Endocrine System Review Two major regulatory systems in the body
advertisement

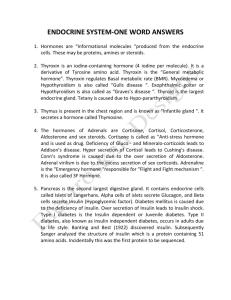
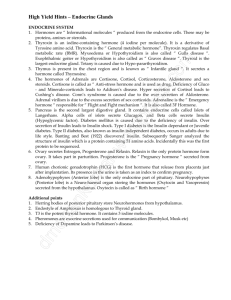
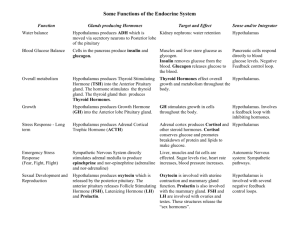
Endocrine System Review Two major regulatory systems in the body: neural and endocrine Endocrine functions: 1. 2. 3. 4. 5. 6. Regulating water-electrolyte balance and organic metabolism Helping body cope with stress Promoting growth/development Controlling reproduction Regulate RBC production Working with autonomic NS to control circulation, digestion and absorption Tropic hormone – primary function is to regulate hormone secretion by another endocrine gland Remember: 1. 2. 3. 4. 5. 6. 7. One endocrine gland may produce many hormones The same hormone may be produced by two different glands One hormone may have various target cells Some hormone release is cyclic in pattern One target cell may be influenced by multiple hormones The same messenger may be a hormone or neurotransmitter depending on source/delivery Some organs/glands may have endocrine and non-endocrine functions General Mechanisms for Hormone Secretion control: 1. 2. 3. Negative-feedback o Output counteracts a change in input Neuroendocrine o Sudden increase in hormone secretion by neural and hormonal control Diurnal (circadian) o Rhythmically fluctuate up and down with time Pituitary Gland Located in the bone cavity at base of brain below hypothalamus, connected to hypothalamus by stalk Anterior lobe – glandular epithelial tissue, secretes peptide hormones Thyroid Stimulating (TSH) Adrenocorticotropic (ACTH) Growth Hormone (GH) Follicle-Stimulating (FSH) Thyroid follicular cells Zona fasciculata/reticularis of adrenal cortex Bone/soft tissue, liver Ovarian follicles Stimulate T3/T4 production (thyroid) Stimulate cortisol secretion (adrenal cortex) Growth, anabolism Follicular growth/development (ovary) Estrogen secretion Seminiferous tubules Sperm production (testes) Luteinizing (LH) Ovarian follicle/corpus luteum Ovulation, corpus luteum development, estrogen and progesterone secretion (ovary) Prolactin Mammary glands Breast development Milk secretion Corticotropin-releasing hormone ACTH, Thyroid-releasing hormone TSH, Gonadotropin-releasing hormone (GnRH) LH/FSH, Growth-releasing/inhibiting hormone GH, Prolactin-releasing/inhibiting hormone PRL Hypothalamic-Hypophyseal portal system – vascular connection between the hypothalamus and anterior pituitary used for pickup/delivery of hypophysiotropic hormones TSH, ACTH, FSH and LH are tropic – regulate secretion of another endocrine gland FSH and LH are collectively called Gonadotropins, TSH called Thyrotropin, GH called Somatotropin Posterior lobe – nervous tissue, forms neuroendocrine system with hypothalamus using neurosecretory neurons, does not produce hormones but releases them when stimulated by the hypothalamus Vasopressin/ADH (Supraoptic) Oxytocin (Paraventricular) Kidney tubules Arterioles Uterus Mammary glands Increase water reabsorption Vasoconstriction Increases contractility Milk ejection Stress Response Stress Hypothalamus Corticotropin-releasing H anterior pituitary ACTH adrenal cortex cortisol Growth Hormone (GH) 1. 2. 3. 4. 5. Simulates liver to make somatomedins, primary is insulin-like growth factor (IGF-1) o Acts directly on bone/soft tissue o Stimulates protein synthesis, cell division, lengthening/strengthening of bones Metabolic effects o Increases triglyceride breakdown o Decreases glucose uptake by muscles GH hyposecretion o Pituitary or hypothalamic defect o Can cause dwarfism in children and little effect in adults GH hypersecretion o Tumor of anterior pituitary o Can cause gigantism before epiphyseal plates close o Acromegaly or thickening of bones in extremities/face Other hormones are essential for growth o Thyroid hormone – hyposecretion causes stunted growth in children o Insulin – decreased/excessive growth o Androgens – pubertal growth spurt, protein synthesis o Estrogens Pineal Gland 1. 2. 3. 4. Secretes the hormone melatonin – keep body’s circadian rhythms in synchrony, increased secretion during the night (light-dark cues) Suprachiasmatic nucleus (SCN) serves as pacemaker for rhythms Jet lag – not maintaining the internal clock with external environment Photoreceptors in the eye transmit signals to SCN to maintain this clock Thyroid Gland Located on the trachea below the larynx consisting of two lobes joined by narrow tissue, largest endocrine gland, involved in production, storage and release of thyroid hormone Follicular cells: 1. 2. 3. Surround a hollow sphere of colloid to form function unit - follicle o Extracellular storage site for TH Produce iodine-containing hormones derived from tyrosine o T4/thyroxine/tetraiodothyronine o T3/triiodothyronine C-cell secrete calcitonin TH Synthesis 1. 2. 3. 4. Requires tyrosine (made by body) and iodine (diet) Thyroglobulin (contains tyrosine) is excreted by follicular cells into colloid Thyroid gland transfers iodine in colloid via iodine-pump Tyrosine and iodine bind and T3/T4 formed TH Storage – remain in colloid until secretion, supply is enough to last body several months TH Secretion – follicular cells thyroglobulin colloid freeing T3 and T4 (lipophilic) to diffuse across plasma membrane, T3>T4 Thyroid Gland Follicular Cells T3/T4 Most cells Thyroid Gland C Cells Calcitonin Bone Increased metabolic rate Improves cardiac and muscle contractility Increases target cell response to catecholamines Increases GH secretion Required for proper neural growth Increases bowel motility Decreases LDL (bad) cholesterol Decreases plasma [Ca2+] Hypothyroidism Causes – failure of the thyroid, deficiency of TRH, TSH or both, too little dietary iodine intake Symptoms - overall reduction in metabolic activity, sensitive to cold, weight gain, easily fatigued, weak pulse, slow reflexes, slow speech, poor memory Myxedema – water-retaining carbohydrate molecules enter skin resulting in puffy appearance on face/extremities Cretinism – from birth, dwarfism, mental retardation Treatment – replacement therapy, add iodine to diet Hyperthyroidism Causes - Grave’s disease – most common cause, autoimmune disease that targets TSH receptors on thyroid gland acting like TSH but lacking the negative feedback regulation Goiter – can occur with hypo/hyperthyroidism when thyroid gland is stimulated Symptoms – high metabolic rate, sensitive to heat/sweating, low body weight, weakness, high cardiac output, irritability, anxiousness, exophthalmos – water-retaining carbohydrates deposited behind the eye (bulging) Treatment – surgical removal of portion of thyroid gland, give radioactive iodine which destroys thyroid tissue, antithyroid drugs that interfere with TH synthesis Parathyroid Gland Four tiny glands located on the back surface of the thyroid gland Parathyroid hormone (PTH) Bones, kidneys, intestines Increase plasma [Ca2+] Decrease plasma [PO43-] Stimulate Vitamin D activation Remember – Calcium allows for excitation-contraction coupling in muscles, without it, death would ensue from asphyxiation cause by hypocalcemic spasm of respiratory muscle Also, plasma [Ca2+] affects stimulus-secretion coupling, maintaining tight junctions between cells, blood clotting Which hormones regulate plasma [Ca2+]? 1. 2. 3. PTH Calcitonin Vitamin D Bone density peaks at age 30 and declines after that. When bone resorption (removal) exceeds bone formation, the result is disease such as osteoporosis – reduced bone density, bones lose minerals such as calcium (99% of this mineral is in the bones) leading to breakage, fragility and weakness Bone cells: 1. 2. 3. Osteoblast – secrete extracellular organic matrix (make bone) Osteoclast – resorb bone in vicinity by releasing acid to break down matrix (break bone) Osteocyte – retired osteoblasts that make up main structure of bone Hypercalcemia PTH hypersecretion, [PO34-] reduced, reduced nerve/muscle excitability, bone thinning, kidney stones Calcitonin – produced by C cells, secreted when plasma [Ca2+] is high and acts to lower it, inhibits osteoclast activity Hypocalcemia PTH hyposecretion, [PO34-] increased, increased nerve/muscle excitability, irritability, paranoia Vitamin D Deficiency Impaired intestinal absorption of calcium because Vitamin D (must be activated by kidney and liver, also made by sunlight) is essential for this process, PTH maintains plasma [Ca2+] level at the expense of bone health, known as rickets in children and osteomalacia in adults Adrenals Located above the kidneys in a capsule of fat, external to the peritoneal sac, outer layer is adrenal cortex (steroidal hormones) and inner layer is adrenal medulla (catecholamines) – both are separate endocrine organs Adrenal Cortex Zona glomerulosa (O) Zona fasciculate (M/biggest) Zona reticularis (I) Aldosterone (Mineralocorticoid) Cortisol (Glucocorticoid) Kidney tubules Androgens (Like sex hormones) Bone/brain (females only) Most cells Increase Na+ reabsorption Increase K+ secretion Increase blood glucose at the expense of storage Stress response Pubertal growth spurt Sex drive Aldosterone 1. 2. 3. Acts on distal and collecting tubules of kidney Secretion increased by o Activation of rennin-angiotension-aldosterone system reduce [Na+] and BP o Direct stimulation on cortex by increasing plasma [K+] Independent of anterior pituitary control Cortisol 1. 2. 3. 4. 5. 6. 7. Stimulates gluconeogenesis in liver Inhibits glucose uptake (not in brain) Stimulates protein degradation and lipolysis Stress response Can have anti-inflammatory/immunosuppressive effects (should not use long term) Displays diurnal rhythm Involved in negative feedback loop involving CRH (hypothalamus) and ACTH (pituitary) Androgens 1. 2. 3. Dehydroepiandrosterone (DHEA) is the only adrenal sex hormone with biological importance Overpowered by testosterone in males Facilitates growth of pubic hair, growth spurt and sex drive in women Disorders Aldosterone hypersecretion – adrenal tumor (Conn’s Syndrome) or high activity of rennin-angiotensin system Symptoms – high Na+ retention/K+ depletion, high BP Cortisol hyposecretion – Cushing’s Syndrome, causes include excessive CRH and ACTH, cortisol-releasing or ACTH-releasing adrenal tumor, Symptoms – hyperglycemia, glucosuria (adrenal diabetes), abnormal fat distribution Androgen hypersecretion – 1. 2. 3. 4. Adult female – hirsutism: deep voice, muscular arms/legs, small breast, menstruation ceases Newborn female – male external genitalia Pre-pubertal male – pseudopuberty Adult male – no effect Adrenocorticol insufficiency – 1. 2. Addison’s Disease (primary) Autoimmune disease (primary) o Aldosterone deficiency 3. o Cortisol deficiency Secondary o Hypothalamic/pituitary deficiency Adrenal Medulla Epinephrine/Norepinephrine (catecholamines) Sympathetic receptor sight throughout body Reinforces sympathetic response Helps with stress response Blood pressure regulation Medulla is – 1. 2. 3. Modified part of sympathetic nervous system (postganglionic) When stressed, site of primary adrenomedullary secretion Epinephrine/norepinephrine secreted into blood by exocytosis (chromaffin granules) o Fight or flight response o Maintain arterial BP o Increase blood glucose and fatty acids General Stress Response SNS stimulation Epinephrine secretion CRH-ACTH-cortisol system activated (mobilize metabolic resources) elevated blood glucose/fatty acid decrease insulin/increase glucagon maintain blood volume/pressure rennin-angiotensin system activated vasopressin secretion increased Interconversion Among Organic Molecules Glucose Fatty acids Amino acids (protein) Liver/muscle Adipose tissue Muscle Glycogen Triglyceride Body protein Primary energy source Primary reservoir Source during fasting Major tissues 1. 2. 3. 4. Liver – maintain normal blood glucose levels, site of interconversions Adipose tissue – energy storage Muscle – primary amino acid storage, major energy user Brain – can only use glucose but does not store glycogen Pancreas Is an exocrine (secretes solution into digestive tract through duct) and endocrine organ Islet of Langerhans 1. 2. 3. Cluster of endocrine cells between exocrine cells Has various cell types o Beta (B) cells – most abundant, synthesize/secrete insulin o Alpha (a) cells – synthesize/secrete glucagon o Delta (D) cells – synthesize/secrete somatostatin o F cells (PP cells) – secrete pancreatic polypeptide (may deal with appetite control), least common Insulin and glucagon regulate fuel metabolism Somatostatin – released when blood sugar/amino acids are high during absorption, decrease secretion of insulin, glucagon, and itself, more research needed Insulin – anabolic, promotes uptake of glucose, fatty acids and amino acids turning them into stores, secreted during absorptive state when blood glucose is high Glucagon – mobilizes energy-rich molecules during postabsorptive state when blood glucose is low, opposes action of insulin, no known clinical abnormalities with this hormone Disorders Diabetes Melllitus – elevated blood glucose level, “sweet” urine 1. 2. Type I – lack of insulin secretion, childhood, 10-20%, autoimmune destruction of B cells, treatment includes insulin injections, diet management, exercise Type II – normal/increased insulin secretion but reduced sensitivity of target cells, adulthood, 80-90%, treatment includes diet and weight control, exercise, sometimes oral hypoglycemic drugs Hormonal Control of Fuel Metabolism Hormone Insulin Blood glucose Glucose uptake Make glycogen Glucagon Break glycogen Make glucose Break glycogen Make glucose Secrete glucagon Make glucose Decrease glucose uptake by tissues Decrease glucose uptake by muscle Epinephrine Cortisol Growth Hormone Metabolic Effect Blood Fatty Acid Make triglyceride Blood Amino Acid AA uptake Muscle protein Make protein Secretion Stimuli Inc blood glucose/AA Break triglyceride - - Break triglyceride - - Break triglyceride Break protein Break protein Dec blood glucose, Inc AA Sympathetic during stress and exercise Stress Break triglyceride AA uptake Make protein, DNA and RNA Deep sleep, stress, exercise, low blood sugar Metabolic acidosis 1. 2. 3. 4. Severe diarrhea Diabetes mellitus – excess fat metabolism because glucose cannot be utilized resulting in keto acids Strenuous excersize – anaerobic glycolysis lactic acid Uremic acidosis Sex Hormones Undifferentiated reproductive system contains – 1. 2. 3. Mullerian ducts – make female reproductive tract Wolffian ducts – make male reproductive tract The other duct degenerates resulting in a specific sex Male Repro Spermatogenesis requires: 1. 2. Leydig cells – produce testosterone stimulated by LH Sertoli cells – produce androgen-binding protein (ABP) stimulated by FSH Role in Metabolism Regulator in postabs/absorptive cycle Same as insulin Energy for emergency/exercise Move fuels in adapting to stress Growth 3. 4. Remember – GnRH stimulates release of FSH and LH Parts of sperm: acrosome covers head (nucleus), centricle connects head to midpiece (contains mitochondria), tail is microtubules Female Repro Ovarian cycle alternates between two phases (1) follicular – presence of maturing follicle (2) – presence of corpus luteum, interrupted if pregnancy occurs and lasts ~ 28 days Follicle – secretes estrogen during first ½ of cycle Corpus luteum – secretes progesterone and estrogen during second ½ Estrogen – LH/FSH convert androgens to estrogen 1. 2. 3. 4. 5. 6. Low concentrations – negative feedback inhibition of LH/FSH during follicular phase High concentrations – anterior pituitary secretes more LH/FSH resulting in LH surge and ovulation Essential for egg maturation/release Stimulates granulosa cell proliferation follicle maturation Thins cervical mucous so sperm can penetrate Triggers onset of parturition Progesterone – negative feedback inhibition of LH/FSH preventing surge during luteal phase/pregnancy 1. 2. 3. 4. Make uterus a good environment for embryo Forms thick mucus plug at cervix Inhibits GnRH and Gonadotropin Stimulates alveolar development but inhibits prolactin/uterine contraction during gestation Inhibin – acts on the pituitary to inhibit secretion of FSH Lactation Prolactin – anterior pituitary hormones that stimulates breast development and milk production in females Oxytocin – hypothalamic hormone stored in the posterior pituitary stimulating uterine contraction and milk ejection Suckling stimulate mechanoreceptors hypothalamus posterior pituitary releases Oxytocin myoepithelial cells surrounding alveoli contract milk ejection Sucking stimulate mechanoreceptors hypothalamus increase Prolactin releasing hormone anterior pituitary releases Prolactin increases milk secretion