2010 CBT Workshop
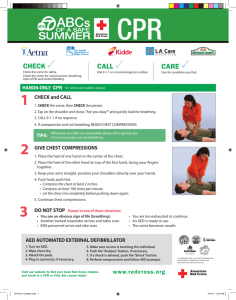
advertisement

ROC on Dr. Eisenberg Steve Perry Administrivia CPR Highlights Lowlights Application of skills Any Changes? ROCKING on or off? Rock is still alive and well Analyze early and late and ITD are done Oct 2009 1600 enrolled 94% cases correctly enrolled with AE/AL and ITD 89 % correctly enrolled with ITD Receiving downloads fast then ever following HOT CALLS Don’t Forget: EMS witnessed Every time compressions are started on a non traumatic patient Cardiac arrest after Medics arrive You’ve done such a good job****** More to come Mickey Eisenberg, MD Medical Director King County EMS Eisenberg’s Pet Peeves Review of cardiac arrest survival ROC trial summary CPR protocol changes DART trial summary New MIRF for 2010 Emphasis for 2010 Revision in Protocol Book (Blue Book) Pulse oximeter is not a pulse detector. The old fashioned way to feel a pulse is the ONLY way to feel a pulse A seizure may be the first sign of cardiac arrest. Do not use oxygen saturation to verify cardiac arrest Glucose level must be documented after therapy Remember IOS and MOI when using sick/not sick Survival from Witnessed VF NIH has stopped ROC-PRIMED and ITD because of similar survival in all arms of the study. NO harm identified Revision in King County CPR protocol in light of ROC Trial Assess ABCs. Assess ABCs. If not breathing, open airway and provide two ventilations. If no pulse, perform chest compression while attaching defibrillator. Give verbal report and count compressions. When defibrillator is attached complete 30 compressions, clear patient, analyze rhythm, and shock if indicated. Always provide 30 compressions prior to any rhythm analysis. Subsequent CPR intervals should begin and end with 30 chest compressions and each interval should be 2 minutes (or slightly longer depending when 30 compressions end). Exception: When the patient goes into VF while monitored or attached to an AED a defibrillatory shock may be administered immediately. Essentially a slightly modified analyze early Confirm need for CPR, open airway, look listen and feel, two ventilations, 30 chest compressions (during which AED is attached), analyze, shock, 30:2:30:2:30:2:30 (for approximately 2 minutes or slightly longer – start and end with 30 chest compressions), analyze, if no shock indicated check pulse, if shock indicated shock, 30:2 etc Dispatch Assisted Resuscitation Trial King County, Thurston County, London Comparing chest compression only versus chest compression and mouth-to-mouth No difference in survival between the two messages Chest compression delivered earlier with chest compression only Every patient to receive backer Must complete the electronic record Only exceptions are DOA patients, patients that leave the scene, or AMA patients Case will be left open until record is complete Please verify phone and address Not Transported Your condition did not require emergency vehicle transport at this time. Please understand that your situation may still require follow up medical attention. If your condition worsens, seek medical help or call 9-1-1. Transported You are being transported to a medical facility for further medical care. You may be billed for this service. Low Blood Sugar Your fire department measured your blood sugar during your medical emergency. Before treatment, your blood sugar level was _________________. Your low blood sugar was treated by the following method: □ No Treatment The EMTs gave no immediate treatment because_________________________ □ Oral Glucose _______ gm □ Other ____________________ After administration of glucose and/or prior to the departure of the EMS Team, your blood sugar level was ________________ . If you are choosing to stay at home: Eat a FULL MEAL NOW. Contact your doctor before you take your next insulin dose. If you are unable to contact your doctor, reduce your next insulin dose by 25%. Keep trying to contact your doctor. Check your blood sugar frequently for the next several hours. DO NOT: stay alone or drive/operate dangerous machinery for the next six (6) hours If your condition worsens or initial signs and symptoms return, CALL 911 IMMEDIATELY! High Blood Pressure Your fire department took your blood pressure during your medical emergency. Your blood pressure was very high. Blood Pressure Categories Systolic Diastolic 160 140 120 <120 Hypertension Stage 2 Hypertension Stage 1 Prehypertension Normal 100 90 80 <80 Your Reading High blood pressure can lead to life-threatening disease such as heart disease, stroke, or kidney failure. There are good treatments for lowering high blood pressure. You need to talk with a doctor. We recommend that you have your blood pressure checked again as soon as possible. Community Resources The Crisis Clinic offers support services available to everyone in King County. Their staff gives immediate, confidential assistance for people in need of help. Language interpretation is available. DIAL 2-1-1 (available Monday thru Friday from 8 am to 6 pm) Caregiver & Disability Resources Domestic Violence Emergency Shelter Financial Assistance for Rent or Utilities Food & Clothing Health Care & Support Groups Legal Help DIAL (206) 461-3222 • (866) 427-4747 (available 24 hours a day) Emotional Crisis & Trauma Suicide Prevention & Education www.crisisclinic.org Heart Attack Warning Signs Call 9-1-1 if you have: Chest Discomfort Uncomfortable pressure, squeezing, fullness, or pain in the center of the chest that lasts more than a few minutes, or goes away and comes back. Discomfort in Other Areas of the Upper Body May be felt in one or both arms, the back, neck, jaw, or stomach. Shortness of Breath Often occurs with or before chest discomfort. Other Signs May include breaking out in a cold sweat, nausea, or lightheadedness. Stroke Warning Signs Call 9-1-1 if you have: Sudden numbness or weakness of the face, arm or leg, especially on one side of the body Sudden confusion, trouble speaking or understanding Sudden trouble seeing in one or both eyes Sudden trouble walking, dizziness, loss of balance or coordination Sudden severe headache with no known cause Continued emphasis on 3 major conditions: CA (we can achieve 50% survival for VF) Code ACS (recognition, STEMI, determination of onset, aspirin, expedited scene time and transport to hospital by paramedics) Code CVA (recognition, determination of onset, expedited scene time and transport to hospital by EMTs Recognition and expedited care Provide aspirin Determine time of onset Emphasis on STEMI and early alerting of hospital Expedited transport to hospital by paramedics FAST exam Facial weakness Arm weakness Speech abnormality Time last seen normal Check glucose, should be >60 Determine if patient is taking coumadin (Warfarin) Time hospital alerted Expedited transport to hospital by EMTs Current version was issued in 2007 Suggestions for updates and changes are welcome AFTERCARE Not Transproted Transported Low Blood Sugar High Blood Pressure Community Resources Type code 234: 2190 patients coded as CVA/TIA. (2.3% of all EMS calls) 13% received ALS care at the scene 16% required intubation, 42% required IV line Transport 87% transported by BLS (60% by private ambulance) 7% ALS 3% not transported 2% POV Falls If you are 65 or older and fell at home, there are two programs in King County that can assist you in staying healthy, independent, and safe in your home. Please call for more information. One Step Ahead King County Emergency Medical Services (206) 369-5817 Individualized health evaluation in your home Free for those who qualify Home safety check Installation of home safety devices Harborview Fall Prevention Clinic (206) 744-4191 Individualized health evaluation at Harborview Home safety suggestions Medication review, balance and vision checks AFTERCARE Not Transported Transported Low Blood Sugar High Blood Pressure Falls Community Resources De-Fibrillation Coordinator Steve Perry King County EMS Training Division AED / Defib Program Up-date Quality Assurance Through June 2009 425 CPR Cases 57 of those cases were bystander-witnessed arrest due to CAD 28 had VF as initial rhythm 49% Where we are and what do we know?? Compressions Compressions Compressions The more time on the chest the better The more time on the chest the better!! Minimize time for analysis Minimize time from defibrillation –resuming chest compressions. Practice makes perfect practice. Audio Information is important. Stay focused. Review your own cases. Confirm cardiac arrest – turn on AED while performing CPR ID self, company, approx age of pt, witnessed or not, pad application, clearing to analyze. Proceed with 30:2 compression to ventilations in adults 15:2 x 2 in child SHOCK if indicated – immediately start 2 mins CPR If NO SHOCK - check pulse – immediately start 2 mins CPR Prior to January 2005 our resuscitation rate was < 36%.... We are currently > 48%...... We’re all in this together We have a problem…. No one wants to be that guy CC of Angina & RA SaO2 = 99%. When asked why no oxygen was applied, the comment was: “You can’t get higher than 100% so what’s the point?” Uncons/Unresp & snoring after being struck by a car and the most important thing was to get the patient’s tennis shoes off. OD with RA SaO2 of 96%, uncons, & snoring. (We were told “No O2 until SaO2 is <95%” Since when is checking cervical dialation within an EMT’s standard of care?? “His pulse is 70 bpm…According to the pulse ox..That’s what it says, is 70” CC of respiratory distress applied a NRB at 8 lpm because: ”That’s how we were taught” Mistake a hypoxic sz (VF) for an ill diabetic determined to get a blood glucose reading. Female with NO BP sitting on toilet awaiting a doppler from a second due medic unit (“white as rice paper”) Remember who we are here for and why. Check our egos at the door Bed side learning is optimal Chances are similar issues are occurring in other agencies so let’s help one another out! Patient EMT/ CBT Instructor Training / Education Establish Continuity ID Training Needs (We are here for you!) Improve Performance EMTAC – EMT Advisory Committee. Paramedic Instructor Group Non-punitive Constructive Informative Feedback loop Site visits The Fire Service 100 years of tradition unimpeded by progress Progress - one retirement at a time Competition Ownership Lead by example Instructors as ambassadors Care and Feeding State County 301 Soft Tissue 435 Abdominal Discomfort 443 Altered LOC 537 Pediatric Emergencies 165 Sick vs. Not Sick 938 Street Medicine Care for burns? Penetration to the box? Care for Tensions Pnuemothorax Treatment of contusions, abrasions, lacerations, avulsions and amputations Put the wet stuff on the red stuff. But what about the patients? Immediate Life Threats Hypoxia/Respiratory Insufficiency Trauma Hypotension Persistent dry cough Poor Skin Signs Decreased Mentation Hoarse Voice Patient was in a confined space Burns to Face, Nose, Mouth and Chest Singed Nasal Hair, Eyebrows and Hair Sooty Sputum Abnormal Breathing Inadequate chest expansion Thermal Electrical Chemical Nuclear Superficial Partial thickness Full Thickness Treatment of Pneumothorax Tension Pneumothorax Contusions Abrasions Lacerations Amputations – Pain usually interpreted as colic; a severe, intermittent cramping pain. Referred pain Perceived pain at a distant point of the body caused by irritation of the visceral peritoneum Perforation of an ulcer Gallstones that lead to inflammation (cholecystitis) Inflammation of the pancreas (pancreatitis) Inflammation or infection of appendix Inflammation of pouches in large intestine (diverticulitis) IHOP Causes of pain Menstrual cycle Pelvic inflammatory disease Ectopic pregnancy Always consider an ectopic with women having abdominal pain of child bearing years. Aneurysm Pneumonia Weakness in aorta May cause ileus and abdominal pain Hernia Protrusion through a hole in the body wall Determine whether patient can relax abdomen on command. Determine whether abdomen is tender when palpated. Palpate gently—rough palpation could cause further damage. Initial BP ,Pulse, Respirations, LOC Postural Vital Signs Findings 20 points Systolic drop in BP 20 point rate increase Contraindications Pressure of 90 or below Trauma 3rd Trimester bleeding Cardiac TIA’s Strokes Decreased LOC Why Why Why Brain attack Interruption of blood flow to the brain that results in the loss of brain function. Thrombosis — Clot that forms at the site Arterial rupture — Rupture of a cerebral artery Cerebral embolism — Obstruction of a cerebral artery caused by a clot that was formed elsewhere and traveled to the brain Left hemisphere Aphasia: Inability to speak or understand speech Receptive aphasia: Ability to speak, but unable to understand speech Expressive aphasia: Inability to speak correctly, but able to understand speech Right hemisphere Dysarthria: Able to understand, but hard to be understood Pipes –Pumps-Fluid Noxious Stimuli Response Why? Alcohol and it’s effects Cardiac Arrest OD’s Opiates Oxycodone Oxycotin Ecstasy Spinal Immobilization Pediatric Triangle Abuse Febrile Seizures Make a Decision! SICK NOT SICK Fluid Clinical Picture Evolving evolution Go with it Make a Decision! Chief Complaint/N.O.I. Respirations Pulse Mental Status Skin Signs/Color Body Position The Clinical Picture SICK DECIDE NOT SICK Unexplained bruises and welts seen after absences, weekends, or vacations. Unexplained burns, cigarette burns, especially burns found on palms, soles of feet, abdomen, buttocks; immersion burns producing "; "doughnut shaped" on buttocks or genital area. Rope burns. delay in treatment; burns in the shape of common household utensils or appliances Stories different from caregivers The majority of children with febrile seizures have rectal temperatures greater than 102 degrees F. Most febrile seizures occur during the first day of a child's fever Children rarely develop their first febrile seizure before the age of 6 months or after 3 years Online Course and Round Table Scene safety Yours Look but don’t touch everything Evidence preservation Documentation Documentation Written Camera Documentation Notes O2 sats are NOT pulse indicators Seizures may be your first sign of a cardiac arrest A B C’s Glucose MUST be documented after treatment REMEMBER IOS and MOI when using sick not sick Life begins and ends with Compressions Time is Muscle or Brain and in some areas these people don’t have grey cells to lose