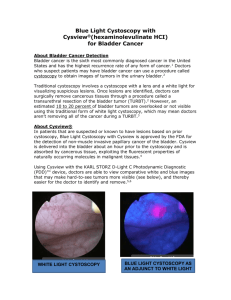
DIAGNOSIS OF BLADDER CANCER USING A POINT
advertisement

IMPROVED DETECTION AND SURVEILLANCE OF BLADDER CANCER USING A POINT-OFCARE NMP22 ASSAY Giora Katz MD, Raoul Salup MD, And the NMP22 Clinical Investigation Group Author Disclosure1 Matritech, Inc. : Honorarium 1 NMP22 Clinical Investigation Group Collaborating Investigators Yitzhak Berger MD, Associates in Urology, West Orange, NJ David Bock MD, Kansas City Urology Care, Kansas City, MO Jeffrey Brady MD, Winter Park Urology Associates, Orlando, FL M. Patrick Collini MD, Urology Associates of North Texas, Fort Worth, TX Martin Dineen MD, Atlantic Urological Associates, Daytona Beach, FL H. Barton Grossman MD, M.D. Anderson Cancer Center, Houston, TX Vahan Kassabian MD, Georgia Urology, Atlanta, GA Giora Katz MD, Lake City VAMC, Lake City, FL Shiva Maralani MD, Michigan Urology, St. Clair Shores, MI Edward Messing MD, University of Rochester Medical Center, Rochester, NY Raoul Salup MD, James A. Haley VAMC, Tampa, FL Mark Soloway MD, University of Miami School of Medicine, Miami, FL Barry Stein MD, Rhode Island Hospital, Providence, RI Alan Treiman MD, Urology Treatment Center, Sarasota, FL Kevin Tomera MD, Alaska Clinical Research Center, Anchorage, AK 2 Introduction • Early diagnosis of bladder cancer saves lives • Cystoscopy is the “Gold Standard” in evaluation of the urinary bladder for presence of cancer • AUA guidelines recommend combination of cystoscopy and adjunct tests in evaluation of urinary bladder for the presence of cancer in high risk patients. 3 Nuclear Matrix Proteins and Transitional Cells of the Urinary Tract • Nuclear matrix proteins (NMP) make up the structural framework of the nucleus and coordinate its functions. • NMP22 is specific for transitional cells in the urinary tract. • Upon cell death NMP22 is released into the urine. • Malignant transitional cells contain up to 80 times higher concentration of NMP22 levels than normal cells. • Urine level of NMP22 > 10 U / ml is associated with a high probability of TCC. • Unlike cytological examination, detection of NMP22 protein is not dependent on recovery of intact cells. 4 NMP22 BladderChek Point-of-Care Device Created to identify urinary NMP22 levels > 10 U/ml. – Can be performed by non-physician staff members (CLIA exempt). – Requires 4 drops of freshly voided urine. – Results available in 30 minutes. – Built-in quality control. 5 Positive Negative Control Test 6 OBJECTIVE We investigated whether a point-of-care assay (NMP22® BladderChek® Test, Matritech, Inc., Newton, MA) can enhance detection of bladder cancer in patients undergoing cystoscopy for either initial evaluation or surveillance of TCCB. 7 Study Design • Two prospective studies: 23 facilities in 10 states; academic, private practice and VA – 1,331 patients scheduled for cystoscopy due to increased risk of bladder cancer (hematuria (92%), history of smoking, irritative voiding symptoms), – 668 patients with a history of bladder cancer under surveillance for recurrence • Voided urine sample obtained for analysis of NMP22 marker (30 min, CLIA waived) and cytology prior to diagnostic cystoscopy • Urologists were blinded to NMP22 and cytology results while performing and reporting the result of cystoscopy • Further workup was based on clinical findings and results of cystoscopy and cytology • TCC was diagnosed based on pathology 8 Results: Evaluation of High Risk Patients Suspected of Having Bladder Cancer • Among 1,331 high risk patients screened for bladder cancer, 79 (6%) had pathologically confirmed transitional cell cancer. • Initial cystoscopy alone detected 86% (68/79) of the cancers. • Combination of cystoscopy and NMP22 test (either or both are positive), detected significantly more cancers, 94% (74/79), p = 0.014. 94 % 92 Cysto alone 90 88 Cysto and NMP22 86 84 82 New investigation 9 Surveillance Patients with History of TCCB for Recurrence of Bladder cancer • Among the 668 patients undergoing surveillance, 100 % 103 (15%) had 98 pathologically confirmed recurrences. 96 Cysto • Initial cystoscopy alone 94 alone detected 91% (94/103) of 92 the malignancies. Cysto 90 and • Combination of cystoscopy NMP22 with the NMP22 test (either 88 or both are positive) 86 identified 99% (102/103) of TCCB surveillance the cancers , significantly more than cystoscopy alone, p = 0.005. 10 Patients At Risk Improved Diagnosis of Aggressive Cancer with Combination of Cystoscopy and NMP22 BladderChek Test Muscle Invasive High Grade Cystoscopy alone 55% (6/11) 81% (22/27) Cystoscopy & NMP22 Test 91% (10/11) 93% (25/27) p=0.046 Cancers not seen by cystoscopy but detected by NMP22 Test: Bladder CIS, T2, T3; Ureter T2; Renal Pelvis T1, T3 11 Surveillance Improved Diagnosis of Aggressive Cancer with Combination of Cystoscopy and NMP22 BladderChek Test Muscle Invasive High Grade Cystoscopy alone 64% (7/11) 75% (24/32) Cystoscopy & NMP22 Test 100% (11/11) 97% (31/32) p=0.046 Cancers not seen by cystoscopy but detected by NMP22 Test: TaG1, 2 CisG3, T1G3, 2 T2G3, 2 T4G3 12 Negative Predictive Value when both cystoscopy and NMP22 Test are negative (Reliability of a negative result, driven by false negative) Evaluation of patients at risk 99.5% (1072/1077) Surveillance for recurrence of TCC 99.8% (493/494) 13 CONCLUSIONS • Combined with cystoscopy, the NMP22 point-of-care test can significantly improve detection of bladder cancer both in patients at risk and under surveillance. • It can be performed by office staff, and delivers a clinically meaningful result during the patient visit. 14 Sensitivity for Detecting TCC: Diagnosis 100 90 80 70 60 50 40 30 20 10 0 Ta T1 Tis NMP22 Test = 57% T2 + Low Grade Md Grade High Grade Cytology = 16% 15 Sensitivity for Detecting Cancer: Monitoring 100 90 80 70 60 50 40 30 20 10 0 Ta T1 Tis NMP22 Test = 50% T2 + Low Grade Md Grade Cytology = 12% High Grade 16 Specificity in Initial Diagnosis No GU Disease No Cancer NMP22 Test 90% 86% (512/567) (1072/1249) 100 90 % Negative NMP 80 70 60 50 40 30 20 10 0 NED BPH Cystitis Calculi 17 Predictive Value: Surveillance NMP22 Test Cytology Cystoscopy PPV NPV 41% 91% (51/123) (493/545) 41% 86% (12/29) (535/621) 91% 98% (94/103) (556/565) Positive and negative predictive value are dependent upon the prevalence of disease in the tested population 18 Sensitivity for Detecting Cancer: Monitoring 100 90 80 70 60 50 40 30 20 10 0 Ta T1 Tis NMP22 Test = 50% T2 + Low Grade Md Grade Cytology = 12% High Grade 19