The Motor System and Its Disorders
advertisement

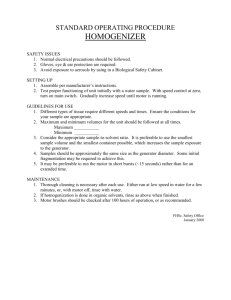
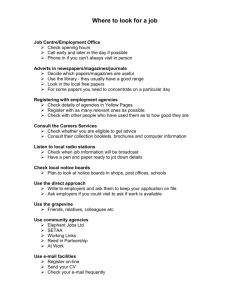
The Motor System and Its Disorders Lecture 3 Lecture Outline: Overview and major pathways Cerebellum Cerebellar atrophy videos Basal Ganglia Hyperkinetic disorders Hypokinetic disorder Huntington’s chorea Tourette’s Tardive Dyskinesia Parkinson’s Disease - videos Cortex Primary motor Premotor, supplementary motor, prefrontal Parietal cortex Apraxia(s) Motor Control Behaviour is observable motor output by the organism Sitting, writing, speaking, eating, typing, running, playing, having sex etc. These different behaviours are executed by different aspects of the motor system Some motor functions are automatic (e.g., breathing, eating, sex), while others require a lot of practice and effort (e.g., playing a piano) Steps in Motor Action Muscles 4 Major Motor Pathways 1. 2. Corticospinal (cortex to spinal cord) a) Lateral – distal limb muscles (fine manipulations) b) Ventral – trunk and upper leg muscles (posture/locomotion) Corticobulbar (cortex to pons, 5th, 7th, 10th and 12th cranial nerves) – control of face and tongue muscles; upper face both contralateral, lower face contralateral Major Motor Pathways 3. 4. Ventromedial (brain stem to spinal cord) – trunk and proximal limb muscles (posture, sneezing, breathing, muscle tone) Rubrospinal (red nucleus to spinal cord) – modulation of motor movement (limb movement independent of trunk movement) Cerebellum Vermis Intermediate zone Lateral zone Within are deep cerebellar nuclei: Fastigial nucleus Interpositus nucleus Dentate nucleus Vermis Kinesthetic and somatosensory inputs from the spinal cord projections to fastigial nucleus Damage interrupts posture and walking In monkeys, unilateral lesions of the fastigial nucleus cause the monkeys to fall (ipsilateral side) Intermediate Zone Inputs from red nucleus (brain stem & motor cortex) and somatosensory info from the spinal cord Projects to interpositus nucleus red nucleus (loop) Damage produces rigidity and difficulty in moving limbs Action tremor or intention tremor – a tremor causing movement to occur in a staggered manner during motor act. Lateral Zone Inputs from motor and association cortices (through pons) Projections to dentate nucleus primary motor and premotor cortex 1. Balistic movement – movement that occurs so quickly that it can not be modified by feedback E.g., swinging of a batter trying to hit a ball moving 140 km/h Lateral Zone 2. Multijoint movements 3. Learning of new movements 4. Timing of motor movements (and cognitive functions) Basal Ganglia Unlike the cerebellum, which plays a role in rapid balistic movements, the basal ganglia are more important for the accomplishment of movements that may take some time to initiate or stop Important for internal guiding (rather then external) of movement Dopamine – nigrostriatal pathway Basal Ganglia Damage to the basal ganglia: Produces either too much activation (hyperkinetic) responses= twitches, movements bursts, jarring, etc. Huntington’s Chorea-dominant gene based, increases glutamate in striatum which destroys GABA neurons in BG and loss of inhibition No cure Tourette’s OR Produces too little force (hypokinetic)=rigidity Parkinson’s disease Pink=inhibition Blue=excitation Hyperkinetic Disorder Huntington’s Chorea Genetic disorder associated with intellectual deterioration and abnormal movements The symptoms appear from 30 to 50 years of age Initially the person shows small involuntary movements that look like fidgeting These symptoms increase until they are incessant usually involve whole limbs Eventually the movements become uncontrollable and affect the head, face, trunk and limbs Pink=inhibition Blue=excitation Hyperkinetic Disorder Tourette’s Syndrome 1. 2. 3. Three stages: Only multiple tics (twitches of the face, limbs or the whole body) Inarticulate cries are added to multiple tics Emission of articulate words with echolalia – repeating what others have said or done – and coprolalia – uttering of obscene words – are added in this stage Onset is typically 2-15 years of age Drugs that block dopamine (e.g., haloperidol) ameliorate the disorder Hyperkinetic Disorder Tardive Dyskinesia Occurs in 20-40% of individuals who are long time (at least 3 months) users of conventional antipsychotics Conventional or classic antipsychotics (e.g., haloperidol) block dopamine receptors Symptoms include: Chorea Tics Akathisia – compulsive, hyperactive, and fidgeting movements of the legs Dystonia – painful, sustained muscle spasms of the same muscle groups frequently causing twisting and repetitive movements and abnormal postures Possible causes are supersensitivity of dopamine neurons after prolonged suppression Atypical antipsychotics are good at suppressing psychoses and they have fewer motor side effects Hypokinetic Disorder Parkinson’s Disease 0.1-1.0% of the population Incidence rises in older population Degeneration of neurons in substantia nigra and to the loss of the neurotransmitter dopamine Symptoms: 1. 2. Positive – abnormal behaviours not seen in intact individuals Negative – absence of normal behaviours Hypokinetic Disorder Parkinson’s Disease POSITIVE SYMTOMS 1. 2. 3. Tremors at rest Muscular rigidity – simultaneously increasing the muscle tone in both extensor and flexor muscles. Involuntary movements – akatheisia –motor restlessness, ranging from a feeling of inner disquiet to an inability to sit or lie quietly NEGATIVE SYMTOMS 1. 2. 3. 4. 5. 6. Abnormal posture Abnormal righting – difficulties in achieving a standing position Abnormal locomotion – difficulty initiating stepping Festination – tendency to engage in behavior at faster and faster speeds. Aprosodia – Lack of emotional tone in speech and comprehension of emotional tone Akinesia – absence of movement (e.g., blank facial expressions, lack of blinking) Bradykinesia – slowness of movement Hypokinetic Disorder Parkinson’s Disease - Causes 1. 2. 3. Idiopathic – cause not known Postencephalitic – “sleepy sickness” – 1916-1917 vanished by 1927 see Oliver Sack in Awakenings Drug induced (e.g., major tranquilizers, MPTP – contaminant in heroin – is toxic to dopamine neurons) Treatments: L-dopa dopamine precursor video Cortex Externally guided movements – those requiring sensory inputs Picking up objects, using tools, moving eyes to explore faces, making gestures etc. Primary Motor Cortex Primary motor cortex executes motor movements When the primary motor cortex is damaged the result is weakness and imprecise fine motor movements Premotor and Supplementary Motor Areas (SMA) Premotor and SMA are involved in a plan of action - motor programs – an abstract representation of an intended move We have the ability to prepare for the next movement before it occurs (we have an internal program) Premotor and Supplementary Motor Areas (SMA) Premotor cortex – Two-hand Coordination THE MONKEY HAS LEARNED THE TASK PUSH THE OBJECT THROUGH THE HOLE AND CATCH IT WITH THE OTHER HAND; With damage to premotor cortex, cannot coordinate two hands to do the task Anterior Cingulate Cortex Cingulate is involved in many functions Subject of controversy as it is rarely damaged in isolation fMRI data shows that it is activated in variety of tasks Cingulate has been implicated in motor planning of movements especially when they are novel or require much cognitive control “A” “B” (well rehearsed) “A” “M” (novel) anterior cingulate activation Topography for different motor functions Manual – posterior regions Speech – middle regions Ocular – anterior regions Frontal Eye Fields Control of voluntary eye movements (scanning the visual field to see a friend…or someone you like) Reflexive eye movements are controlled by brain stem nuclei (superior colliculi) Frontal eye fields can inhibit the activity of superior colliculi Prefrontal Cortex Cortex that receives projections from the dorsomedial thalamus Last to develop in terms of evolution and ontogenetically Involved in highest level of motor functions – planning Damage to Cortex Alien Limb Syndrome A disorder in which person feels unable to control movements of a body part, believes that the limb is alien, or believes that the body part has its own personality It is typically associated with lesions in the supplementary motor area or those affecting blood flow to the anterior regions of the corpus callosum and the anterior cingulate Man who simultaneously tried to strangle and save his wife from himself!!! Parietal Lobe Twofold role: Integration between motor and sensory information Contributes to the ability to produce complex, welllearned acts Proprioceptive information Kinesthetic information Damage to Parietal Lobe Superior region important in visual guided movements Damage to superior regions can produce optic ataxia Optic ataxia – difficulty in using visual information to guide actions that cannot be ascribed to motor, somatosensory, or visual-field or – acuity deficits. Afferent paresis – loss of kinesthetic feedback that results from lesions to the postcentral gyrus and produces clumsy movements Apraxia Apraxia – an inability to perform skilled, sequential, purposeful movement This cannot be accounted by disruptions in more basic motor processes such as muscle weakness, abnormal posture or tone, or movement disorder (e.g., chorea). Two pieces of evidence that apraxia is a higher order disorder: 1. 2. Video It occurs bilaterally (lower level deficits are contralateral to the side of the injury) Individuals can perform behaviours spontaneously but not when imitating someone or on verbal command Oral (buccofascial) Apraxia vs. Limb Apraxia Oral apraxia is associated with difficulties performing voluntary movements with the muscles of the tongue, lips, cheek, larynx Limb apraxia disrupts the ability to use limbs to manipulate items such as screwdrivers, scissors or hammers. Ideational vs. Ideomotor Apraxia Ideational apraxia – difficulty in performing a movement when the “idea” of the movement is lost It occurs when individuals can perform simple one-step movement but not multistep movement Ideomotor apraxia – difficulty in performing a movement when a disconnection occurs between the idea of movement and its execution Simple movements of an abstract nature are most affected Other Apraxias Constructional apraxia – individuals cannot manipulate objects correctly with regards to their spatial relations (e.g., wooden block arrangement) Dressing apraxia – individuals have difficulty manipulating and orienting clothing and limbs so that the clothing can be put on correctly Callosal apraxia – difficulty with manipulating and using the left hand after verbal instructions (language in the left hemisphere)