the bowel wall”. What code would be used? CS EXT = 400 28 This field is used primarily to derive the staging basis for the T category in the TNM system. In most circumstances it records how the codes for the two items “CS Tumor Size” and “CS Extension” were determined, based on the diagnostic methods employed. 29 Instructions for coding: 1. Document the staging basis for the farthest extension and/or greatest tumor size. The underlying purpose of this field is to capture the staging basis for the highest T category assigned to the case. In most circumstances, this will be the staging basis for the highest Tumor Size code or Extension code as appropriate to the site. In coding colon cancer the extension code is used to derive the T category. 30 Clinical Code 0 (c) Physical Exam Imaging (CT, MRI, PET) Other non-invasive methods of examining tissues 31 Clinical code 1 (c) Scopes Observations at surgery Diagnostic biopsies 32 Pathologic Code 3 (p) Based on surgical resection (no or unknown prior neoadjuvant treatment) OR Based on biopsy that determines the highest T or N category 33 Clinical Code 5 (c) Neoadjuvant treatment received Clinical evidence unless pathologic evidence is more extensive than clinical 34 Pathologic Code 6 (yp) Neoadjuvant treatment AND pathologic evidence at Surgery is more extensive than clinical evidence before treatment Neoadjuvant therapy given, pathologic evidence available, clinical evaluation prior to neoadjuvant therapy not available 35 Autopsy Code 2 (p) - Autopsy performed - Prior knowledge of malignancy (suspected OR diagnosed) Autopsy Code 8 (a) - Autopsy performed - Malignancy diagnosed at autopsy with no prior knowledge of malignancy (unsuspected OR undiagnosed) 36 Clinical Code 9 (c) Unknown - Unknown how T, N or M determined - Defaults to clinical (c) 37 Example #1 You have a CT scan showing a 8.4 cm lesion located in the cecum with stranding seen in the mesenteric tissue. The patient underwent a colonoscopy that showed adenocarcinoma. A colon resection was performed showing the cancer extended through the muscularis propria into pericolic adipose tissue. What is the Tumor Size? What is the Extension Code? What is the TS/EXT eval? 38 Example #2 A patient undergoes a screening colonoscopy and a large mass was seen in the cecum which was biopsied showing adenocarcinoma. The patient then had a CT scan of abdomen & pelvis showing a mass in cecum measuring 72 mm consistent with patient’s known history of newly diagnosed colon cancer. There is associated bowel wall thickening and stranding in adjacent mesentery, suspicious for invasion. The patient refused any other workup. What is the Tumor Size ? What is the Extension code ? What is TS/EXT Eval ? 39 40 This field identifies the regional lymph nodes involved with cancer at the time of diagnosis. Record the specific involved regional lymph node chain(s) farthest from the primary site. The lymph nodes may be involved by tumor either clinically or pathologically. Record the highest applicable code in the following order: pathology report, imaging, physical exam. 41 Pathologic information takes precedence. If there is a discrepancy between clinical information and pathologic information about the same lymph nodes, pathologic information takes precedence if no preoperative treatment was administered. It is not necessary to biopsy every lymph node in the suspicious area to disprove involvement. Example: Mesenteric lymph nodes stated as “suspicious for involvement” on CT scan. After colon resection all lymph nodes are negative. Code CS Lymph Nodes as 000, no regional lymph node involvement. 42 Inaccessible lymph nodes rule for regional lymph nodes. For inaccessible lymph nodes, record CS Lymph Nodes as Code 000 (None) rather than Code 999 (Unknown) when the following three conditions are met: 1. There is no mention of regional lymph node involvement in the physical examination, pretreatment diagnostic testing or surgical exploration. 2. The patient has clinically low stage (T1, T2, or localized) disease. 43 Note: Code 999 can and should be used in situations where there is reasonable doubt that the tumor is no longer localized and there is no documentation of involved regional lymph nodes 44 45 Segment Regional Lymph Nodes Cecum - Pericolic, anterior cecal, posterior cecal, ileocolic, right colic Ascending colon - Pericolic, ileocolic, right colic, middle colic Hepatic flexure - Pericolic, middle colic, right colic Transverse colon - Pericolic, middle colic Splenic flexure - Pericolic, middle colic, left colic, inferior mesenteric Descending colon - Pericolic, left colic, inferior mesenteric, sigmoid 46 Segment Regional Lymph Nodes Sigmoid colon - Pericolic, inferior mesenteric, superior rectal, superior hemorrhoidal, sigmoidal, sigmoid mesenteric Rectosigmoid - Perirectal, left colic, sigmoid mesenteric, sigmoidal, inferior mesenteric, superior rectal, superior hemorrhoidal, middle hemorrhoidal Rectum - Perirectal, sigmoid mesenteric, inferior mesenteric, lateral sacral, presacral, internal iliac, sacral promontory (Gerota's) superior hemorrhoidal, inferior hemorrhoidal Anus - Perirectal, anorectal, superficial inguinal, internal iliac, hypogastric, femoral, lateral sacral 47 000 No regional LN involvement 050 TD in the subserosa, mesentery, or nonperitonealized pericolic or perirectal tissues WITHOUT regional nodal metastasis Stated as N1c with no other information on regional 110 Regional lymph nodes: Colic (NOS) Epicolic (adjacent to bowel wall) Mesocolic (NOS) Paracolic/pericolic Nodule(s) or foci in pericolic fat/adjacent mesentery/mesocolic fat 48 210 Regional lymph nodes, for specific colon sites 300 Mesenteric, NOS Regional lymph node(s), NOS 410-480 Stated as pathologic N1 with no other information on regional lymph nodes 49 800 Lymph nodes, NOS 999 Unknown; regional lymph nodes not stated Regional lymph nodes cannot be assessed Not documented in patient record 50 Example #1 A patient presents with abdominal distention and pain. A CT of abdomen and pelvis is performed and shows descending colon mass with regional lymph node metastasis. What code would you use for CSLN? Answer: CSLN = 300 regional lymph nodes, nos 51 Example #2 A patient underwent a screening colonoscopy where a transverse colon cancer was identified and biopsy shows Adenocarcinoma. The patient had surgery and the path report has 15/15 positive pericolic lymph nodes. What is the code for CSLN? Answer: CSLN = 110 52 This field is used primarily to derive the staging basis for the N category in the TNM system. It records how the code for the item “CS Lymph Nodes” was determined, based on the diagnostic methods employed and their intent. Document the farthest involved regional nodes. Select the CS Lymph Nodes Eval code that identifies the type of report or procedure from which the information about the farthest involved regional lymph nodes was obtained. 53 Clinical Code 0 (c) Physical Exam Imaging (CT, MRI, PET) Other non-invasive methods of examining tissues 54 Clinical code 1 (c) Endoscopic exam Observations at surgery Diagnostic biopsy 55 Pathologic Code 3 (p) Based on surgical resection (no or unknown prior neoadjuvant treatment) OR Based on biopsy that determines the highest N category 56 Clinical Code 5 (c) Neoadjuvant treatment received Clinical evidence unless pathologic evidence is more extensive than clinical 57 Pathologic Code 6 (yp) Neoadjuvant treatment AND Pathologic evidence at Surgery is more extensive than clinical evidence before treatment Neoadjuvant therapy given, pathologic evidence available, clinical evaluation prior to neoadjuvant therapy not available 58 Autopsy Code 2 (p) - Autopsy performed - Prior knowledge of malignancy (suspected OR diagnosed) Autopsy Code 8 (a) - Autopsy performed - Malignancy diagnosed at autopsy with no prior knowledge of malignancy (unsuspected OR undiagnosed) 59 Clinical Code 9 (c) Unknown - Unknown how T, N or M determined - Defaults to clinical (c) 60 Example #1 Patient comes to ER with abdominal pain, bloating and rectal bleeding. A CT abdomen/pelvis is performed which shows colon cancer with pericolic lymph node involvement as well as liver metastasis. What is the CSLN code? Answer: 110 pericolic LNs What is the LN eval code? Answer: 0 clinical per CT 61 Example #2 Patient was found to have colon cancer after undergoing a screening colonoscopy. Surgery was performed. Path report says ascending colon adenocarcinoma with involvement of 10 out of 15 lymph nodes. What is the code for CSLN ? Answer: 300 regional lymph nodes, nos What is the LN eval code ? Answer: 3 pathologic 62 Description This field records the exact number of regional lymph nodes examined by the pathologist and found to contain metastases. Based on pathologic information only. This field is to be recorded regardless of whether the patient received preoperative treatment. Record the total number of regional lymph nodes removed and found to be positive by pathologic examination. The number of regional lymph nodes positive is cumulative from all procedures that remove lymph nodes through the completion of surgeries in the first course of treatment. 63 Use of code 95. Use code 95 when the only procedure for regional lymph nodes is a needle aspiration (cytology) or core biopsy (tissue). Use code 95 when a positive lymph node is aspirated and there are no surgically resected lymph nodes. 64 Definition of code 97. Use code 97 for any combination of positive aspirated, biopsied, sampled or dissected lymph nodes if the number of involved nodes cannot be determined on the basis of cytology or histology. 65 Use of code 98. Code 98 may be used in several situations. a. When the assessment of lymph nodes is clinical only. b. When no lymph nodes are removed and examined. c. When a “dissection” of a lymph node drainage area is found to contain no lymph nodes at the time of pathologic examination. d. If Regional Nodes Positive is coded as 98, regional Nodes Examined is usually coded 00. 66 Use of code 99. Use code 99 if it is unknown whether regional lymph nodes are positive. 67 This field records the total number of regional lymph nodes that were removed and examined by the pathologist. Based on pathologic information only. This field is to be recorded regardless of whether the patient received preoperative treatment. Cumulative nodes removed and examined. Record the total number of regional lymph nodes removed and examined by the pathologist. The number of regional lymph nodes examined is cumulative from all procedures that removed lymph nodes through the completion of surgeries in the first course of treatment. 68 Use of code 95. Use code 95 when the only procedure for regional lymph nodes is a needle aspiration (cytology) or core biopsy (tissue). Definition of “sampling” (code 96). A lymph node “sampling” is removal of a limited number of lymph nodes. Other terms for removal of a limited number of nodes include lymph node biopsy, berry picking, sentinel lymph node procedure, sentinel node biopsy, selective dissection. Use code 96 when a limited number of nodes are removed but the number is unknown. 9. Definition of “dissection” (code 97). A lymph node “dissection” is removal of most or all of the nodes in the lymph node chain(s) that drain the area around the primary tumor. Other terms include lymphadenectomy, radical node dissection, lymph node stripping. Use code 97 when more than a limited number of lymph nodes are removed and the number is unknown. 69 This field identifies the distant site(s) of metastatic involvement at time of diagnosis. Use highest applicable code. Assign the highest applicable code for metastasis at diagnosis, whether the determination was clinical or pathological and whether or not the patient had any preoperative Systemic therapy. Progression of disease. Metastasis known to have developed after the extent of disease was established (also referred to as progression of disease) should not be recorded in the CS Mets at Dx field. 70 Coding 00 versus 99 Record CS Mets at Dx as Code 00 (None) if there is no clinical or pathologic evidence of distant metastases and the patient is not treated as if metastases are present or suspected. This presumes that there are no distant metastasis that would otherwise alter the treatment approach. Code 99 may be used in situations where there is reasonable doubt that the tumor is no longer localized and there is no documentation of distant metastases. Note that code 99 maps to MX in sixth edition and cM0 in seventh edition. 71 00 No distant metastasis 08 Metastasis limited to a single distant lymph node chain: For cecum, ascending, hepatic flexure and transverse colon: Superior mesenteric lymph nodes 16 Metastasis limited to a single distant lymph node chain: For all colon sites: Common iliac Distant lymph node(s), NOS External iliac Para-aortic Retroperitoneal 18 Metastasis limited to a single distant lymph node chain, 72 26 Metastasis limited to a single distant organ except peritoneum 27 Stated as M1a with no other information on distant metastasis 31 Metastases to a single distant lymph node chain listed in code 08 and to a single distant lymph node chain listed in code 16 OR Multiple distant lymph node chains listed in code 16, with or without distant lymph nodes listed in code 08 33 Metastases to multiple distant lymph node chains, NOS 73 36 Metastases to more than one distant organ except distant lymph node(s) Metastasis to peritoneum Carcinomatosis 45 (26 or 36) + any of (08, 16, 18, or 31) Metastases to distant organs plus distant nodes 48 Stated as M1b with no other information on distant metastasis 74 60 Distant metastasis, NOS Stated as M1 [NOS] with no other information on distant metastasis 99 Unknown; distant metastasis not stated Distant metastasis cannot be assessed Not documented in patient record 75 Example #1 CT scan that shows evidence of liver metastasis. What is METS at DX code? ANSWER: 26 (single distant organ) Example #2 CT scan shows evidence of carcinomatosis. What is METS at DX code? ANSWER : 36 (carcinomatosis) 76 This field is used primarily to derive the staging basis for the M category in the TNM system. It records how the code for the item “CS Mets at Dx” was determined based on the diagnostic methods employed. Document the highest code in CS Mets at Dx. The primary use of the CS Mets Eval field is to assign a “c” or “p” to the M category derived from the CS Mets at Dx field. Since both clinical and pathologic evidence might be available for assessing distant metastasis, the coding of the Eval field can be confusing. The goal is to assign the Eval code that indicates the best evidence used to determine the M category. 77 Mapping of M1 subcategories. If a specific subcategory of M1 will be derived (such as M1a), determine if there was any pathological evidence for the specific subcategory. If so, select an Eval code that will derive a “p” staging basis. If there was only clinical evidence of the subcategory disease, select an Eval code that will derive a “c” staging basis. 78 Eval code 0 Does not meet criteria for AJCC pathologic staging of distant metastasis: Evaluation of distant metastasis based on physical examination, imaging examination, and/or other noninvasive clinical evidence. No microscopic examination of metastatic specimen performed or microscopic examination was negative. This will derive a clinical M. 79 Eval code 3 Meets criteria for AJCC pathologic staging of distant metastasis: Specimen from metastatic site microscopically positive WITHOUT pre-surgical systemic treatment or radiation OR specimen from metastatic site microscopically positive, unknown if pre-surgical systemic treatment or radiation performed OR specimen from metastatic site microscopically positive prior to neoadjuvant treatment 80 Examples: Cecum carcinoma with lung metastases on chest X-ray and positive liver biopsy. CS Mets at Dx is coded 36 (Metastases to more than one distant organ), which maps to M1b. Code CS Mets Eval as 0, which maps to the “c” staging basis because only one organ/site was microscopically proven. Sigmoid adenocarcinoma with liver metastases on ultrasound and positive peritoneal nodule biopsy. CS Mets at Dx is coded 36 (Metastasis to peritoneum). Code CS Mets Eval as 3, which maps to the “p” staging basis because although only one organ/site is microscopically confirmed, that one organ/site is the peritoneum (M1b). 81 82 CASE #1 A patient presents with abdominal pain. A CT scan was performed that showed sigmoid colon wall thickening, no LAD identified and no evidence of distant disease. A colonoscopy was performed where a sigmoid colon mass was BX’d showing adenocarcinoma. Patient then underwent sigmoid colon resection. The path report describes a 4.6 cm adenocarcinoma invading the muscularis propria. There were 17 benign mesenteric lymph nodes examined. 83 Case #1 CSTS = 046 CS EXT = 200 CS TS/EXT EVAL = 3 CSLN = 000 LN EVAL = 3 LNS POSITIVE = 0 LNS EXAMINED = 17 METS AT DX = 00 METS EVAL = 0 84 Case #2 A patient has an abnormal screening colonoscopy showing an obstructing colon cancer. The patient has a CT scan performed which shows evidence of liver and lung METS. The colon cancer appears to invade the abdominal wall. There is probable mesenteric lymph node involvement noted. The patient undergoes a CT guided BX of both the lung nodule and liver mass. Pathology from both shows metastatic carcinoma from colon primary. The patient is referred to Hospice. 85 Case #2 CSTS = 999 CS EXT = 655 CS TS/EXT EVAL = 0 CSLN = 300 LN EVAL = 0 LNS POSITIVE = 98 LNS EXAMINED = 00 METS AT DX = 36 METS EVAL = 3 86 Case #3 A patient presented to ER with severe rectal bleeding and pain. CT scan showed a large mass in the descending colon. The patient was taken to operating room where a laparotomy showed a large mass in the left colon directly invading the spleen. There are mesenteric LNs suspicious for involvement. The liver was palpated and there were 3 small nodules suspicious for implants. One of these nodules was biopsied and sent for frozen, which came back as metastatic signet ring adenocarcinoma consistent with colon primary. After discussion with family, decision to abort operation. 87 Case #3 CSTS = 999 CS EXT = 565 CS TS/EXT EVAL = 1 CSLN = 300 LN EVAL = 0 LNS POSITIVE = 98 LNS EXAMINED = 00 METS AT DX = 26 METS EVAL = 3 88 89 Nicole Catlett, CTR KCR Senior Regional Coordinator Kentucky Cancer Registry nicole@kcr.uky.edu 90 91