Anatomy of the Urinary System
advertisement

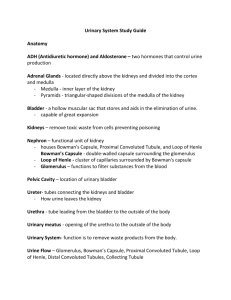
Anatomy of the Urinary System Structures • Kidneys: • located under back muscles, behind parietal peritoneum, above the waistline, right slightly lower than left • Internal structure: • Cortex: outer layer • Medulla: inner portion • Pyramids: triangular sections of medulla • Kidney…con’t • Papilla: narrow innermost end of pyramid • Pelvis: expansion of upper end of ureter, inside the kidney • Calyces: division of the renal pelvis Microscopic Structures • • • • Nephron: functional unit of kidney 1. Renal Corpuscle: Bowman’s capsule with glomerulus Glomerulus: network of blood capilliaries • 2. Renal Tubule: • Proximal convoluted tubule: first segment • Loop of Henle: extension of prox. Tubule; consists of descending limb, loop and ascending limb Renal Tubule…con’t • Distal convoluted tubule: extension of ascending Loop of Henle • Collecting Tubule: straight extension of distal tubule Ureters • Long narrow tube with expanded ends in the kidney (renal pelvis) • Lined with mucous membrane • Drains urine from kidney to urinary bladder Urinary Bladder • Elastic muscular organ, capable of great expansion • Lined with mucous membrane arranged with rugae • Stores urine before voiding • Voiding Urethra • Narrow tube from urinary bladder to exterior urinary meatus • Lined with mucous membrane • Passage for urine from bladder to meatus • Passage of semen from the body Functions • 1. Producing and Excreting Urine • 2. Regulates chemicals in the blood – Electrolytes, acid base balance • 3. maintains fluid balance • 4. Regulate blood pressure through secretion of renin Formation of urine • 3 processes: • 1. Filtration: continually in renal corpuscle, • glomerular blood pressure causes water and dissolved substance to filter out of glomeruli into bowman’s capsule, • normal rate is 125 ml/min • 2. Reabsorption: movement of substances out of renal tubules into blood in the peritubular capillaries; • Water, nutrients, and ions are reabsorbed • Water is reabsorbed by osmosis from proximal tubules • 3. Secretion: movement of substances into urine in the distal and collecting tubules • Hydrogen ions, potassium ions, and certain drugs are secreted by active transport • Ammonia is secreted by diffusion Control of Urine Volume • Posterior Pituitary hormone: ADH, which decreases urine, by making collecting tubules permeable to water • If no ADH is present, collecting tubules are practically impermeable to water • Adrenal Cortex: aldosterone, important in controlling reabsorbtion of sodium Abnormal amounts of Urine • Anuria: absence of urine • Oliguria: scant amounts of urine • Polyuria: excessive amounts of urine Micturation • Urination/Voiding • Sphincter control: • Internal urethral sphincter: involuntary, located at the bladder exit • External urethral sphincter: voluntary, located just below the neck of the bladder • Most learn voluntary control between 2 and 3 years of age Emptying Reflex • • • • Initiated by stretch reflex in bladder wall Bladder wall contracts Internal sphincter relaxes External sphincter relaxes and bladder is emptied Disorders • Urinary Retention: urine produced, bladder wont empty • Urinary Suppression: no urine produced, but bladder will empty • Incontinence: Voiding involuntarily – Causes: spinal injury, stroke – Retention may cause cystitis Disorders con’t • Obstructive Disorders • Renal Calculi (kidney stones) block ureters, intense pain, renal colic • Neurogenic bladder: paralysis or abn functioning of bladder, prevents normal flow of urine out of the body • Tumors: renal cell carcinoma & Bladder cancer: Characterized by blood in urine UTI’s • Often caused by gram negative bacteria • Escherichia coli (E. coli) causes about 80% of UTIs in adults. These bacteria are normally present in the colon and may enter the urethral opening from the skin around the anus and genitals. Women may be more susceptible to UTI because their urethral opening is near the source of bacteria (e.g., anus, vagina) and their urethra is shorter, providing bacteria easier access to the bladder. UTI’s con’t • Other bacteria that cause urinary tract infections include Staphylococcus saprophyticus (5 to 15% of cases), Chlamydia trachomatis, and Mycoplasma hominis. • Men and women infected with chlamydia trachomatis or mycoplasma hominis can transmit the bacteria to their partner during sexual intercourse, causing UTI • Uretritis: inflammation of the urethra • Cystitis: inflammation or infection of the bladder • Pyelonephritis: inflammation of the renal pelvis and connective tissues of the kidney: acute(infectious) or chronic (autoimmune) Glomerular disorders • Nephrotic syndrome: • Proteinuria: protiens in urine • Hypoalbuminemia: low plasma protiens (albumin) levels • Edema: tissue swelling caused by loss of water from plasma as a result of hypoalbuminemia • Acute glomerulonephritis: caused by delayed immune response to streptococcal infection Chronic Glomerulonephritis • Slow inflammatory condition caused by immune mechanisms and often leads to renal failure. Renal Failure • Acute: abrupt reduction in kidney function that is usually reversible • Chronic: slow progressive loss of nephrons, caused by a variety of underlying diseases (BUN increases, GFR decreases, creatinine increases Chronic Renal Failure • Stage 1: some nephrons lost • Compensation by enlargement of remaining • BUN is kept normal • GFR drops (up to 75%) • Often asymptomatic, may last for years Stage 2 • Renal insufficiency: Kidney no longer compensates for loss of nephrons • Remaining cant handle urea load • BUN increases dramatically • Kidneys ability to concentrate urine is impaired: polyuria and dehydration occur Stage 3 • • • • • Called “uremia” or “uremic syndrome” High blood urea BUN very high Caused by loss of kidney function GFR low=oliguria: edema and hypertension result • Dialysis or kidney transplant required or • Death occurs