FACULTY DEVELOPMENT
IN PRIMARY CARE
With Support Provided by:
Health Resources and Services Administration
Grant # D55HP23200
Chief Complaint &
History of Present Illness
Chief complaint: “I would like to get my blood pressure
checked.”
HPI: A 66 year old male presents for a blood pressure
check, this is his second elevated blood pressure reading.
He came to the doctor’s office last week with elevated
blood pressure and complaints of feeling light headed and
fatigued. Patient still feels tired, has been checking blood
pressures at home with electric cuff and they have been
consistently elevated at 150s/100.
Past Medical & Surgical History
PMH: Colon Cancer (s/p chemo and radiation at
age 45)
●
PSH: Colon Resection and Anastomosis with
Lymph node dissection, chemo port insertion and
removal
●
Medications & Allergies
Prescribed Medications:
Takes no medication
●
●
Supplements: none
●
Allergies: NKDA
●
Social History
He is a retired psychologist who lives with his wife in an
apartment.
●Sleeps 6 hours a night.
●Drinks three cups of coffee daily and three glasses of
caffeinated diet soda a day.
●Never smoked
●Alcohol- drinks socially, one glass of wine a week.
●He exercises daily by going to the gym and doing elliptical
machine or light weights for an hour.
●Patient and wife travel to Japan once a year to see their
grandson (who lives there).
●
Family History
●
Mother alive at 96- takes blood pressure medicine
●
Father deceased at 70 from Heart attack
●
One son with hypothyroid
Health Maintenance
Immunizations:
●Influenza 2013
●Pneumococcal- never had
●Tdap 2011
●Zostavax- never had
●PPD- cannot remember ever having
●Health Maintenance
●Colonoscopy 6 months ago, polyp removed (has one yearly)
since Colon Cancer diagnosis
●Prostate exam- 2013 normal
●CXR- 6 months ago, normal
●Cardiac:
●EKG (6 months ago) showed NSR at 75
●
Review of Systems
●
●
●
●
●
●
●
●
●
●
●
●
General: Well groomed, proper hygiene
Constitutional: No fevers, chills, or night sweats
Skin: No lesions, no ulcers, no itching, no edema
HEENT: Denies nasal congestion, no ear pain.
Breasts: No pain, no discharge, no changes noted.
Respiratory: No active Dyspnea
Heart: No palpitations, no dizziness, no chest pain.
Hematological: No signs of easy bruising.
GI: No reflux, nausea, vomiting or diarrhea noted. No changes in bowel
habits.
GU: No dysuria, no hematuria, no incontinence, no impotence
Neurologic: No tremors, no headaches, paresthesias, dysarthria or gait
instability.
Psych: Denies anxiety or depression.
Comprehensive Geriatric
Assessment Tools
The following tools are utilized when performing a
comprehensive geriatric assessment, along with a
thorough history & physical exam.
Fall Risk: Get Up and Go Test
Barthal Index of ADL’s
IADL’s
Mini Mental Status Examination
Clock Drawing Test
Geriatric Depression Scale
●
●
●
●
●
●
These account for the patient’s gait stability, fall risk, their functional capacity and
ability to live independently, their mental status (which can vary with acute illness
and can worsen with age related disease), their higher cognitive function, and any
underlying depression that may worsen co-morbid conditions.
Gait Stability Assessment
Get up and Go Test:
●Scoring:
1 = Normal
●2 = Very slightly abnormal
●3 = Mildly abnormal
●4 = Moderately abnormal
●5 = Severely abnormal
●A patient with a score of 3 or more
on the Get-up and Go Test is at risk of
falling.
●
The patient rises out of chair comfortably, walks forward steadily, pivots without
difficulty and shows a steady gait while walking back.
He scores a 1- Normal get up and go test with no gait abnormality noted.
Assessment of mobility, balance, walking ability, & fall risk
The Timed Up and Go Test (TUG)
Instructions for administration
The patient sits in the chair with his/her back against the
chair back.
On the command “go”, the patient rises from the chair,
walks 3 meters at a comfortable and safe pace,
turns, walks back to the chair and sits down.
Timing begins at the instruction “go” and stops when
the patient is seated.
Scores range from 1 to 5 based on the observer's
perception of the patient’s risk of falling.
The patient should have one practice trial that is not
included in the score
Patient must use the same assistive device each
time he/she is tested to be able to compare scores.
Podsiadlo & Richardson 1991
TUG Normative Data for Community Dwelling
Older Adults:
Age
years
Gender
N
Mean
Time
(seconds)
SD
95%
CI
60-69
Male
15
8
2
7-9
Female
22
8
2
7-9
Male
14
9
3
7-11
Female
22
9
2
8-10
Male
8
10
1
9-11
Female
15
11
3
9-12
70-79
80-89
Steffen et al, 2002
Equipment required: standard armchair (approx. 46cm high) and stopwatch. Time to Administer: >3 min.
ICF Domain: Activity
Cut-Off Scores for TUG indicating
risk of falls by population
Population
Cut-Off score (in seconds) Author
Community dwelling adults >13.5*
Shumway-Cook et al, 2000
Older stroke patients
> 14*
Andersson et al, 2006
Older adults already
attending a falls clinic
> 15*
Whitney et al, 2005
Frail elderly
> 32.6*
Thomas et al, 2005
LE amputees
> 19*
Dite et al, 2007
Parkinson's Disease
>7.95*
Dibble et al, 2006
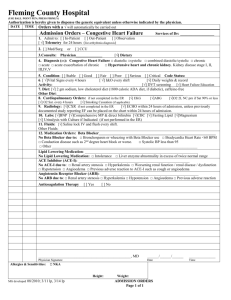
Barthel Index of ADLS
Activities of Daily Living
●Bowels
●0 = incontinent (or need to be given enema)
●1 = occasional accident (once/week)
●*2 = continent
●Bladder
●0 = incontinent or catheterized and unable to manage
●1 = occasional accident (max. once per 24hrs)
●*2 = continent (for over 7 days)
●Grooming
●0 = need help with personal care
●*1 = independent face/hair/teeth/shaving
●Toilet use
●0 = dependent
●1 = needs some help, but can do something alone
●*2 = independent (on and off, dressing, wiping)
●Feeding
●0 = unable
●1 = needs assistance
●*2 = independent
●Transfer
●0 = unable – no sitting balance
●1 = major help (1 or 2 people, physical), can sit
●2 = minor help (verbal or physical)
●*3 = independent
●Mobility
●0 = immobile
●1 = wheelchair independent, including corners
●2 = walks with help of one person (verbal or physical)
●*3 = independent (but may use any aid, e.g., stick)
●Dressing
●0 = dependent
●1 = needs help, but can do about half unaided
●*2 = independent (including buttons, zips, laces,
● Stairs
●0 = unable
●1 = needs help (verbal, physical, carrying aid)
●*2 = independent up and down
●Bathing
●0 = dependent
●*1 = independent (or in shower)
TOTAL Score: (Circle score and calculate sum at bottom)
Total possible score 0 – 20 with lower scores indicating increased disability.
The patient scored a Total of 20- no disability, no problems with transfers and the stairs.
Instrumental Activities of Daily
Living (IADL’s)
●Ability to use telephone
●*1 = Operates phone on own initiative (looks up & dials)
●1 = Dials a few well-known numbers
●1 = Answers telephone but does not dial
●0 = Does not use telephone at all
●Laundry
●1 = Does personal laundry completely
●*1 = Launders small items; rinses stockings etc.
●0 = All laundry must be done by others
●Shopping
●1 = Takes care of all shopping needs independently
●*0 = Shops independently for small purchases
●0 = Needs to be accompanied on any shopping trip
●0 = Completely unable to shop
●Housekeeping
●* 1 = Maintains house alone or with occasional assistance
●1 = Performs light daily tasks such as dishwashing, bed making
●1 = Performs light daily tasks but cannot maintain acceptable
level of cleanliness
●1 = Needs help with all home maintenance tasks
●0 = Does not participate in any housekeeping tasks.
●Mode of Transportation
●1 = Travels independently on public trans. or drives own car
●*1 = Arranges own travel via taxi but does not use public trans.
●1 = Travels on public trans. when assisted or accompanied by aid
●0 = Travel limited to taxi or car with assistance of another
●0 = Does not travel at all
●Food Preparation
●*1 = Plans, prepares and serves adequate meals independently
●0 = Prepares adequate meals if supplied with ingredients
●0 = Heats and serves prepared meals or prepares meals but does not
maintain adequate diet
●0 = Needs to have meals prepared and served
●Responsibility of own medications
●*1 = Is responsible for taking medication in correct dosage & time
●0 = Takes responsibility if medication is prepared in advance in
●
separate dosages (pill box)
●0 = Is not capable of dispensing own medication
●Ability to handle finances
●*1 = Manages financial matters independently (budgets, writes
checks, pays rent/bills, goes to bank)
●1 = Manages day-to-day purchases, but needs help with banking and
major purchases.
●0 = Incapable of handling money
Scoring: The patient receives a score of 1 for each item if his/her competence is rated at some
minimal level or higher. Total score range is 0 – 8. A lower score indicates a higher level of
dependence. The patient scored a 8, which is of independent function.
Mini Mental Status Exam
Mini Mental Status Exam: Results
The patient correctly states the year and the season, he is
not confused.
●He remembers all dates and objects.
●The patient checks his blood sugar himself twice a day.
●He is able to copy the object shown with the lines
crossing over each other.
●The remainder of his MMSE had appropriate responses.
●His total score is 30, which reflects the highest score,
no deficits
●
Cognitive Screening: The Montreal
Cognitive Assessment (MoCA) Nasreddine et al, 2005
Administration
Rapid screen of cognitive abilities designed to detect
mild cognitive dysfunction
Domains
Visuospatial/Executive: alternating trail-making,
cube and clock drawing
Naming: animals
Memory: introduce word list and delayed recall
Attention: forward digit span, backward digit span,
vigilance, serial 7’s
Language: sentence repetition and verbal fluency
Abstraction: recognize similarity
Orientation: person, place and time
Scoring
Total possible total score = 30
A score of 26 or above is considered normal
For individuals with 12 years or less of formal
education, one point is added to the score as a
correction (Nasreddine et al, 2005)
Scoring criteria are provided for each category/item.
Three different forms of the test are available to
reduce likelihood of practice effects
Test manual and score sheets are available at:
www.mocatest.org
*For those with mild deficits, the MoCA appears to
be more sensitive for those with high premorbid IQ,
non-AD dementia and early stages of dementia.
Equipment Required: score sheet, stopwatch, pencil and paper.
Time to administer: 10 minutes; ECF Domain. Body Structure, Body Function
Norms for MoCA by age and Education
Level
Rossetti et al, 2011
Years of Education
<12
12
>12
Age Group (years)
Mean (SD)
Mean (SD)
Mean (SD)
50-60
19.94(4.34)
22.25(3.46)
24.34(3.38)
60-70
19.30(3.79)
20.89(4.50)
24.32(3.04)
70-80
16.07(3.17)
20.35(4.91)
23.60(3.47)
Clock Drawing Test: Higher
Executive Function & Dementia
The patient draws the image shown in Figure A- normal
Geriatric Depression Scale
(15 point)
Scoring: Score 1 point for each one selected.
A score of 0 – 5 is normal. A score greater than 5 suggests depression.
The patient scored a 1. He does not seem to have depression.
Quality of Life assessment: SF-12
v.2
This is a generic assessment of health-related quality
of life (HR QOL) from the patient’s perspective. The
survey is administered as a questionnaire and can be
self-administered or completed through an interview.
Domains
Physical functioning (PF)
Role- physical (RP)
Bodily Pain (BP)
General Health and perceptions (GH)
Vitality (V)
Social Functioning (SF)
Composite Scores
PCS= physical health composite score
MCS= mental health composite score
An algorithm is used to generate the physical and
mental health composite scores for comparison
to normative data. In normative data, the mean
score is set to 50, scores >50 indicate better
physical or mental health than the mean, and
scores <50 indicate worse health. Normative
data were ‘renormed’ in 2009 and are available
with acquisition of administration manual.
Equipment required: Users manual
http://www.qualitymetric.com/WhatWeDo/201
1P
roductsServicesCatalog/tabid/326/Default.aspx
Role- emotional (RE)
Time to administer: 3-5 minutes
Mental Health (MH)
ICF Domain: Participation
Physical Examination
Vital Signs
BP: 158/98 on right, 156/94 on left, same blood
pressure both lying and standing
●Pulse: 78 regular
●RR: 18
●Temp: 98.6
●Pulse ox: 98%
●Weight: 212 lbs.
●Height: 6ft 1in.
BMI: 27.9
●
Physical Examination
General appearance: NAD, A&O x3
●Skin: No cyanosis, no clubbing
●Fundoscopic exam: Anterior narrowing of optic vessels.
Vision 20/20 bilateral
●HEENT: TM intact b/l no erythema, no mastoid, no
tragal tenderness. No erythema on tonsils, no
exudates. No sinus tenderness to palpation. No pain on
TMJ palpation. No cervical lymphadenopathy, no carotid
bruits, neck supple, carotid artery pulse normal, no
thyromegaly.
●
Fundoscopic Exam of
Hypertensive Patient
Image:http://www.acponline.org/mobile/ophthalmologywaxman2011/oda.html
Physical Examination
Neuro: Cranial nerves 2-12 grossly intact bilateral, sensation intact b/l
face, negative Brudzinski's sign, negative Kernig's sign
●
●
Lungs: CTA bilateral
●
CVS: RRR S1/S2, +S4 gallop
.
Abdomen: No Bruits; No pulsatile abdominal mass, NT, ND, positive
bowel sounds in all 4 quadrants, no HSM
●
●
Back: No CVA tenderness
Extremities: + 1 bilateral pitting edema of lower leg, dorsalis pedis
and posterior tibial pulse intact
●
Osteopathic Findings on
Physical Exam 1
• Cranium- CRI 8/min, good flexion and extension, craniocervical junction
with tense muscles, fascial tension, OA-Ext, RrSBl
• Cervical- Posterior cervical muscle tension, Slight head forward position with
tense scalenes and SCM muscles B/L,
• Thoracic-Good rib cage motion w/ breathing, slight increase thoracic
kyphosis, flexed T2- T8 with tense paraspinals, chronic viscerosomatic
reflexes T2-T5, Shoulders forward, internally rotated arms, pec minor and pec
major tense and tender to palpation
• Diaphragm- Exhalation dysfunction on L
• Lumbar- L1-2 chronic viscerosomatic reflexes
• Ileum- R anteriorly rotated, pelvic diaphragm congested L>R
• Lower Ext. - Hamstrings tense b/l, L>R, fibula head posterior on L, pitting
edema B/L, popliteal fossa fascial tension
Laboratory Tests
WBC: 6.2
◆Hb: 13.9
HCT: 34 PLT: 230
◆Total Chol: 190 LDL: 130 HDL: 60
◆CMP: Sodium 142 potassium 4.1
◆BUN/Creatinine: 18/0.9
◆AST and ALT: 17, 22
◆Glucose: 95 (fasting)
◆TFTs: normal
◆U/A: Normal, no protein
◆Uric acid: Negative
◆
Diagnostic Tests
•
Echo: Ejection fraction 60, left ventricle
hypertrophy
•
EKG: NsR at 75
•
CXR: normal
Assessment
This elderly male with a past medical history
of Colon Cancer presents with Hypertension. This
has been documented on at least two office visits and
by the patient’s blood pressure log. Patient also
presents with Hypertensive Signs to the Optic
Vessels.
Hypertension
Isolated Systolic Hypertension
Isolated Systolic Hypertension: Elevation in Pulse
Pressure due to diminished arterial compliance, seen
commonly in the elderly. Elderly with Isolated Systolic
Hypertension (ISH) tend to have a 2-4 fold risk of MI
and LVH. Systolic Blood Pressure greater than 160, or
less than 90.
Isolated Systolic Hypertension
Elevated Pulse Pressure Due to Diminished Arterial
Compliance Due to:
●
Increased Cardiac Output
●
Anemia
●
Hyperthyroidism
●
Aortic Insufficiency
●
AV Fistula
●
Paget’s Disease of the Bone
Types of Hypertension:
1. Essential/Primary HTN: no detectable cause of
elevated blood pressure
2. Renal Artery Stenosis: is the narrowing of one or both
renal arteries.
3. Renovascular HTN: 1-2% of HTN due to
underperfusion of renal tissues. Labs show high renin
levels.
Types of HTN Continued..
4. Coarctation of the Aorta- Congenital narrowing of the
aorta
Image from:
http://www.lpch.org/Disease
HealthInfo/HealthLibrary/car
diac/ca.html
Types of HTN Continued
5. Primary Hyperaldosteronism (Conn’s Syndrome):
Low Renin, Low potassium
6. Cushing’s Syndrome: excess of Cortisol
7. Pheochromocytoma
8. Excess Alcohol Use
9. Birth Control Pills
Treatment of Hypertension:
Lifestyle modifications- low salt diet- low caffeine,
low alcohol diet, low stress, active lifestyle
Antihypertensives- According to the SHEP study
(Systolic Hypertension in Elderly Patients) 4376
elderly patients with blood pressure of 170/77 or
greater were started on Chlorthalidone 12.5mg or
25mg and ½ of the study patients had reached their
goal blood pressure. The risk of stroke was 4 to 5
times lower if they were on Chlorthalidone.
Treatment of HTN in Elderly:
Principles in Treatment of Elderly Hypertensive Patients:
Lower initial doses of blood pressure medicine
Be careful for Orthostatic Hypotension, therefore blood
pressure medication should be carefully monitored in the
elderly and medication doses should be adjusted
gradually.
Medications for Hypertension:
●
●
●
●
●
Long Acting Calcium Channel Blocker
Chlorthalidone and Diuretics
ACE inhibitors
Beta Blockers should NOT be used as primary
therapy for hypertensive elderly patients
For second line therapy in the elderly add Amlodipine
JNC-8 Panel: New Guidelines in
Treatment of Hypertension
9 recommendations were made based on the answers
to the following questions.
1. In adults with HTN, does starting medication
treatment at specific BP thresholds IMPROVE
Health outcomes?
2. Does treating with medication to a specific BP
goal improve health?
3. Which drug classes cause more benefit in treating
co-morbid conditions.
JNC-8 Panel reviewed evidence
based trials
Studies were ranked as High, Moderate or Low
Evidence quality rating. The studies that were chosen
focused on:
• Overall Mortality
• CDV Related mortality
• CKD Related mortality
• MI, CHF, and need for hospitalization due to these
events.
• Revascularization procedures: Need for coronary
bypass, lower extremity re-vascularization.
Recommendation #1: Elderly 60+
Start Treatment at 150/90
60 years old + Initiate treatment at SBP 150 and DBP 90 and treat to
lower than 150/90, with the studies reviewed by the panel showing a clear
benefit to treating below SBP 150 mm Hg, with reduction in stroke, CHF,
CAD.
● There is also evidence that shows that treating to SBP <140 provides NO
greater reduction in risk for stroke, CHF, CAD when compared to SBP of
140-149.
● If the patient is already on medication regimen that is well tolerated,
without any adverse effects on health or quality of life and BP is <140/90,
then it is ok to continue treatment.
● There was controversy among the panel over increasing the upper limit to
an SBP of 150 in high risk groups (African American, those with existing
CVD and h/o stroke). For these high risk patients there is strong opinion
to treat to a level of 140/90 or less.
● Priorly those with target organ damage had goal of <130/80.
●
Recommendations #2 & 3:
<60 Y/O- Treat SBP <140 & DBP <90
In those <60 years old:
● Target the SBP to <140 & DBP to treat to <90
mm Hg.
● Start treatment > or equal to 140/90 and treat to
below that level.
● There was insufficient evidence for those less than 60
years old for a goal of systolic blood pressure, or in
those less than 30 years old for a diastolic goal, so the
panel recommended a systolic pressure of 140 and
diastolic pressure of 90.
Recommendation #4:
Chronic Kidney Disease
In adult population >18 years old with Chronic
Kidney Disease, start treatment when at blood
pressure of > or equal to 140/90 and treat to below
that level.
• Change from 2013 where CKD with Proteinuria
<130/90.
Recommendation #5: Diabetes
In adults over 18 years old with Diabetes start
treatment at or greater than 140/90.
• Change from 2013 where treatment goal was
<140/80 according to the ADA.
Recommendation #6 & 7: Start
treatment with Thiazide Diurhetic or
Calcium Channel Blocker
General population, inclusive of Diabetics
• Initial therapy:
• Thiazide Diuretic
• ACE-I or ARB
• Calcium Channel Blocker
• Each of these classes of drugs had comparable effects on
decreasing overall mortality, CDV, cerebrovascular, and kidney
disease as well.
• As many people will require more than one medication to control
BP, using any of these classes as an add on medication is highly
recommended.
Exception:CHF
Only exception, CHF:
● Thiazide diurhetic was found to be more effective
than CCB or an ACE-I. (ACE-I was found to be
more effecetive than CCB in CHF as well).
What about B-Blockers?
•
•
•
B Blockers were not recommended by the panel as First Line
treatment due to a study that found when used as initial
treatment for BP, resulted in a higher rate of CDV events and
stroke, as opposed to using an ARB.
The same goes for Alpha Blockers
The panel could not find high quality studies that compared
dual Alpha 1 & B-Blockers (Carvedilol), vasodilating Bblockers (Nebivolol), central Alpha 2 adrenergic agonists
(Clonidine), direct vasodilators (Hydralazine), Aldosetrone
receptor antagonists (Spironoloactone) and loop diurhetics
(Furosemide), and so NONE of these were recommended as
First Line therapy.
Recommendation #7: Initiating
treatment in our African American
population
General African American population, inclusive of Diabetics
•
Thiazide Diuretic or CCB is recommended (over ACE-I).
•
Based on study that showed that Thiazide diurhetic was
more effective at preventing Heart Failure when compared
with an ACE-I in the African American population.
•
Higher risk of stroke when using ACE-I as initial
treatment(over CCB).
ACE-I were found to be Less effective at treating BP.
•
•
No differences in outcomes of CVD, Stroke when comparing
Thiazide Diurhetic and CCB.
Recommendation #8: Chronic
Kidney Disease; use ACE-I or ARB
In those with CKD 18 years and older:
• Either INITIAL treatment or add on should include an ACE Inhibitor or ARB.
• This includes all patients with CKD + HTN, regardless of race or diabetes.
What about prior recommendation to use CCB vs ACE-I in African Americans?
• CKD and proteinuria? Use ACE-I or ARB as first line treatment because of the
greater risk of progressing onto ESRD.
• CKD without proteinuria? Initial therapy choice less clear, open to thiazide
diuretic, CCB, ACE-I or ARB.
• If ACE-I/ARB not used as first drug choice, may use it as an add on agent.
• It is anticipated that in CKD an ACE-I/ARB will be used within the total drug
regimen either way.
Recommendation #9:
Maintain Goal Blood Pressure
• Main objective in treating hypertension is to maintain
goal BP.
• If goal not met within a month, increasing dose of initial
medication started or adding a second agent, add a third
agent later on if necessary.
• Avoid using ACE-I and ARB together in same patient.
From: 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the
Panel Members Appointed to the Eighth Joint National Committee (JNC 8)
JAMA. 2014;311(5):507-520. doi:10.1001/jama.2013.284427
Figure Legend:
Strategies to Dose Antihypertensive Drugsa
Date of download: 4/5/2014
Copyright © 2014 American Medical
Association. All rights reserved.
From: 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the
Panel Members Appointed to the Eighth Joint National Committee (JNC 8)
JAMA. 2014;311(5):507-520. doi:10.1001/jama.2013.284427
Figure Legend:
Guideline Comparisons of Goal BP and Initial Drug Therapy for Adults With Hypertension
Date of download: 4/5/2014
Copyright © 2014 American Medical
Association. All rights reserved.
Heart Adapting Abilities
• “The heart at age 65 has adapted to meet the
demands of a 65 year old body”
• It is these physiologic changes that bring an
increased risk for developing HTN, heart disease,
risk of stroke and MI.
Assesment & Plan: HTN
Management
Patient was started on Chlorthalidone 12.5mg po q
day and given a low salt diet to follow. Pt told to limit
caffeine intake to 6 oz a day. Pt also told to limit alcohol
use and continue exercise regimen. Pt was told to monitor
and log his blood pressure twice a day.
After 2 weeks on the medication his blood pressure
was 140/90. At the two week visit the patient had no side
effects. Pt’s medication was increased to Chlorthalidone 25
mg po q day and was given a referral to an Ophthalmologist
for full eye exam.
Nutrition Management
DASH Diet (Dietary Approaches to Stop HTN)
•Focus on keeping Na consumption below 1500-2000 mg
-read labels
-prepare more food at home and fewer restaurant meal
•Assure adequate potassium in light of medications
•Increase fruits and vegetables (5-10 servings/day) for their flavonoid, phytochemical,
potassium content and properties
•Reduce calorie consumption to reach BMI < 25 t
•Encourage use of omega-three fatty acids
•Avoid excessive alcohol intake
•Choose high-fiber, less processed grains and legumes as carbohydrate sources to reduce DM
risk
http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf
Patient’s Treatment
On four week follow up patient had a blood
pressure of 122/78 in bilateral arms and no complaints.
Patient is tolerating the Chlorthalidone 25 mg po q day
well. Patient continues to follow a low salt diet.
Patient saw ophthalmologist and was diagnosed with
hypertensive retinopathy and told to keep his blood
pressure under control.
Osteopathic Treatment
Osteopathic treatment in this geriatric patient with
newly diagnosed hypertension is very broad. It consists
of addressing somatic dysfunctions of the autonomics
and correcting dysfunctions that affect movement and
can add to exercise tolerance and weight loss.
Additional Osteopathic
Considerations
In developing a treatment plan for elderly patients
there are many considerations such as bone density and
degree of spinal restrictions, overall muscle tone and
strength, degree of pain patient is in. For most seniors
HVLA should not be the initial treatment option.
Muscle energy, counterstrain, Myofascial release ,
Facilitated positional release, and balanced ligamentous
tension are better tolerated.
References
Lee, T and R., CARDIOLOGY. Pages 275-278. Medical
Economic Comp. 1989
Egan, B., Treatment of Hypertension in the Elderly Patient,
Particularly Isolated Systolic Hypertension. uptodate 2013
Rubin et al Geriatrics at your Fingertips. Pages 42-44. AGS
2012.
References
Cheak-Zamora, N. C., Wyrwich, K. W., & McBride, T. D. (2009). Reliability and validity of the SF-12v2 in the
Medical Expenditure Panel Survey. Quality of Life Research, 18 (6), 727–735.
Podsiadlo, D. and Richardson, S. (1991). "The timed "Up & Go": a test of basic functional mobility for frail
elderly persons." J Am Geriatr Soc 39(2): 142-148.
Nasreddine, Z. S., Phillips, N. A., et al. (2005). "The Montreal Cognitive Assessment, MoCA: a brief screening
tool for mild cognitive impairment." Journal of the American Geriatrics Society 53(4): 695-699.
Rossetti, H. C., Lacritz, L. H., et al. (2011). "Normative data for the Montreal Cognitive Assessment (MoCA) in a
population-based sample." Neurology 77(13): 1272-1275.
Steffen, T. M., Hacker, T. A., et al. (2002). "Age- and gender-related test performance in community-dwelling
elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds." Physical
Therapy 82(2): 128-137.
Ware JE, Kosinski M, Keller SD (1996). A 12-Item Short-Form Health Survey: Construction of scales and
preliminary tests of reliability and validity. Medical Care. 34(3):220-233. (SF-12v1)
References
American Academy of Family Physicians A Physician's Guide to Nutrition in Chronic Disease
Management of Older Adults Accessed from
http://www.einstein.yu.edu/nutrition/pdf/nutrition%20and%20the%20elderly.pdf
Brown, E. and Sharlin, S. (2009) Life cycle nutrition: An evidence-based approach, Sudbury, MA:
Jones and Bartlett Publishers.
Escott-Stump, S. (2012) Nutrition and diagnosis-related care. Baltimore, MD: Lippincott
National Health Lung and Blood Institute (2006) Lowering your blood pressure with DASH.
Accessed from http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf
Special Thanks to…
Clinical Case by: Dr. Bernadette Riley, DO
Mary Adar, DO, Assistant Professor, Dept. Family Medicine,
NYIT College of Osteopathic Medicine
Joseph Simone, DO
Corri Wolf, PA-C, MS, RD, Assistant Professor, Dept. Physician Assistant Studies,
NYIT School of Health Professions
Rosemary Gallagher, PT, DPT, GCS, Assistant Professor, Dept. Physical Therapy,
NYIT School of Health Professions
B. Suzanne Diggle-Fox, PhD, RN, Assistant Professor, Dept. Nursing,
NYIT School of Health Professions
Tobi Abramson, PhD, Director, Mental Health Counseling,
NYIT School of Health Professions
Mind Haar, PhD, RD, CDN, Director, Program Development Interdisciplinary Health Sciences,
NYIT School of Health Professions
Gioia Ciani , OTD, OTR/L, Assistant Professor, Dept. Chair Occupational Therapy,
NYIT School of Health Professions
Grant Director: David P. Yens, PhD, Associate Professor, Family Medicine,
NYIT College of Osteopathic Medicine