The Psychology of Addiction- A current perspective on Chemsex
advertisement

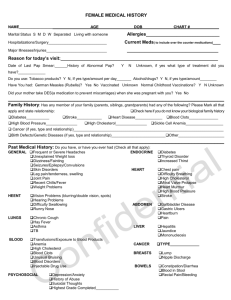
Outline Biography Introduction • Intoxicating substances, old and new • Dependence and withdrawal • Comprehensive SM history • Conventional approaches to SM treatment Integration • Drugs and alcohol in the sexual health setting • Advice for screening and intervention • Services local to C&W Medical and psychiatric training • Chelsea & Westminster Hospital: Liaison / HIV • Central & North West London: Addictions • Special interests: Club Drug Clinic • WLMHT Integrated care for patients with LTCs Now • WLMHT / Ealing : Consultant Liaison Psychiatrist • Home ward Ealing – Intermediate Care Service • Imperial College: Honorary Senior Clinical Lecturer • Medical Council on Alcohol: Executive Committee Acknowledgements • Dr Owen Bowden-Jones • David Stuart, Antidote • Mark Dunn • Stacey Hemmings • • • • Dr Pepe Catalan Flick Thorley Dr Amrit Sachar Prof Anne Lingford-Hughes Declarations CH has in the past received honoraria for travel / lecturing (not related to this work) from: Bayer, Lilly, Pfizer and Janssen Categories of intoxicating substances Depressants Opioids, benzodiazepines, alcohol Stimulants Cocaine, amphetamines, MDMA, caffeine Hallucinogens LSD, PCP, ketamine Cannabis, nicotine Highs and harms Desirable effects • Pleasure • Relaxation, anxiety reduction, disinhibition • Increased energy, enjoyment, confidence • Fatigue reduction, pain reduction • Curiosity, new experiences, ‘psychonaut’ Highs and harms Undesirable effects • Mode of administration • Physical and systemic effects • Psychiatric effects • Dependence potential and withdrawal • Behavioural consequences • Indirect harms / harms to others • Crime • Synergistic effects The most harmful drug overall? Nutt et al Lancet 2010; 376:1558 The most harmful drug overall? Nutt et al Lancet 2007; 369:1047 Novel psychoactive substances • Club drugs recreational drugs used in nightclubs, festivals, gigs, bars, circuit and house parties • Eg: amphetamine, methamphetamine, MDMA, cocaine • NPS designed to mimic controlled drugs but synthesised to evade prohibitions • Many now banned after period as legal highs • Eg: mephedrone, methoxetamine, GHB/GBL • Easily available online, head shops, dealers Novel psychoactive substances Categories of drugs Depressants Opioids, benzodiazepines, alcohol, GBL/GHB, Phenibut, Stimulants Cocaine, amphetamines, MDMA, caffeine m-cat, NRG-1, BZP, MDAI, Synthacaine, 5/6-APB Hallucinogens LSD, PCP, ketamine, AMT, methoxetamine Cannabis, nicotine Spice Novel Psychoactive Substances - Key points • It is impossible for clinicians to remain abreast of all NPS on the market (1 new drug per week) • NPS are synthesised to mimic existing drugs / use the same neurotransmitter mechanisms • Most NPS are not detected by routine urinary drug testing – false negatives • Ask, and have degree of suspicion based on clinical assessment Scale of drug use in England & Wales • Adults 16-59: • Prevalence of having taken illicit drugs: – 36.4% ever – 8.6% in last year – 3% Class A • Young adults 16-24: – 48.6% ever – 20.4% in last year – 6.6% Class A NHS IC 2011 Scale of NPS use EMCDDA 2005-111 • 164 NPS were formally notified (now ~1 per week) • UK - 23% European NPS users Crime Survey E&W 2011-122 • 1.1% respondents had used mephedrone in the last year, 3.3% in 16-24 age group Global drugs survey 20132 (clubbing last month): • 36.1% reported lifetime use of mephedrone 1 EMCDDA-Europol 2011 Annual Report on the Implementation of Councel Decision 2005/387/JHA. EMCDDA/Europol, 2012. | 2 Home Office. Drug misuse declared: findings from the 2011 to 2012 Crime Survey for England and Wales. Home Office, 2012. | 3 Winstock, A. "Global Drug Survey." Mixmag, May 2013. A whirlwind tour of addiction • Chronic relapsing brain disorder characterised by neurobiological changes that lead to compulsion to take a drug (or activity) with loss of control over the activity. • Transition from recreational to obsessive use • From positive to negative reinforcement • Psychological factors drive the behaviour Koob GF and Le Moal M, Science, 1997 But what drives the psychological factors? Inside the brain of a recreational user of drugs Boileau et al Synapse 2003 Inside the brain of a dependent user of drugs 1. Volkow 2. Koob Outline Biography Introduction • Intoxicating substances, old and new • Dependence and withdrawal • Comprehensive SM history • Conventional approaches to SM treatment Integration • Drugs and alcohol in the sexual health setting • Advice for screening and intervention • Services local to C&W ICD-10 diagnosis of dependence • Three or more at once in the last year: • • • • • • Withdrawal symptoms Tolerance to the effects of the drug Strong desire or compulsion to use the substance Persistent use despite adverse consequences Difficulty controlling use / amount / recidivism Neglect of other activities / primacy • (Narrowing of repertoire) Comprehensive SM history • Who? (everyone) • What substances? (Avoid ‘illegal’) – Quantity – Frequency – Route – Circumstances – History of use (first, regular, heaviest, cumulative) • Negative effects (teachable moment) • Features of dependence and withdrawal 2L Cider (£3) 7.5% 15 units 1 pint Peroni 5.1% 2.95 units 440mL Special Brew (£1.32) 9% 70cL whisky 4 units 40% 28 units 250mL wine 13% 3.25 units 75cL wine 13% 9.75 units Clinical treatment strategies • • • • • • Education & brief intervention Harm minimisation Stabilisation / maintenance Detoxification Rehabilitation Abstinence • NHS Drug Clinics • PHE commissioned (via LAs) Outline Biography Introduction • Intoxicating substances, old and new • Dependence and withdrawal • Comprehensive SM history • Conventional approaches to SM treatment Integration • Drugs and alcohol in the sexual health setting • Advice for screening and intervention • Services local to C&W Alcohol and sexual health Family Planning Association Survey 2009 1000 18-30 year olds, Online survey by Mori • 37% had unprotected sex with a new partner • Of these: 40% said alcohol was a factor • 38% reported sex which they regretted later • Of these: 70% said alcohol was a factor • 28% reported having sex with someone they wouldn’t normally find attractive • Of these: 78% said alcohol was a factor Alcohol and sexual health Binge drinking, sexual behaviour and sexually transmitted infection in the UK Int J STD & AIDS 2007; 18; 810-13 • • • • 86% GU attendees are binge drinkers 32% felt alcohol played a role in their attendance 77% drunk before sex with a new partner Binge drinking assoc with bacterial STI diagnosis and unwanted pregnancy Recreational drugs and GUM: meth Scale of methamphetamine use (UK) • CSEW 2011-121: 0.1% used in last yr • GMSS 20072: 4.7% used in last yr • HIV testing cohort3: (2002-3): 8.3% in last yr • HIV treatment cohort3 (2002-3): 12.6% in last yr • Gym cohort (2004)3 21% in last yr 1Home Office. Drug misuse declared: findings from the 2011 to 2012 Crime Survey for England and Wales. Home Office, 2012. | 2Keogh P et al. Wasted opportunities: Problematic alcohol and drug use among gay men and bisexual men. Sigma Research 2009 | 3Bolding G et al. Addiction 2006; 101, 1622–1630 • CNWL (NHS) • Antidote (Charity) • National / open access • Opened: Jan 2011 • First 18 months: • 291 patients seen CDC - Presenting drug use (n=291) GBL/GHB Crystal methamphetamine Mephedrone Cocaine Ketamine Alcohol MDMA Cannabis Other NPS Benzodiazepines Opioids Amyl Nitrate CDC - Presenting drug use (n=52 heterosexual) Ketamine Cocaine Alcohol Mephedrone GBL/GHB Crystal methamphetamine MDMA Cannabis Benzodiazepines Other NPS Opioids Crystal methamphetamine and HIV • Users of crystal methamphetamine in the clinic (n=120) were two times more likely to be HIV positive than non users (n=170). 68% vs 33% (p <0.05) • Users of crystal methamphetamine in the clinic were four times more likely to be HCV positive than non users. 12% vs 3% (p <0.05) Crystal methamphetamine and HIV Do you attribute your HIV status to your drug use? 30% of HIV positive patients responded YES Crystal methamphetamine and HIV Does your drug use get in the way of taking your prescribed medications regularly? 39% patients on antiretrovirals responded YES Injecting drug use Crystal methamphetamine users: • 53% reported having injected the drug • 47% never Non crystal users: • 6% reported currently injecting (meph, cocaine, G, K) • 19% reported previously injecting • 75% never MSM and substance use – why? • • • • Helps to relax and be more sociable Mitigating social unease (general, sexuality, scene) Alleviating loneliness / unhappiness Enabling sexual encounters (sexuality, HIV, ‘raucous’ – integral to sex) • Gay norms of alcohol and substance use (integral to socialising) Keogh P et al. Wasted opportunities: Problematic alcohol and drug use among gay men and bisexual men. Sigma Research 2009 Associations between substance use and HIV related risk indicators • Systematic review of 23 studies (2012)1 looked at studies into various substances: only methamphetamine and binge alcohol drinking associated with sexual risk (see plot) • Systematic review of 61 studies (2012)2 highlighted HIV+ MSM who use meth more likely to report high-risk sexual behaviour, incident STI, serodiscordant UAI compared with HIV+ MSM who do not use methamphetamine 1 Vosburgh, HW et al. A Review of the Literature on Event-Level Substance Use and Sexual Risk Behavior Among Men Who Have Sex with Men. AIDS Behav 2012: 16:1394–1410 2 Rajasingham R et al. A Systematic Review of Behavioral and Treatment Outcome Studies Among HIV-Infected Men Who Have Sex with Men Who Abuse Crystal Methamphetamine. AIDS PATIENT CARE and STDs 2012: 26; 36-51 High risk sexual behaviours • • • • • • • • Increased frequency of sex Prolongation of sex (‘marathon’) Increased number of partners Reduced condom use / UAI Increased condom failure Disinhibiting effects Mucosal trauma Co-infection with other STI Colfax G, Guzman R. Club Drugs and HIV Infection: A Review. CID 2006: 42:1463–9 High risk sexual behaviours Clinical experience • Online apps / websites • ‘Party and play’ / parTy • Multiple partners • Higher risk sexual practices • Intravenous use in sexualised contexts • ‘Slamming’ / re-injecting Kirkby T, Thornber-Dunwell M. High-risk drug practices tighten grip on London gay scene. Lancet 2013: 381; 101-2 Interventions Patient • 37 year old HIV+ gay man, working full time in City • Recent acquisition of HCV following casual UPSI at party arranged online • Binges on drugs 3-4x per month including ‘tina’ smoked or ‘slammed’ and ‘meph’ • Reports feeling depressed and being ‘monitored’ online at times • Would like to abstain from drugs, but doesn’t see self as a ‘junkie’ so won’t visit mainstream services • Multiple lapses related to sex: ‘haven’t had drug free sex for years’, ‘can’t manage sex without drugs’ Substance misuse in sexual health • Investigate the link between substance misuse and sexual health • Design interventions to minimise harm from both Social care Disintegrated services Relationships Sex Social life Family / children Employment Habits Spirituality &c Justice System Addiction services • NHS • Third Sector Mental health Physical health • HIV • Sexual health • Other medical problems Primary care • • • • • • Wellbeing Self esteem Depression, anxiety Cognitive function Psychosis Self harm Substance misuse in sexual health • Clinicians should – be aware of the commonly used recreational drugs and their potential short term complications and risks – consider screening individuals at risk – give simple safety advice and information – have agreed referral pathways into local services AK Sullivan, O Bowden Jones, Y Azad (2014) Drug Screening Qs 1. Did you use drugs before/during sex in the last 3m Yes / No / Yes but not during sex 2. Which drugs did you use? Crystal methamphetamine - Mephedrone - GHB/GBL- Ketamine- Cocaine- Other (specify)- 3. Did you inject? Yes / No / Yes but not in the last 3m Identification and Brief Advice • “The teachable moment” Change in awareness Change in attitude Change in behaviour Prochaska & DiClemente Identification and Brief Advice • “The teachable moment” • Reflect back to the patient any identified harms • Offer advice on making changes • Offer further advice/support/referral • Cochrane review supports effectiveness of IBA1 • To reduce drinking to lower-risk levels, NNT = 8 2 1 Kaner 2007, 2 Moyer 2002 Referral pathways • • • • Access to integrated SMHW Mental Health referral pathways Integrated health and social care services Addictions services: – PHE/LA commissioned – Increasingly partnerships between 3rd sector and NHS – Concern about reduced capacity to deal with complexity including physical / MH comorbidity – Culturally competent? Eg MSM specific Clinical treatment strategies PS - Mental health in sexual health Psychological Wellbeing Agenda • Support at time of diagnosis • Screening for psychological needs: depression, anxiety, SM, stress, self harm, cognitive impairment • Initial management interventions • Referral pathways - evidence based, HIV-specific, timely, competent, access to psychological care Resources Specialist services: CODE ChemClinic ReShapeNow.org • THT www.drugfucked.tht.org.uk • talktofrank.com • erowid.com