Tourette's Disorder and Comorbidity
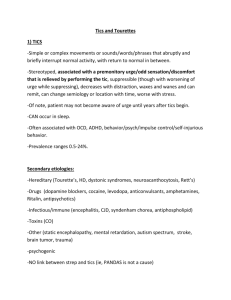
advertisement

Tourette Syndrome: The Whole Tic and Kaboodle Tourette Syndrome Association, Inc. & CDC Samuel H. Zinner, M.D. Associate Professor of Pediatrics University of Washington, Seattle depts.washington.edu/dbpeds December 15, 2012 Case 1 • • • • • 10-year-old boy “Not himself” past year Rubbing eyes and blinking Wiping/blowing nose until bleeds Allergy medications not helping Case 3 • • • • 8-year-old boy Deteriorating school performance Disruptive in classroom Recruits kids in noise-making antics • Moves about classroom Case 4 • 7-year-old boy with possible otitis media • Severe lip chapping • Licking lips Overview • Signs and symptoms • Associated problems • Management Take Home Points: • TS not rare • Tics usually mild • Tics usually 1 of many related problems • Address main problems Historical timeline of Tourette syndrome events Charcot & Tourette Georges Albert Edouard Brutus Gilles de la Tourette (1857-1904) Georges Albert Edouard Brutus Gilles de la Tourette (1857-1904) Childhood onset Heritable Premonitory sensation Motor & Vocal Coprolalila Echolalia Wax & Wane Eiffel Tower erected in Paris 1889 Tic Disorders: Historical context • Psychological • Neurological • Neuropsychiatric –Neurology –Genetics & Environment –Behavioral & Functional Tic Disorders: Characteristics • Tic Definition – motor or phonic – involuntary (unvoluntary?) – sudden and rapid – recurrent – non-rhythmic and stereotyped Tics: Characteristics Simple Motor Phonic Complex Tics: Characteristics Simple Motor Phonic •“Meaningless”/isolated •Facial and neck •Abdomen •Extremities Complex Tics: Characteristics Simple Motor Phonic •“Meaningless”/isolated •Facial and neck •Abdomen •Extremities Complex •“Purposeful” •Gestures •Dystonic postures •Self-abusive or vulgar Tics: Characteristics Simple Motor Phonic •“Meaningless”/isolated •Facial and neck •Abdomen •Extremities •“Meaningless” •“Allergy”-like •Grunting •Tongue-clicking •Animal noises Complex •“Purposeful” •Gestures •Dystonic postures •Self-abusive or vulgar Tics: Characteristics Simple Motor Phonic •“Meaningless”/isolated •Facial and neck •Abdomen •Extremities •“Meaningless” •“Allergy”-like •Grunting •Tongue-clicking •Animal noises Complex •“Purposeful” •Gestures •Dystonic postures •Self-abusive or vulgar •“Linguistic” •Syllables •Words, obscenities •Imitative (“echoic”) •Speech atypicalities .......W W A A X E S N E S ....... Tourette’s Disorder TM • DSM-IV-TR Criteria –Multiple motor plus 1 or more vocal –Many times/day and at least 1 year –Onset before 18 years –Not due to substance or medical condition Chronic Tic Disorder (M or V) TM • DSM-IV-TR Criteria –Multiple (or single) motor or vocal –Many times/day and at least 1 year –Onset before 18 years –Not due to substance or medical condition Transient Tic Disorder TM • DSM-IV-TR Criteria –Multiple (&/or single) M. &/or V. –Many times/day (4 weeks – 1 year) –Onset before 18 years –Not due to substance or medical condition Tourette’s Disorder • DSM-V –Duration criterion for chronic tics • Tics persist for > 1 yr since first tic onset • Changes from DSM-IV-TR. Removed: –More than 9/12 months of any year –Tic-free period of no more than 3 months –Transient Tic Disorder –Provisional tic disorder Tourette’s Disorder • DSM-V –Duration criterion for chronic tics • Tics persist for > 1 yr since first tic onset • Changes from DSM-IV-TR. Removed: –More than 9/12 months of any year –Tic-free period of no more than 3 months –Transient Tic Disorder –Provisional tic disorder PREMONITORY URGE Tics: Characteristics Anatomic evolution of tics top midline simple → → → bottom peripheral complex Anatomic evolution of tics Anatomic evolution of tics Anatomic evolution of tics Anatomic evolution of tics Anatomic evolution of tics Anatomic evolution of tics Anatomic evolution of tics Epidemiology • Prevalence – 1% males (or more) – Male > Female (3-to-10 times) “If the brain were simple enough that we could understand it, we’d be so simple that we couldn’t” Paul Greengard, Ph.D. Nobel Prize in Physiology or Medicine 2000 Tics: Pathophysiology • Cortical & Subcortical network – Sensory – Affective – Motor Tic Disorders: Characteristics • Premonitory urge • Tics can usually be suppressed Etiology URGE → TIC → RELIEF Tics: Pathophysiology • Dis-inhibition – “sensori-motor gating” – “filtering” • Motor programs – “fixed action patterns” – “muscle memory” Brain Regions in TS With permission, NIMH Basal Ganglia cortex Striatum GP / SN brainstem Thalamus PANDAS controversial Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections PANDAS 5 identifying criteria developed for research by clinical observation 1. Dramatic emergence or exacerbation of OCD and/or tics 2. Pre-pubertal symptom onset 3. Other neurological signs 4. Association with GABHS 5. Episodic or sawtooth symptom course Genetics • TS is genetic in origin • TS is inherited – family, twin and adoption studies • Non-genetic factors also present – Gestational exposure? – Perinatal? – Hormonal? Genetics • Major genes are involved – autosomal dominant w/incomplete penetrance? – polygenic? – additive? • Genomic regions suspected – Seeking susceptibility genes in the regions • Epigenetic factors Differential Diagnosis of repetitive behaviors Neurological Sydenham chorea Myoclonus Tremor Dystonia Athetosis Spasms Dyskinesias Psychiatric Compulsions Stereotypies Perseverations Self-injurious behavior Addictive behaviors Habits Mannerisms Differential Diagnosis of repetitive thoughts Psychiatric Obsessions Ruminations Delusions Perseverative thoughts Cravings Over-valued ideas Flash-backs Identification • Clinical aspects of tics • Comorbid conditions • Emotion and behavior Identification – comorbid conditions KEY POINT! Always assess for non-tic comorbidity * 90% occurrence if tics mild * 100% occurrence if tics severe *in clinically-referred samples Assessment: co-morbid conditions • • • • • • • • ADHD Obsessions/Compulsions Learning interferences Behavioral disorders Developmental disorders Mood disorders Anxiety Social difficulties (including PDDs) David Sedaris a plague of tics from “Naked” Little, Brown and Company, 1997 TOURETTE SYNDROME IN HISTORY Emperor Claudius (10 BC - AD 54) TOURETTE SYNDROME IN HISTORY Peter the Great (1672 – 1725) TOURETTE SYNDROME IN HISTORY Samuel Johnson (1709 – 1784) TOURETTE SYNDROME IN HISTORY Wolfgang Amadeus Mozart (1756-1791) Clinical Course • • • • • <7 7 8 11 > 11 ADHD Simple motor tic (head) Vocal tic OCS + peak tic severity tics ↓ (but lifelong in 50-90%) Time course of symptom dev’t Adapted from presentation by John Walkup, MD Personality Disorder, Bipolar, Conduct Disorder Conduct Depression, ODD ADHD, Anxiety Autism, Abuse/Neglect Clinical Assessment: complex presentations • Tics plus: – – – – – – separation (or other) anxiety autism disruptive behavior disorders depression (or bipolar) substance abuse personality disorders Quality of Life? “Tourette differs from other neuropsychiatric disorders in one simple way: It is largely the disease of the onlooker. When I tic, I am usually not the problem. You are.” Peter Hollenbeck, Ph.D. (a neuroscientist with TS) -Cerebrum (2003) Diagnostic Pitfalls 101 • Subject or clinician unaware of tics • Waxing and waning nature of tics • Tics are suppressible Diagnostic Pitfalls 102 • • • • T.S. is not rare T.S. is usually not catastrophic Few have coprolalia You may not see the tics Management • General Guidelines –Education –Monitoring –Containment Management • Containment - overcome assumptions – “He can’t control it” – “I can’t set limits on him” – “He has a tough life. I want it easier” – “He needs special accommodations” – “Medication is the answer” – “It’s all related to the Tourette” Adapted from a presentation by John Walkup, MD Management • Anger: An easily conditioned behavior –Effective in interactions –Associations: • Mood & Anxiety • Cognitive / Brain –Culture Adapted from a presentation by John Walkup, MD Management • General Guidelines - Education –Clarify neurological basis –Reassurance and support –Emphasize strengths –Whole child –Whole family Management Outcome is associated with: Severity of co-occurring conditions & self-control + The courage to overcome adversity Adapted from presentation by John Walkup, MD Management • Is further treatment necessary: –For tics? –For comorbid conditions? Caution: There is often > 1 condition Management • Lumpers vs. Splitters – Tic suppression – Co-occurring conditions – Children: Raising kids w/ TS – Adults: Building on strengths Adapted from presentation by John Walkup, MD Management • Splitters – – – – – Make problem list Rank & treat by impairment Treat each problem/diagnosis Consider consult Goal: “Fix” other diagnoses Adapted from presentation by John Walkup, MD Management • Splitter – OCD: CBT & / or Rx – Behavior: Parent training – Tics: Education, Advocacy, Monitor, Consider Rx (esp. α2 agonist) Adapted from presentation by John Walkup, MD Management • Lumpers problem problem problem problem Tourette problem problem problem problem Adapted from presentation by John Walkup, MD Management • Perspectives: – The child – The parent – The school – You Management parent perspective • Most Important – Episodic rage – Attention deficit – Learning difficulties • Least Important – Motor tics – Vocal tics FOCUS ON TARGET SYMPTOMS Types of Reinforcement Adapted from presentation by John Walkup, MD + - Internal Gratification Relieves distress External Attention & Support Avoidance Management: tics • Education & Accommodation • Medications • Experimental – Behavioral – Integrative – Surgical Management - tics • Non-pharmacological –Dynamic psychotherapy • Supportive • Cognitive-Behavioral • Parenting education Management – tics: environment • Things that worsen tics – Excitement & stress – Fatigue – Attending to tics / Accepting of tics • Things that improve tics – Calm, focused activities – Deep relaxation – Inhibiting environments • Adults’ experience w/behavior strategies Adapted from presentation by John Walkup, MD Management - tics • Non-pharmacological – Behavioral approaches • CBIT (Comprehensive Behavioral Intervention for Tics) – HRT (Habit Reversal Therapy) » » » » Awareness Training Competing Response Relaxation Social Support – FA (Functional Analysis) » Social situations that influence behaviors Management - tics • Non-pharmacological –Behavioral approaches • CBIT –Behavioral Antecedent - Behavior - Consequence –Functional + & - reinforcing functions Change in Advice Adapted from presentation by John Walkup, MD OLD (intuitive) NEW (counterintuitive) Ignore tics Can’t be controlled Don’t punish Behavior tx won’t work Don’t try to suppress Suppression ↑ tics Suppression ↑ urges Become more aware Learn to manage Reward successful mgt Use beh. strategies Beh. tx. doesn’t ↑ tics Urges will fade away Beh. tx. doesn’t create new tics Management - tics • • • • • • • • Teacher in-service on T.S. Classroom education on T.S. Teacher as role model Tic breaks/sanctuaries Testing accommodations Opportunities for movement Scribes Tic suppression (behavioral and/or medical) Management: “co-morbid” conditions – – – – – – – Family dysfunction OCD & other anxiety disorders ADHD Learning difficulties Behavioral Disorders Sleep disturbances Other self-injurious behaviors Management – bullying • Stop Bullying Now - HRSA www.stopbullyingnow.hrsa.gov Pharmacotherapy KEY POINTS! •Do not assume medication is necessary •Address comorbid condition(s) •Complete tic remission is rare •Stimulants are generally safe Pretty much everything known to humankind tried for tics • Alkaloid nicotine • Alpha adrenergic agonist clonidine guanfacine • lofexidine flutamide Anti-cholinesterase donepezil • • topiramate Anti-depressant (tricyclic) desipramine • Anti-hypertensive (misc.) mecamylamine • Anti-psychotic (other) tetrabenazine • Atypical neuroleptic aripiprazole olanzapine quetiapine tiapride Benzodiazepine clonazepam Cannabinoid delta-9-tetrahydrocannibinol (THC) • Dopamine agonist ropinirole Dopamine antagonist metoclopramide • MAO inhibitor selegiline • Muscle relaxant baclofen Neurotoxin botulinum toxin A pergolide • • • Anti-Parkinson Atypical neuroleptic (N/A in US & Canada) sulpiride • Anti-convulsant levetiracetam • • Anti-androgen finasteride • reserpine risperidone ziprasidone • Selective NE reuptake inhibitor atomoxetine • Typical neuroleptic fluphenazine haloperidol pimozide Pharmacotherapy for tics Mild tics No medication treatment Pharmacotherapy for tics Mild tics Monotherapy – α-adrenergic agonists – Clonidine (shorter-acting) – Guanfacine (longer-acting) “Small” Pharmacotherapy for tics Mild tics w/ or w/o comorbid ADHD Monotherapy – α-adrenergic agonists – Stimulants – Atomoxetine Pharmacotherapy for tics •Moderate tics – α-adrenergic agonists and/or: – Atypical neuroleptics • Severe tics – Atypical neuroleptics – Typical neuroleptics Pharmacotherapy for tics •Category A –Typical Neuroleptics •Haloperidol (Haldol) •Pimozide –Atypical Neuroleptics •Risperidone Pharmacotherapy for tics •Category B –Typical Neuroleptics •Fluphenazine (Prolixin) –Atypical Neuroleptics •Aripiprazole (Abilify) –Other •Clonidine (Catapres) •Guanfacine (Tenex) •Botulinum toxin (Botox) Pharmacotherapy for tics •Category C –Atypical Neuroleptics •Olanzapine (Zyprexa) •Quetiapine (Seroquel) •Ziprasidone (Geodon) –Other •Baclofen •Nicotine patch or chewing gum Pharmacotherapy for tics •Other options that may be effective –Benzodiazepines •Clonazepam (Klonopin) –Anticonvulsants •Topiramate (Topamax) growing interest –Tricyclic antidepressants Newer Antipsychotics Lots of aripiprazole studies Few olanzapine, ziprasidone studies Expect lots of tetrabenazine studies Ecopipam (First orphan drug) Pharmacotherapy for tics: European experts ratings 60 50 40 30 20 10 0 Drug Roessner et al. Eur Child Adolesc Psychiatry, 2011 Risperidone Clonidine Aripiprazole Pimozide Sulpiride Tiapride Haloperidol Tetrabenazine Ziprasidone Quetiapine THC Desipramine BoTox Thioridzine Guanfacine Oxcarbazepine Atomoxetine Pharmacotherapy for tics: American opinions 1st tier Clonidine Guanfacine Baclofen Topiramate Levetiracetam Clonazepam 2nd tier Pimozide Fluphenazine Risperidone Aripiprazole Olanzepine Haloperidol Ziprasidone Quetiapine Sulpiride Tiapride 3rd tier Dopamine agonists Tetrabenazine BoTox Singer et al. In Movement Disorders in Children, 2010 OCD more impairing than tics Treat OCD, then reassess tic severity Effective 3rd-line DA receptor blocking meds Treatment Algorithm 2 -line nd T I C S Monitor ADHD more impairing than tics Treat ADHD (stimulants may be OK), then reassess tic severity Tics cause Clonidine Gilbert. interference, or J Child impairment guanfacine or pain Non-DA receptor blocking meds Intolerable side effects or inadeq. benefit Monitor closely for weight ↑, extrapyramidal side effects, etc. Effective Monitor Neurology 2006 Pharmacotherapy for Comorbid Conditions KEY POINT! Target the most troubling symptoms Treatment Integrative Medicine • “Complementary” • “Alternative” Treatment Integrative Medicine • Why the interest? –Medication problems –Autonomy –Readily available information and “information” –Personal values –Liabilities in conventional medicine Integrative Medicine Tourette syndrome Fish Oil / Omega 3 • Double-blind trial 2012 • 33 youth O3FA v. PBO (20 weeks) • No difference on tics • Improvement on tic-impairment • No change OC, anxiety, depression A common sense guide to complementary/alternative medicine Effective? YES YES NO Recommend Tolerate Safe? NO Monitor closely Discourage or discourage Source: Cohen MH & Eisenberg DM, Ann Intern Med (2002) Pharmacotherapy Experimental • • • • • Naloxone Anti-androgen Cannabinoids N-Acetylcysteine Other agents now less experimental – Botulinum toxin – Nicotine patch Surgical Treatment Experimental • Deep Brain Stimulation (DBT) DBS lead Deep Brain Stimulation Printed with permission, Medtronic Extension adjust settings Neurostimulator Surgical Treatment Experimental • DBS Inclusion Criteria – 25 years old – Severe tics – Failed Rx – Failed behavioral tx – Stable co-morbidities – Active psychological interventions Advocacy and Legal Rights Advocacy and Legal Rights • • • • • Tourette Syndrome Association Protection and Advocacy Office Local Bar Association IDEA (now IDEIA) Section 504 Case 1 • • • • • 10-year-old boy Mother states “not himself” past year Rubbing eyes and blinking Wiping/blowing nose until nose bleeds Allergy medications not helping Case 3 • • • • • 8-year-old boy Deteriorating in school performance Disruptive in the classroom Recruits kids in noise-making antics Moves about the classroom Case 4 • 7-year-old boy with possible otitis media • Severe circumoral chapping • Licking lips Take Home Points: Clarifying Common Misconceptions • TS is not rare • Tics are usually mild, not catastrophic • In most people with TS, tics are one of many related complications • Address main problems, often not tics For further information, including Rx discussion: Tourette Syndrome Association, Inc. www.tsa-usa.org NEWLY DIAGNOSED Video Webstream with Dr. John Walkup Extensive Resources in Medical Home partnership: Developmental-Behavioral Pediatrics Depts.washington.edu/dbpeds Tourette Syndrome Association, Inc. www.tsa-usa.org