Adrenal_Gland_
advertisement

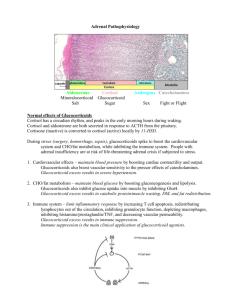
There are two adrenal glands, one located above each kidney. Each gland consists of two morphologically and functionally distinct endocrine tissues – the outer cortex and the inner medulla The Adrenal Gland The cortex, which is derived from mesodermal tissue, is composed of three zones 1. The outermost zone, the Zona glomerulosa, synthesizes the mineralocorticoid aldosterone 2. The middle zone, the Zona fasciculata, and the innermost zone, 3. The Zona reticularis, synthesize the glucocorticoid cortisol and the androgens dehydroepiandrosterone (DHEA) and androstenedione The medulla, which is derived from the neural crest, can be considered a modified sympathetic ganglion that directly releases catecholamines into the circulation The reticularis is the one big in androgen production. Zones 1 & 2 & 3 all the hormones produced are steroids. The basic backbone of cholesterol synthesis comes from diet or the liver. They are cholesterol based. The conversion of the cholesterol to its end product. Making the enzyme relies on Transcription and translation. The androgens that are produced are DHEA and androstenedione can be converted to testosterone, but they are not the main sources of testosterone in the body. Diet, liver Adrenal Steroidogenesis C3, 11, 17, 18, 21 are conversion sites C11 C3 C21 Progesterones: 21 carbons Androgens: 19 carbons (Estrogens: 18 carbons) C17 C18 The steroidogeneis pathway is messy! 1. The conversion of cholesterol in the diet in the liver is canned out by enzymes which is a rate limiitng step. The pregnenolone – convereted to andorogens. Most of the genetic problems associated with 21 – hydroxylase and the 11 B hydrolase. The zones are unique because of the complement of enzymes. The blue arrows are to remind you that things are occuring at different levels in the cells. The CYP21 hydroxylase you will see referred to as 21-alpha. CYP11A1 - Side Chain Cleavage CYP17 - 17-hydroxylase *CYP21 - 21-hydroxylase (defect accounts for 95% of genetic abnormalities) *CYP11B1 - 11-hydroxylase(next most common defect) CYP11B2 - Aldosterone Synthase Page 1 Becky Stepan Rose-Hellekant – Adrenal Gland Pregnenolone Synthesis Rate limiting step; ACTH regulated! (21 - carbons) Aldosterone Synthesis in Z. glomerulosa only! C3 C21 C11 C18 Cortisol is produced at the highest level in the human body. If the 11 B defect is in place, you will not have cortisol, corticosteroids, and androgens. Glucocorticoids have Zona glomerulosa cells: -lack 17-hydroxylase but -express Aldosterone Synthase 0.125 mg aldosterone secreted/d Plasma concentration = 0.01 g/dL Cortisol Synthesis in Z. fasciulata and z. reticularis Cortisol is the negative feedback to the pituitary and the anterior pituitary – 11-Deoxgycortisol has a higher mineralcorticoid properties and actions. – too much of this will increase BP because of volume expansion. 10 mg/day secreted Plasma concentration: 8 AM - 16 g/dL 4 PM - 4 g/dL Page 2 Becky Stepan Rose-Hellekant – Adrenal Gland 21-Hydroxylase Deficiency ↓Cortisol and Aldosterone ↑ACTH ↑Androgens Symptoms: Virilization, Hypotension (due to reduced blood volume) * With excess production – you can end up with a lot of testosterone. You are reducing aldosterone, and you are reducing the mineralcorticoid effects. 11-hydoxylase Deficiency ↓Cortisol and Aldosterone ↑ACTH ↑Androgens Virilization, Hypertension (due to excess 11-deoxycortisol which has mineralo-corticoid activity) Mineralocorticoid System: Aldosterone is responsible for sodium absorption across epithelia A. Aldosterone Synthesis 1. Synthesized by glomerulosa cells of adrenal cortex 2. Glomerulosa cells lack 17a -hydroxylase (CYP17) and uniquely express aldosterone synthase (CYP11B2) B. Control of Aldosterone Synthesis 1. Regulated by the renin-angiotensin system and increased plasma potassium 2. Under tonic control of ACTH 3. Minimal binding to plasma proteins so metabolized and excreted quickly C. Mineralocorticoid Receptor 1. Aldosterone binds to an intracellular receptor, mineralocorticoid receptor (MR), expressed, primarily, in the kidney (distal tubule and collecting duct), distal colon, salivary glands, sweat glands, and hippocampus 2. MR is a member of the steroid-hormone receptor superfamily and is a ligand-activated transcription factor that regulates gene expression. 3. MR shares significant homology with GR. Cortisol binds with equal affinity to MR as aldosterone. D. Effects of Aldosterone 1. Aldosterone stimulates sodium reabsorption and potassium and H+ excretion in target organs such as the kidney, colon, and salivary glands. Mineralocorticoids Mineralcorticoids Aldosterone Effects: • Causes retention of Na+ and excretion of K+ and results in ECF and blood volume expansion. Increasing reabsorption of Na+ from urine, sweat, saliva and colon. Increases in sodium in kidneys results in increase exchange for K+ and H+ in renal tubules producing K+ diuresis and increased urine acidity and alkalosis. Renin suppression is a result A decrease in plasma volume promotes angiotensin II conversioncauses vasoconstriction in adrenals causes aldosterone production. • Regulated by Renin-Angiotensin, K+, ACTH Induced by sodium depletion or blood volume decrease Page 3 Becky Stepan Rose-Hellekant – Adrenal Gland Hypothalamic-Pituitary-Adrenal Axis ACTh is stimulatory – the primary hormone responsible for the negative feedback will be cortisol. Physical and psychological STRESS + Low dose dexamethasone test HYPOTHALAMUS + CRF + ANTERIOR PITUITARY - ACTH ADRENAL CORTEX CYTOKINES IL-1 IL-6 TNF- Corticotropin Releasing Hormone • 41 AA polypeptide • Synthesized in hypothalamus • Proinflammatory cytokines augment release of CRF Inflammation - CORTISOL CRF/H: corticotropin releasing factor/hormone ACTH: adrenocorticotropic hormone Adreno Cortico Tropic Hormone • Synthesized in the A. pituitary as part of a larger 241 aa precursor, propriomelanocortin. • ACTH binds to Melanocortin-2-receptor (a Gαs coupled protein so elevation of cAMP initiates signal transduction cascade) • 39 AA polypeptide • Rapidly stimulates side-chain cleavage enzyme (CYP11A). THIS IS A RATE-LIMITING STEP. Therefore ACTH promotes conversion of cholesterol to pregnenolone. • Has little effect on aldosterone by glomerulosa cells except at high levels. The glucocorticoids, 11 deoxycortocosterone and cortisol have weak mineralocorticoid activity (compared to aldosterone). • Ectopic production possible in cancer and is not responsive to neg feedback by cortisol. • These hormones can easily traverse across cell membranes. Higher in the non-golmerulus. Those hormones can easily get to the glomerulosa. Glucocorticoids • Cortisol is the principal glucocorticoid secreted − 10% circulates free − 90% circulates bound • 60% to CBG (corticotropin binding globulin=transcortin) • 30% to albumin − T 1/2= 70-90 min − Cortisol, cirrhosis, nephrosis, hyperthyroidism ↓CBG • Estrogens, pregnancy and hypothyroidism ↑CBG Page 4 Becky Stepan Rose-Hellekant – Adrenal Gland Glucocorticoid Metabolism • Cortisol is quickly converted to cortisone. Cortisone can be easily converted to cortisol. • But most of metabolism occurs in the liver where cortisone is rapidly conjugated to form tetrahydrocortisone glucuronide or sulfated. These derivatives are soluble in serum and are excreted by kidneys. • These 17-hydroxycorticosteroid metabolites are used to assess adrenal steroid production in 24h urine collections • Other conversion enzymes found in kidney, colon and salivary glands. Glucocorticoid Receptor • GR - Intracellular Steroid Hormone Receptor • Transcription factor regulating gene expression • Found in virtually all cells where it regulates a variety of processes including development, metabolism and immune response. • Two isoforms - GR and GR − GR mediates physiological effects − GR dominant negative regulator • They are promiscusis and may dimerize with an alpha-lapha or a beta-beta. The binding and storage of these hormones in the cytoplasms are done by heat-shock proteins; these are drug target productions in development. HSP = important for the oncology field. Glucocorticoid promotes mobilization of serum energy substrates Glucocorticoids: Actions at Excess Levels Page 5 Becky Stepan Rose-Hellekant – Adrenal Gland Hyperadrenocorticism/hyperadrenalism/Cushing Syndrome If due to excess ACTH secretion, blood profiles are: ↑ACTH ↑Cortisol If due to excess Cortisol production blood profiles are: ↑ Cortisol ↓ ACTH Most common cause is iatrogenic w/long term glucocorticoid use. Hypoadrenalism 1o -Addison’s Disease (usually due to immune mediated destruction of adrenal cortex) ↓Cortisol ↓Aldosterone ↑ACTH o 2 - Iatragenic by sudden withdrawal of exogenous glucocorticoid ↓Cortisol ↓ACTH Hyperpigmentation may be seen in primary adrenal insufficiency due to ACTH overproduction by the pituitary. The ACTH molecule contains the sequence for alphamelanocyte-stimulating hormone (MSH), which stimulates melanocytes. (See CRH slide). Page 6 Becky Stepan Rose-Hellekant – Adrenal Gland Here is an example of endocrine imbalance which occurs with the administration of exogenous hormone, in this case cortisol. High levels of circulating cortisol reduces the levels of hypothalamic releasing hormone (corticotrophic releasing hormone) and anterior pituitary hormone (adrenocorticotrophic hormone) due to long loop negative feedback. Cortisol is typically produced by the adrenal cortex. Target cells/tissues respond to cortisol (whether it is endogenous or exogenously provided). Usually excess cortisol is provided exogenously due to need to reduce immune reaction Once the reaction subsides, exogenous cortisol is withdrawn. Slow withdrawal from exogenous cortisol is necessary to allow a smooth transition back to endogenous regulation of cortisol. Too rapid of exogenous cortisol withdrawal would lead to cortisol crash because the hypothalamopituitary-adrenal axis is temporarily shut down. The adrenal glands are incapable of producing cortisol without a transition period to normal production levels. FYI: Look to specific lecture on adrenal gland physiology. * Too little glucocorticoid causes symptoms of adrenal insufficiency, such as anorexia, nausea, vomiting, abdominal pain, asthenia, poor weight gain, and weight loss. * Too much glucocorticoid causes excessive weight gain, cushingoid features, hypertension, hyperglycemia, cataracts, and growth failure. * In children, growth failure is a sensitive indicator of exposure to excessive glucocorticoids. If the endocrine imbalance, in this case hypersecretion, is due to problems at the level of the peripheral endocrine gland, then it is called “primary hypersecretion” If the problem is at the level of the hypothalamus it is known as secondary. Some references suggest that problems at the level of the pituitary is referred to as “tertiary” but others lump this into “secondary hypersecretion” along with the hypothalamus. One can distinguish the problem endocrine gland by measuring hormone levels in the peripheral blood. Expected circulating levels of hormone: Page 7 Becky Stepan Rose-Hellekant – Adrenal Gland Secondary Hyposecretion Primary Hyposecretion What relative levels of CRH, ACTH and cortisol would you expect in each of these scenarios? Circadian and Pulsatile Rhythm Cortisol concentration follows a circadian rhythm, peaking in the early morning and reaching a nadir in the evening. Superimposed on this rhythm is the pulsatile secretion of ACTH. The circadian rhythm reflects, in part, the influence of the hypothalamic pacemaker, suprachiasmatic nucleus, on CRF secretion. When blood is drawn is important to interpretation of results? Key Concepts • Glucocorticoid production and release are under ACTH regulation. Glucocorticoid supports homeostasis of blood glucose regulation; growth; thyroid system, reproduction • Mineralocortiocid (aldosterone) is under antiotensen II and K+ regulation, as well as tonic ACTH. High levels in ACTH will cause high levels of aldosterone production. • Aldosterone regulates body sodium balance. • Two genetic anomalies of adrenal cortex: 11b hydroxylase defect: low cortisol and corticosterone levels and mineralocorticoids. Hypertension due to 11 deoxycortisol which has mineralocortioid effects even though aldosterone is low. 21 - hydroxylase defect: low glucocortiocids and low mineralocorticoids: Hypotension due to low mineralocorticoid production as well as low 11-deoxycortisolproduction. Hyperpigmentation due to excess MSH co-production with ACTH ACTH is produced as a preprohormone, pro-opiomelanocortin. Page 8 Becky Stepan Rose-Hellekant – Adrenal Gland