Complicated Contraception - New York State College Health
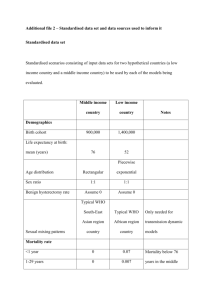
advertisement

Alexandra Hall MD amh89@cornell.edu Beth Kutler FNP bk82@cornell.edu Cornell University Understanding the Data The New Pap Smear Guidelines The New Medical Eligibility Criteria for Contraceptive Use Update on STI Treatment and Diagnosis What’s New in Emergency Contraception Understanding …. and Explaining the Data Explaining Risk Absolute Risk Attributable Risk Relative Risk Absolute Risk The percentage of people in a group who experience a discrete event Number of events experienced Total exposure time of people at risk Example of Absolute Risk The “pill scare” of 1995… Of 100,000 women using third generation progestins (desogestrel, norgestimate), 30 people developed a VTE (venous thromboembolic event) per year Absolute Risk = 30 per 100,000 women years (.03 %) Attributable Risk The difference in risk between those exposed and those not exposed Reflects extra risk associated with exposure Risk in exposed – Risk in unexposed Example of Attributable Risk The absolute risk of VTE in women who took second generation OCs (norgestrel, levonorgestrel) was 15 per 100,000 woman years compared with 30 per 100,00 woman-years in those using third generation OCs. The attributable risk of VTE in women taking third generation OCs is 15 per 100,000 30/100,000 - 15/100,000= 15/100,000 (.015%) Relative Risk Frequency of the outcome in the exposed group divided by the frequency of the outcome in the unexposed group. Reflects the likelihood of developing an outcome based on an exposure Relative Risk Example (30/100,000) (15 / 100,000) Absolute risk of taking third generation OCs Absolute risk of taking second generation OCs =2 Interpreting RR Relative Risk 1.0 Interpretation No increase in risk of outcome in exposed group compared with unexposed group >1.0 Increased risk of outcome in exposed group <1.0 Decreased risk of outcome in exposed group Women taking 3rd generation OCs had a risk of VTE two times that of women taking second-generation OCs. Confidence Interval Confidence Intervals are a way of taking data from a sample and saying something about the population from which the sample was drawn. If the value 1.0 is in the range of the confidence interval, it can be concluded that the data is not statistically significant Odds Ratio Quantifies risk for case-control studies in the same way that relative risk quantifies risk for cohort studies Frequently seen in medical studies Pap Guidelines What was ACOG thinking?! Pap Screening for Cervical Cancer • Is Effective (1) – Cervical CA incidence has declined more than 50% since 1975 due to the introduction of pap screening programs • 1975: 14.9 per 100,000 women • 2006: 6.5 per 100,000 women – Mortality rates have similarly declined • But only if you do it (2) – 50% of those women diagnosed with cervical cancer have never been screened – Another 10% have not had a Pap within the past 5 years before diagnosis – 25% of cancer cases are in women over age 65 (30% of women over age 60 report no pap in past 3 years) – Uninsured, ethnic minorities (particularly Hispanic and Black Americans) and poor women (esp rural) are also disproportionately underscreened (1) http://seer.cancer.gov.csr.1975_2006 (2) http://consensus.nih.gov/1996/1996CervicalCancer102PDF.pdf) START SCREENING AT AGE 21, REGARDLESS OF COITARCHE Adolescents have a very high rate of HPV infection • Ho GY et al 1998 NEJM – 608 women at New Brunswick State, NJ – 6 month intervals for 3 years – Cumulative incidence of HPV was 43% • Woodman et al Lancet 2001 – 1075 women aged 15-19, initially HPV neg – 6 month intervals for 3 years – Cumulative incidence of HPV was 44% Adolescents have a very high rate of HPV infection • Brown et al, J Infectious Dis 2005 – 60 adolescents aged 14-17, inner city, 85% Afr. Am. – Q3 month exam + swab, weekly self-swab x 2 years – Cumulative prevalence 82% • Winer et al, Am J Epidemiol 2003 – 603 college students in Washington State over 10 years – Q4 month visits for 4 years for most women – 24-month cumulative incidence was 32% – 60-month cumulative incidence was 60% Cumulative HPV incidence among sexually active women who were HPV negative at enrollment Shouldn’t we be worried? NOPE Most adolescents will clear HPV spontaneously • Ho GY et al 1998 NEJM (college in NJ) – Median duration of infection was 8 months • Moscicki et al J Pediatrics 1998 – 618 young women positive for HPV, Q 4 month pap, colpo, HPV – 70% of women cleared HPV within 24 months Most adolescents will clear HPV spontaneously • Brown et al, J Infectious Dis 2005 (teens) – Average duration of HPV infection was 168 days Most adolescents will clear HPV spontaneously • Insinga et al, Cancer Epidemiol Biomarkers Prev 2007 – 2391 women aged 16-23 in HPV vaccine trial placebo arm – Q6 mo eval x 4 years – Mean durations for HPV 16 and 18 were 18 and 16 months respectively – 85-90% cleared within three years Insinga et al Cytologic (pap) abnormalities also spontaneously clear in adolescents • Moscicki 2004 Lancet, 187 women aged 13-22 – Median follow-up of 61 months – 61% of LSIL regressed at 12 months – 91% regressed by 36 months Cytologic (pap) abnormalities also spontaneously clear in adolescents • Winer et al, J Infectious Dis 2005 (college) – Mean duration of LSIL was 5 months – 86% cleared their SIL – less than 9% developed CIN 2/3 in 4 yrs Even histologic dysplasia will spontaneously clear in adolescents • Moore 2007 AJOG – 177 Adolescents with biopsy-proven CIN 2 – Given opportunity to choose LEEP or observation – Followed for 18-26 months Even histologic dysplasia will spontaneously clear in adolescents Fuchs 2007 J Pediatr Adolesc Gyn • • • • • Adolescents with CIN2 Observed, not treated 39% regr at 1 yr 50% at 2 yrs 75% at 3 yrs Even histologic dysplasia will spontaneously clear in adolescents Ok, but what about those 10-15% whose HPV or dysplasia didn’t clear within 3-4 years? NO WORRIES Cervical Cancer takes time to develop • Is a result of PERSISTENT HPV infection • Adolescents get a lot of HPV, BUT in the majority, it does not persist • In those in whom it does persist, cervical cancer takes years to develop (analogy to colon cancer) • Remember, in the studies cited, none of the women who were simply observed (including the 5% who progressed) developed cancer • Therefore, cervical cancer is virtually non-existent in adolescents Cervical CA is almost nonexistent under age 21 Watson et al, Burden of cervical cancer in the United States 1998-2003. Cancer 2008 SEER Cervical Cancer Data (Rates per 100,000 women) Comparison of Cancer Incidence in Adolescents (rate per 100,000) 12 9.9 10 Cervix Breast 8 Testicle Hodgkins 6 4.4 3.5 4 1.8 2 0 3.1 2.9 2.1 age 14-19 www.seer.cancer.gov Leukemia 2.4 2.6 2.3 1.6 0.3 0.1 0.1 NHL Brain/CNS 0.9 0.8 age 20-24 Colon But can’t we just screen anyway? • • • • It’d make me feel a lot better. (I know she’s been having sex for years!) And it’s just a pap smear! I have to do a pelvic to screen for STI’s anyway, right? Wrong! • And don’t you have to do a pap smear before you prescribe birth control pills? NO! • I mean really, what harm can it do? Unnecessary screening and treatment can have significant morbidity • Cost, hassle • Fear of exams & fear of providers = barrier to accessing sexual health care (contraceptive counseling and provision, STI counseling and testing, vaginal health) • “Emotional impact of labeling an adolescent with both a sexually transmitted infection and a potential precancer must be considered because adolescence is a time of heightened concern for self-image and emerging sexuality.” (ACOG Practice Bulletin) • Adverse obstetrical outcomes in a population whose childbearing years are still ahead of them Adverse OB outcomes from cervical cancer screening and resultant treatment - Kyrgiou Lancet 2006 So…. • Screening for a disease that practically doesn’t exist in that age group (under 21) does not make sense • And it can cause unnecessary grief and harm, as well as cost Start screening at 21 In short, we don’t want to know what’s going on before then because it will probably go away on its own! (And we’re more likely to cause unnecessary harm than we are to find significant disease.) All we are saying… is give teens a chance! SCREEN EVERY TWO YEARS (AGES 21-29) AFTER AGE 30, IF 3 CONSECUTIVE NORMALS, SCREEN EVERY 3 YEARS Exceptions • The following groups typically need annual pap screening due to increased risk of CIN: – HIV positive – Immunosuppression (transplant recipients) – DES exposure (not relevant to student health) – Previously treated for CIN2, CIN3, or Cancer 30-Somethings are different from 20-somethings! • More likely to be monogamous (not being exposed to HPV, or at least not to new HPV) • More likely to have already had HPV infection at some point and perhaps have some immunity • Less likely to be able to spontaneously clear a new HPV infection • Overall have a higher incidence of cervical cancer (likely reflecting persistence of disease that began in their 20’s) Going the distance: How often to screen? • How predictive is a normal pap smear? • For how long after a normal pap smear can you feel reasonably confident that you haven’t developed cervical cancer? • Depends on two factors: – Sensitivity of the pap (how much faith can you put in a normal one) – Virulence or aggressiveness of HPV/cervical dysplasia (how long does it take to turn really bad?) Going the distance: How often to screen? • In the past 10 years, many studies have been conducted to try to answer this question, thanks, in large part, to a study done 15 years ago… Cancer 1987, Eddy The Frequency of Cervical Cancer Screening Comparison of a Mathematical Model with Empirical Data Found that previous models under-estimated the effectiveness of screening at less than annual intervals, spurred interest in revisiting the wisdom of annual screening. Sawaya 2000 Obstetrics and Gynecology Prospective cohort study of 128,000 women in the CDC Breast/Cervical Cancer Program Sawaya 2000 Prospective cohort study of 128,000 women in the CDC Breast/Cervical Cancer Program No statistically significant difference in rate of high grade abnormalities among the different screening intervals. Sasieni Br J Cancer 2003 Case-Control study of 1200 women with cancer and 2400 matched controls Sasieni Br J Cancer 2003 Case-Control study of 1200 women with cancer and 2400 matched controls • >938,000 women under age 65 • CDC National Breast and Cervical Cancer’s Early Detection Program – Provides pap screening to poor and low-income women – Low SES is, in itself, a risk factor for cervical cancer so this group may even have a slightly higher incidence of dysplasia than the general population • Looked at protective value of number of previous normal paps Prevalence of CIN (in %) 0 prev nl pap 1 prev nl pap 2 prev nl pap 3 prev nl pap NEJM 2003 • If you are less than 30: – and have had one negative pap, the likelihood of having cancer is virtually zero, but we knew that already, as the overall risk of cancer in that age group is so low. – having had 2 or 3 previous normal paps is not more “protective” against CIN 2 or 3 than having had one previous normal pap. • If you are 30-45: – your risk of cancer is 0.01%, or 1 in 10,000. – the more previous normal paps you have had, the more “protected” you are from developing CIN 2 or 3. NEJM 2003 Projected numbers for each 100,000 women paps colpos # cancers Depending on how CIN 2 will act NEJM 2003 Risk of Cancer: Annual Screening Every 3 year screening Age 30-44 2 in 100,000 5 in 100,000 Age 45-59 1 in 100,000 2 in 100,000 Age 60-64 1 in 100,000 1 in 100,000 • Overall, compared with annual screening for three years, screening performed once 3 years after a normal in women who have had >3 normals is associated with an average excess risk of 3 in 100,000 • To avert one additional case of cancer by screening 100,000 women (aged 30-44) annually rather than every 3 years: – 69,665 extra pap smears – 3861 extra colposcopies Sasieni BMJ 2009 Case-Control study of 4000+ women with cervical cancer, each matched to two controls Looked at risk of cancer depending on whether last screen was 1-3 y. ago vs 3-5 y. ago Sasieni BMJ 2009 • Negative screening in your 20’s is not really all that “protective” – doesn’t predict a lower risk of getting cervical cancer – This makes sense due to likelihood of new incident HPV infection from new sexual partners and overall very small risk of cancer in this age group • Screening in early 30’s, however, does give meaningful predictions of decreased risk – If you don’t have HPV now, you’re less likely to get it anytime soon When to screen • ACOG guidelines reflect the data – If 21-29, due to increased risk of new HPV infection and lower likelihood of regression than in adolescents, and data that shows that previous negative paps are somewhat “protective” against CIN 2/3, but not as “protective” against invasive cancer, screen every two years to be safe (even though the overall incidence of cancer is still really low) – Over age 30, if have had three normals, it is very safe to screen only every 3 years So, as long as there are no contraindications to “relaxed” screening (HIV, immunosuppression, h/o high grade dysplasia)… Age 21-29: pap every other year Age>30: pap every 3 years once has had 3 consecutive normals My (own personal) Strategies • Tell patients, ok so you’re an odd (or even) number year pap. (helps them to remember which years they need a pap) • Still recommend annual exams, especially for sexually active women – – – – – Contraceptive management Sexual and Vaginal health General health concerns Health habits (caffeine, alcohol, drugs, exercise, sleep) No internal exam unless symptomatic (can do urine for chlamydia screening) – Beth does usually do an internal exam and bimanual – Usually do external genital exam (practice, surprising number of surprises) • Make sure to obtain prior records and not rely on patient report of when last pap occurred or the actual result Reminders • For pap management guidelines, visit: – www.asccp.org – Click on: Consensus guidelines - cytologic abnormalities - download pdf Reminders • No endocervical cells – Just repeat in one year for most women – Repeat in 6 months for • Previous abnormal pap of >ASCUS without 3 subsequent negative paps, at least one of which had ECC • Previous pap with unexplained glandular abnormality • Positive HR HPV test within past 12 months • Clinician inability to clearly visualize and/or sample the cervix • Immunosuppression • Insufficient previous screening (not participating in at least every 2 year screening) Reminder • Cervicitis / Inflammation / partially obscured – Repeat in 12 months for most women – Repeat in 6 months for • Previous abnormal pap of >ASCUS without 3 subsequent negative paps, at least one of which had ECC • Previous pap with unexplained glandular abnormality • Positive HR HPV test within past 12 months • Clinician inability to clearly visualize and/or sample the cervix • Immunosuppression • Insufficient previous screening (not participating in at least every 2 year screening) • Similar obscuring factor in consecutive pap tests Reminder • Unsatisfactory pap – It’s like not having done the pap at all! – Repeat within 2-4 months WHO Medical Eligibility Criteria Provides guidance regarding whether women with certain medical conditions, characteristics or exposures can safely use specific contraceptive methods Contains over 1800 individual recommendations addressing 18 contraceptive methods and over 160 medical conditions and subconditions http://www.who.int/reproductivehealth/publications/mec/ MEC full guidelines and MEC wheel from WHO Recommendations Category 1: No Restrictions Category 2: Generally Use (Benefits usually outweigh risk) Category 3: Usually Not Recommended (clinical judgment and continuing access to clinical services are required for use) Category 4: Absolute Contraindication US Medical Eligibility Criteria for Contraceptive Use, 2010 Published May 2010 First time CDC has issued national guidance on contraceptive practice Systematic reviews of the scientific evidence for each of the WHO recommendations considered for adaptation and each of the medical conditions considered for addition The vast majority of the US guidance is the same as the WHO guidance. Modification were made to WHO recommendations for six conditions and recommendations were developed for six new medical conditions http://www.cdc.gov/reproductivehealth/unintendedpregnancy/USMEC.htm New Medical Conditions in CDC MEC History of bariatric surgery Peripartum cardiomyopathy Rheumatoid arthritis Endometrial hyperplasia Inflammatory bowel disease Solid organ transplantation Adaptations to WHO recommendations Breastfeeding and hormonal contraception Postpartum IUD insertion Valvular heart disease and IUDs DVT/PE and hormonal contraception Ovarian cancer and IUDs College Concerns Obesity Hypertension Inflammatory Bowel VTE Smokers Headache Drug interactions Drug Interactions Anticonvulsantsphenytoin barbituates primidone topiramate oxycarbazepine carbmazepine Lamotrigine Category 3 for CHC and POP Category 2 for Implanon May decrease contraceptive efficacy Category 1 all other methods Category 3 CHC CHC use may decrease effect of lamotrigine when used as monotherapy Category 1 all other methods Rifampicin or rifabutin Category 3 CHC and POP Category 2 Implanon Contraceptive efficacy may be reduced Antiretroviral Therapies Many interactions- look them up Broad Spectrum Antibiotics Antifungals Antiparasitics All Category 1 for all methods Don’t forget- St John’s Wort ! Any contraceptive failure while using antibiotics is more likely related to… GI upset associated with antibiotics Missing pills due to increased medication taking demands Confusion regarding effectiveness Headaches Recommendations are based on accurate diagnosis of type of headache Non-Migrainous Headaches Approximately 90% of all headaches are not migraines (eg, tension or muscle-contraction headache) Category 1 for all methods Category 2 for combined hormonal contraception ( CHC) if woman develops non-migrainous headaches while using Migraine without aura, age <35 Category 2 for initiation of CHC Category 3 if develops migraines while using CHC Migraine without aura, age >=35 Category 3 for initiation of CHC Category 4 if develops migraines while using CHC All other contraceptive methods are category 2 or 3 Migraine with aura, any age Migraine with aura, characterized by focal neurological deficits before and during the attack, affects 30% of migraine sufferers Category 4 for initiation or continuation of CHC Category 2 for initiation of all other methods (except paraguard) Category 3 if develops migraine while using other methods Why ? Pooled RR of ischemic stroke: Migraine Migraine Migraine Migraine (any) women <45 = 2.16 with aura = 2.27 without aura = 1.83 (any) and COC use = 8.72 BMJ,doi:10.1136 Dec 2004 WHO studies found a statistically significant increase in the risk of ischemic stoke, but not hemorrhagic stroke, among CHC users who experienced migraine with aura (OR 3.0 95% CI 1.3-11.3) A nonsignificant increase was found in CHC users who reported migraine without aura (OR 3.9 95% CI 0.7-14.8) We offer women their choice of all progestin-only methods and IUD Hypertension For all categories of hypertension, recommendations are based on the assumption that no other risk factors exist for cardiovascular disease (ie. smoking, hyperlipidemia, diabetes) Adequately controlled hypertension Category 3 for CHC Category 1 or 2 for all other methods * COC ( 30EE, 150 lvg) increases SBP 8 mm Hg, DBP 6 mmHg on average Elevated blood pressure levels (properly taken measurements) 140-159/ 90-99 Category 3 CHC >= 160/ >= 100 Category 4 CHC Category 3 DMPA All other methods are category 1 or 2 Why ? RR of hemorrhagic stroke is 1.2 for nonsmoking CHC users, 1.8 for those with mild or controlled hypertension and 25.7 for users with severe hypertension WHO Collaborative study of Cardiovascular Disease and Steroid Hormonal Contraceptive Lancet 1996 Smokers Age <35 category 2 CHC category 1 all other methods Age >=35, < 15 cigs/day category 3 CHC category 1 all other methods Age >= 35, >= 15 cigs/day category 4 CHC category 1 all other methods Cardiovascular mortality attributable risk to coc use: In young nonsmokers= 1/370,000 In young smokers= 1/100,000 In older smokers = 10/100,000 Inflammatory Bowel Disease Ulcerative colitis, Crohn’s disease Category 2/3 for CHC Category 2 - Women with mild IBD and no other risk factor for VTE Category 3- Women at increase risk for VTE (those with extensive disease, steroid use, vitamin deficiencies, fluid depletion Category 2 -for POP and DMPA Category 1- IUDs and Implanon Absorption of coc’s among women with mild UC was similar to absorption among healthy women. May not apply to women with Crohn’s or extensive bowel resections Venous Thromboembolism Risk factors Obesity Previous venous compromise Immobilization Factor V Leiden Defect (30% of all VTE) CHC Use RatesYoung women 4-5/100,000 Pregnant women 123/100,000 Postpartum 320/100,000 Low dose CHC use 20-60/100,000 History of DVT/PE Higher risk of recurrence (1 or more risk factors) Category 4 History of estrogen-associated DVT/PE Pregnancy associated DVT/PE Idiopathic DVT/PE Known thrombophilia, including antiphospholipid syndrome Active cancer History of recurrent DVT/PE Low risk for recurrence (no risk factors) Category 3 Weight Concerns Gaining weight on method Method Efficacy due to higher body weight VTE risk due to higher body weight CDC MEC: BMI >= 30 category 2 for CHC category 2 for DMPA use when <18 yo and BMI >30 obese teens more likely to gain weight with DMPA Category 1 all other methods • 3 lb average gain - all CHC • 5 lb cumulatively with DMPA • Decrease effectiveness patch > 90 Kg (though still better than condoms) • No decrease effectiveness with Nuva Ring, IUD • Implanon- Not studied in greater than 130 % IBW (BMI>30) • Decreased effectiveness with CHC ? Body mass index, weight, and oral contraceptive failure risk. Holt VL; Scholes D; Wicklund KG; Cushing-Haugen KL; Daling JR Obstet Gynecol 2005 Jan;105(1):46-52. N= 248 Risk of pregnancy was nearly 60% higher in BMI >27.3 = OR 1.58 “Suggest that being overweight may increase the risk of becoming pregnant while using OCs. If causal, this association translates to an additional 2-4 pregnancies per 100 woman-years of use among overweight women, for whom consideration of additional or effective alternative contraceptive methods may be warranted.” Follow-up study… substantiated overall higher failure rates, did not claim any dosedependent relationship The Role of Body Weight in Oral Contraceptive Failure: Results from the 1995 National Survey of Family Growth . Annals of Epidemiology , Volume 15 , Issue 7 , Pages 492 - 499 L . Brunner , C . Hogue Women with a BMI ≥ 30 had a statistically significant increased risk of having an OC failure as compared to women with BMIs of 20 to 24.9 (OR = 1.80, 95% CI, 1.01- 3.20). However, after adjustment for age, marital status, education, poverty, race/ethnicity, parity, and dual method use, this increased risk was attenuated and no longer statistically significant (OR = 1.51, 95% CI, 0.81- 2.82). Increasing body weight was not associated with an increased risk of OC failure in the unadjusted or adjusted models. Retrospective study adjusted for confounding factors= no increased risk. Body weight and risk of oral contraceptive failure. Holt VL; Cushing-Haugen KL; Daling JR Obstet Gynecol 2002 May;99(5 Pt 1):820-7. N= 755 retrospective questionnaire. Women greater than 70.5 kg = RR 1.6 Obese Very low dose OC users = RR 4.5 “Suggest that body habitus may affect metabolism sufficiently to compromise contraceptive effectiveness. Consideration of a woman's weight may be an important element of OC prescription.” Failures were highest in women >154# who use lower dose formulas Contraceptive Technology 2007 recommends against routinely prescribing high-dose COC to obese women due to VTE risk. It may be better to decrease or eliminate the pill free interval for heavier women ACOG : Advises caution in the use of estrogen-containing methods in obese women (BMI>30) who are over age 35 due to VTE risk Women weighing more than 176 # may have an increased risk of unintended pregnancy when using low- dose COC Practice Bulletin 351:November 2006 Heavier women have higher rates of VTE, the potential for decreased efficacy with lower dose COC’s and higher risk for pregnancy related complications….. With few exceptions, intrauterine devices offer the safest, most effective method for many women- especially those with coexisting medical conditions But … what about… Risk of PID ? The risk of PID postinsertion (9.7/1000) fell to background levels (1.4/1000) 20 days after insertion and remained at that level at 8 year follow-up (Cochrane Database Syst Rev 200;(2). The irritative, mucous plugging effect of the IUD string may provide enhanced protection from PID when exposed to STIs CDC MEC= Category 4 for IUD placement with existing GC or CT Category 2 if GC/CT acquired with IUD in place Nulliparity ? Once STIs were established as the causal agents for PID, the restriction against use of IUC for nulliparous women had no basis in evidence. In 2005 Paraguard removed “having had at least one child” from their labeling for recommended patient profile. CDC MEC= Category 2 for nulliparity History of Ectopic Pregnancy ? The IUD significantly reduces a woman’s risk of an ectopic pregnancy, compared with ectopic risk with no contraception. Pregnancy that do occur with an IUD in place (.14/100 women) are more likely to be ectopic CDC MEC= Category 1 for past history of ectopic pregnancy A 19 yo sophomore with a history of severe dysmenorrhea and iron deficiency anemia. She gets ”bad headaches” that make her nauseous and photophobic- usually with her periods. She denies any “warning sign” of her headaches or symptoms such as visual changes or facial numbness. She is requesting contraception. What are her contraceptive options ? 18 year old Junior who had both Chlamydia and an ectopic pregnancy last year. She is sexually active now and is frequently forgetting her pills. Her partner will not use condoms. What are her contraceptive options ? A 24 yo grad student wants to start contraception. Her mother had breast cancer. She smokes about 10 cigarettes a day and has irritable bowel syndrome What are her contraceptive choices ? 34 year old G0P0 graduate student. She has a BMI of 32 and has a blood pressure on 3 separate readings of 145/92. She developed migraines without aura while using a COC 10 years ago. She is taking Dilantin for a recently diagnosed seizure disorder and was told by her home healthcare provider to “get on birth control” because she shouldn’t get pregnant while taking this medication. What are her contraceptive options ? STI Update CDC has not yet published the 2010 Guidelines, so here’s a taste of what might be new… Expedited Partner Therapy • Expedited Partner Therapy (EPT) is the clinical practice of treating the sex partners of patients diagnosed with chlamydia or gonorrhea by providing prescriptions or medications to the patient to take to his/her partner without the health care provider first examining the partner. Why would we do this? • Between 12 and 26% of young women diagnosed with chlamydia will be re-infected within 12 months • Risk factors are young age (<25) and untreated partners – Risk for recurrence was due to resumption of sexual activity, not due to new partners or other sexual behavior risks (Whittington 2001) • Studies have shown EPT to be safe and effective Trelle, BMJ 2007, Improved effectiveness of partner notification for patients with sexually transmitted infections: Sytematic review. EPT is supported by CDC, AMA, AAP, and the Society of Adolescent Medicine http://www.jahonline.org/article/S1054-139X(09)00205-5/fulltext Legal Status of Expedited Partner Therapy How do you do it? • Incident patient must have confirmed chlamydia or gonorrhea • Prescription/Medication: – Give prescription for the partner to the patient – Double the amount on the script for the patient – Consider calling partner yourself and calling in a prescription after discussing it with them • Education, education, education – – – – Drug allergy & Drug interactions If symptomatic, needs evaluation Synchronicity of treatment and abstinence Need for any other partners to also be treated • www.cdc.gov/std/ept • Consider internet partner notification – www.inspot.org Anticipated Changes in 2010 Guidelines • Male circumcision for STI prevention • Rescreen for CT, GC, and trich after treatment in 3 months (remember, never sooner than 3 weeks if NAAT!) • HPV vaccine for men and women • Gonorrhea – No more fluoroquinolones – Use 250 mg Ceftriaxone dose instead of 125 Anticipated Changes in 2010 Guidelines • More info on vaginitis, such as recurrent and refractory BV and yeast • Also added tinidazole as treatment for BV, 2 gm BID x 2 days • Trichomonas – New tx – tinidazole – New Aptima NAAT test • Info on mycoplasma genitalium A final word… • Remember, if a patient presents with urethritis, cervicitis, PID, or proctitis that is likely an STI… –TREAT EMPIRICALLY – Do NOT wait for test results to guide treatment • Also, remember to retest in 3 months for confirmed gonorrhea, chlamydia, and trich Emergency Contraception Introducing…. ella! ella Emergency Contraceptive • Single 30 mg pill of uliprotsol, which is a progesterone agonist/antagonist (as opposed to Plan B, which is a progestin, so just a regular agonist), and it works by delaying/ inhibiting ovulation and possibly also by changing the endometrium so that implantation is hindered (this is no different than for Plan B). • It has no demonstrated decrease in effectiveness when taken between 48 and 120 hours after intercourse (as opposed to within 48 hrs), but effectiveness stays at about a 66% reduction in possibility of pregnancy. (this is slightly less than Plan B, which gives 75% reduction in the first 2-3 days, but less effectiveness thereafter), so would be a potentially better option at day 4 or 5 than Plan B. ella Emergency Contraceptive • Due to high affinity to the progesterone receptor and its antagonistic effects, it may interfere with effectiveness of regular hormonal contraception. Therefore, the woman MUST use a barrier method for the entire remainder of that menstrual cycle. • It is likely less effective in women with a BMI greater than 30. We do not have sufficient numbers to give us surety or estimates. This has not been well-studied for Plan B, so we do not know if the same problem applies, but it likely does based on preliminary data. • Like Plan B, it can cause nausea and vomiting (recommended to give repeat dose if woman vomits within 3 hours of taking it), and can cause a change or delay in the next period. ella Emergency Contraceptive • Plasma concentration will be decreased if the woman is also taking a med that induces hepatic enzymes, so, like other progesterone methods, including Plan B, it will be less effective if the woman is taking any of the following: – – – – – – – – – – barbiturates bosentan carbamazepine felbamate griseofulvin oxcarbazepine phenytoin rifampin St. John’s Wort topiramate ella Emergency Contraceptive • Ella can only be taken once within the same menstrual cycle – you cannot repeat it again, as we do not have safety or efficacy data on that. • So, overall, it’s medical utility above Plan B is not great, save perhaps for the woman at day 4 or 5, for whom you may get better efficacy than with Plan B. One kicker of course is that it is prescription-only, which may make women THINK that it is more effective, and also may be minimally cheaper for someone with insurance than buying OTC Plan B. • Will be important for women to realize that earlier EC is always better – just because you can take EC 4-5 days out doesn’t mean that you should! Thank you for your attention! QUESTIONS…