injury - GLLM Moodle 2
advertisement
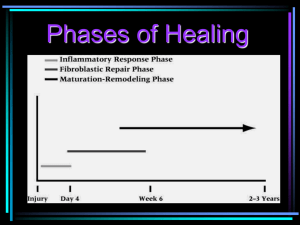
Sports injuries Objectives By the end of the session you should be able to: • List the physiological responses common to most sports injuries • Describe the physiological responses common to most sports injuries Video link Watch the video and identify 5 different types of sporting injury, listing what you think the injury is and write a sentence on how and why you think it occurred • Sports Injuries Primary and secondary damage • Primary damage: Is tissue destruction caused by an injury • Secondary damage: Occurs as cells at the injury site die due to hypoxia due to the damaged and blocked blood vessels at the site which are unable to deliver oxygen Physiological Responses Injury response cycle for any tissue • Primary and secondary damage 1. Inflammatory response 2. Blood Clotting 3. Fibroblastic repair 4. Maturation remodelling 1. Inflammatory response • Stage 1 / Swelling • This inflammatory response represents the body's attempt to dispose of blood (from torn tissue) and damaged cells before starting to repair the damage done. • This initial inflammatory phase lasts about 2 to 4 days and is followed by scar formation and repair. 1. Inflammatory response • This is the beginning of the healing process • Oedema helps to transport proteins and fibrinogen to the area • Chemicals then irritate neuroreceptors which reduces pain • The swelling restricts the movement of the body part preventing further injury • Leucocytes and Phagocytes are delivered to the injured area to dispose of the damaged cells 2. Blood clotting • Starts approximately 48 hours after injury • Increase in the formation of extra cellular matrix (collagen). • Tissue cells reproduce to form new blood vessels • Collagen is crossed linked but is generally haphazard with no real tensile strength. • This phase can last up to six weeks or more. 2. Blood clotting • Haemostasis: damaged blood cells are blocked with a clot which is then removed when tissue is repaired • Platelets activated by Thrombin converge on the injury site • Fibrinogen causes the platelets to bind with collagen that form a plug • Once repaired Plasmin dissolves the clot 3. Fibroblastic repair • Is the formation of scar tissue to repair injured tissue • Starts to rebuild the capillary network ensuring blood supply and nutrients to the damaged area • Collagen is randomly deposited at this stage to strengthen the wounded area Collagen • About one quarter of all of the protein in your body is collagen. • Skin damage often destroys the weave-like structure of collagen. • Evolutionary legacy means the body acts in haste. • The body creates a quick fix. • When skin cells grow on this, they produce the pale, less flexible material we know as scar tissue, rather than normal skin. 4. Remodelling • Initiated after approximately 14 days of injury. • Collagen fibres are realigned or remodelled along lines of mechanical force forming a scar. • Scar tissue reabsorbed – type III collagen is replaced by type I collagen to increase strength. • This phase can last up to a year. 4. Remodelling • The re-modelling phase is initiated after a few weeks but can take several months or even years to be completed. • Depending on the site and severity of the injury. The re-modelling process is helped considerably by rehabilitation exercises. • Correct diagnosis, treatment and rehabilitation is important at this stage. The healing process • In pairs decide how long (typically) it takes for these types of tissue to heal, decide why they take that long and think about the healing process Skin 2-3 weeks Muscle 4-6 weeks Tendon 6-8 weeks Ligament 6-8 weeks Bone 12-16 weeks Nerve 12-18 months Task • In your own words write down the four stages of healing Muscle healing • Your muscles, do not actually heal with muscle tissue, but with "foreign" substances including collagen. • The resulting scar tissue is weaker, less elastic, and highly prone to re-injury. • Once a muscle is damaged, it can become the source of a great deal of pain. Tendon and ligament healing • Follow a similar healing process to that of muscle injury healing. • Inflammation peaks after 4 days and continues until 10 days post injury. • Anti-inflammatory drugs can prevent adhesions but can also delay repair and result in weaker healed tendons Bone healing • If you fracture a bone, as long as it is set and fixed in place properly. • A healed bone can be stronger than it was before the fracture. • Bone tissue heals with calcium and other minerals. • Osteoblasts and Osteoclasts. Cartilage healing • Injuries which do not involve the underlying bone heal poorly, if at all. • No inflammation, bleeding, clots or granulation of collagen matrix occurs in purely cartilaginous injuries, because it doesn’t have a direct blood supply. • Some healing may occur if underlying bone is damaged. Key words • Hypoxia – starving of oxygen • Oedema – accumulation of fluid and swelling • Leukocytes – blood cells which devour damaged or bad cells • Haemostasis: is when damaged blood cells are blocked with a clot which is then removed when the tissue is repaired • Platelets – blood cells which produce clotting • Collagen – a protein that helps repair injured tissue • Fibrinogen - a protein used in repairing tissue • Plasmin – enzyme that degrades blood