File
advertisement

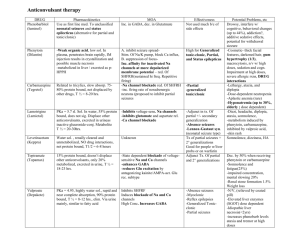
Neurological Diseases Epilepsy Parkinsonism Epilepsy Seizures that occur on a chronic, recurrent basis Thought to be caused by damage to the network of cortical neurons that have become capable of sustaining an excessive discharge pattern for several seconds The results of this excessive discharge pattern is a seizure Question If the damage to the cortical neurons is permanent, why don’t seizures occur all the time? Answer There is an interplay between environmental and internal brain factors The normal neuronal control mechanisms that contain and control abnormal neuronal firing are overcome Sometimes fatigue and sleep loss can trigger a seizure Normally impossible to determine what sets off seizures in most patients with epilepsy Non-Epilepsy Seizures Isolated seizures caused by a number of potentially reversible problems CNS trauma, infection, or stroke Blunt force trauma to the brain, concussions, damage to parts of brain, patients who had strokes Hyponatremia and hypoglycemia Hypoxia Alcohol withdrawal Fever (mainly in children) If underlying causes of seizures are not corrected, may lead to the development of recurrent seizures or epilepsy Etiology The cause of 80% of the seizures in patients with epilepsy are unknown The most common causes of epilepsy include head trauma and stroke CNS tumors and infections are also common causes Epidemiology 2 million in US are afflicted Incidence is between 35-75 cases/100,000 persons About 8% of population will experience a seizure during their lifetime New onset seizures occurs most frequently in infants <1 month of age and in adults >55 years old More chances in very young and very old Classification of Seizures Partial seizures Simple partial seizures Complex partial seizures Secondary generalized Generalized seizures Simple Partial Seizures Caused by a group of hyperactive neurons confined to a single locus in brain Patient experiences abnormal sensations or uncontrolled muscle movements in a portion of their body Patient does not lose consciousness Complex Partial Seizures Also caused by a group of hyperactive neurons confined to a single locus in brain Patient may experience sensory hallucinations and mental distortions Abnormal muscle movements may include chewing movements and loss of bowel or urine control Patient may lose consciousness Secondary Generalized Generalized seizures that begin as simple or complex partial seizure and spread to involve the entire brain Many patients complain of a “aura” Aura may be the beginning of the seizure Generalized Seizures Entire cortex is involved from the onset of the seizure Tonic-clonic seizures Absence seizures Myoclonic seizures Atonic seizures Tonic-Clonic Seizures Sudden loss of consciousness accompanied by tonic extension and rhythmic clonic contractions of all major muscle groups. The duration of the seizure is usually 1 to 3 minutes. This type of seizures are often called grand mal Absence Seizures Sudden and brief loss of consciousness without muscle movements. These seizures are often described as daydreaming or blanking out episodes Seizures often called petit mal Myoclonic Seizures Single and very brief jerks of all major muscle groups lasting 3-4 seconds Patients with these may not lose consciousness Patients describe seizures as shoulder shrugs or spinal chills. May cluster and build into a generalized tonic-clonic seizures. Atonic Seizures The patient loses consciousness and muscle tone. No muscle movements are typically noted Patient falls if not sitting or lying down Often described as “falling out” Overview of Treatment Selecting appropriate therapy is dependent upon identifying and understanding the different seizure types Selecting appropriate therapy is dependent mechanism of action, effectiveness, adverse effects, and potential for drug interactions Doses must be individualized using titration to minimize adverse effects and maximize therapeutic benefits Selecting appropriate therapy is based upon some knowledge, experience, luck and “black magic” In many cases, no logical approach “black magic?” – wagner calls it this because in some cases there is no logical approach to tx or seizures Mechanisms of Action Glutamate is the major excitatory neurotransmitter in the cerebral cortex Glutamate is released from presynaptic neurons and attaches to cetain receptor sites on postsynaptic neurons. This results in a opening of membrane channels allowing calcium or sodium to flow into the postsynaptic neurons thus depolarizing it and transmitting an excitatory signal Phenytoin, carbamazepine, and lamotrigine interfere with this mechanism (interfere w/stimulatory mech) Mechanisms of Action GABA is the major inhibitory neurotransmitter in the cerebral cortex GABA attaches to neuronal membranes and opens chloride channels When chloride flows into the neuron, it becomes less excitable. Mechanism causes seizure activity to be “shut off” by controlling excessive neuronal firing. Benzodiazepines work by enhancing action of GABA Approach to Treatment Type of seizures must be determined Determine if there is an underlying cause Risk of subsequent should be determined If it is determined that the patient has “real” seizures and if there is a risk of subsequent seizures, drugs are given Approach to Treatment In the design of pharmacological plan, the patient Must be willing to take the medication Must be willing to monitor seizure frequency Most be willing to monitor adverse reactions Selection of Treatment Proper identification of seizure type is helpful in selecting appropriate therapy Adverse reaction patterns and economic factors should be considered Follow consensus recommendations for treatment by American Academy of Neurology Effectiveness of Treatment 50% of patients with epilepsy can be completely controlled Of the remaining 50% 25% have meaningful improvement with treatment 25% of patients do not respond well Generic Name Brand Name Dose related Side Effects Idiosyncratic Side Effects Divalproex sodium Depakote Drowsiness, nausea, tremor Hepatotoxicity Lamotrigine Lamaictal Drowsiness, headache Rash Levetiracetam Keppra Drowsiness, dizziness Depression Phenytoin Dilantin Drowsiness, diplopia, ataxia Rash, others Topiramate Topamax Drowsiness, ataxia, dizziness acute myopia and glaucoma Carbamazepine Tegretol Drowsiness, nausea, diplopia Aplastic anemia Oxycarbazepine Trileptal Drowsiness, diplopia Hyponatremia Gabapentin Neurontin Drowsiness Edema Pregabalin Lyrica Drowsiness, ataxia, diplopia Edema General Consultation Take medication with a glass of water. Follow the directions on the prescription label. Take your doses at regular intervals about the same time every day Do not take your medicine more often than directed. If you miss a dose, take it as soon as you can. If it is almost time for your next dose, take only that dose. Do not take double or extra doses. Visit your doctor or health care professional for a regular check on your progress. Do not change brands or dosage forms of this medicine without discussing the change with your doctor If you are taking this medicine for epilepsy do not stop taking it suddenly Consultation You should keep a record at home of how you feel and how your condition is responding to treatment You should share this information with your doctor or health care professional at each visit. You should contact your doctor or health care professional if your seizures get worse or if you have any new types of seizures Many Problems Many, many adverse effects Adverse frequently cause drug to be discontinued Dose related Idiosyncratic Many drug interactions Generic Name Brand Name Dose related Side Effects Idiosyncratic Side Effects Divalproex sodium Depakote Drowsiness, nausea, tremor Hepatotoxicity Lamotrigine Lamictal Drowsiness, headache Rash Levetiracetam Keppra Drowsiness, dizziness Depression Phenytoin Dilantin Drowsiness, diplopia, ataxia Rash, others Topiramate Topamax Drowsiness, ataxia, dizziness acute myopia and glaucoma Carbamazepine Tegretol Drowsiness, nausea, diplopia Aplastic anemia Oxcarbazepine Trileptal Drowsiness, diplopia Hyponatremia Gabapentin Neurontin Drowsiness Edema Pregabalin Lyrica Drowsiness, ataxia, diplopia Edema Idiosyncratic Side Effects Rash including Stevens-Johnson Syndrome Hepatotoxicity Bone marrow toxicity These side effects are potentially lifethreatening Drugs Associated with most Idiosyncratic Reactions Carbamezepine Phenytoin Valproate Lamotrigine Parkinson’s Disease (PD) Overview Patients display motor and non-motor symptoms The most useful diagnostic tool is the clinical history Therapy is begun when the disease affects quality of life Disease is progressive Late stages of the disease may be associated with dementia Epidemiology Affects 1 million Americans Average age of onset is >60 years old Genetics may play a role in that 15% of patients with PD have a first-degree relative with the disease Etiology Cause is unknown Deterioration and eventual death of nerve cells in the substantia nigra Neurotransmitters needed for normal fx are reduced Motor Symptoms – “TRAP” T = Tremor at rest ("pill rolling") R = Rigidity A = Akinesia or bradykinesia P = Postural instability and gate abnormalities Non-Motor Symptoms – “SOAP” S = Sleep disturbances insomnia, rapid eye movement sleep behavioral disorder, restless legs syndrome 0 = Other miscellaneous symptoms nausea fatigue, speech, pain, dysesthesias, vision, seborrhea A = Autonomic symptoms drooling, constipation, sexual dysfunction, urinary problems, sweating, orthostatic hypotension, dysphagia P = Psychological symptoms anxiety, psychosis, cognitive impairment, depression Psychological impairment Cognitive impairment, depression, dimensia Response Fluctuations - MAD M= Motor fluctuations A = Akathisia D = Dyskinesias Approach to Treatment Three phases Lifestyle changes, nutrition, exercise Pharmacological treatment with drugs that enhance dopamine concentrations Helps in early stages Want to decrease progression of disease, but majority of the time it’s not possible Surgical treatment take pt, do NOT anesthetize open up patient’s skull(do use SOME anesthetic) expose the brain(brain has no pain receptors) Take electrodes and put on parts of brain that theoretically is controlling abnormal movements Apply electrical stimulation to those areas, if you hit electrical impulses, everything stops Classification of Drugs 2 types of drugs for tx: 1. 2. Drugs which increase dopamine concentration or activity Drugs which block acetylcholine 1. Theoretically better, but in reality are A LOT less effective, used as an adjunct (NOT as primary tx) Levodopa DOPA is metabolic precursor to dopamine Restores dopamine levels in substantia nigra Levodopa must be converted to dopamine in dopamanergic neurons As disease progresses(more dopramanergic neurons are destroyed in brain) response to L-Dopa declines less dopamanergic neurons are present to convert DOPA to dopamine Results of Treatment with LDOPA Must use high doses Causes significant nausea and vomiting Causes significant orthostatic hypotension (especially in elderly)– most of time elderly has it) With chronic treatment, patients often complain that drug effects wears off resulting in development of motor fluctuation Relief provided by levodopa is only symptomatic and temporary Does not halt progression of disease Carbidopa Carbidopa is a dopa decarboxylase inhibitor Used in combination with levodopa (Sinemet combo of L-dopa and carbidopa) Decreases metabolism of levodopa in GI tract and peripheral tissues Can use a lot less L-dopa Increases available of levodopa in CNS May decrease dose of levodopa five-fold and thus decrease incidence of side effects Consultation Take orally with water at least 30 minutes before eating or 1 hour after meals to maximize absorption May be taken with a small non-protein snack, such as fruit or a cracker, to avoid nausea. Administering with food may decrease absorption. ***Causes orthostatic hypotension **Do not stand or sit up quickly, especially if you are an older patient. This reduces the risk of dizzy or fainting spells Good advice for any pt that causes orthostatic hypotension Consultation Visit your doctor or health care professional for regular checks on your progress. It may be several months before you feel the full benefits of this medicine. Continue to take your medicine on a regular schedule You may experience a wearing of effect of this medication You may also experience an on-off effect where the medicine apparently stops working Tell your doctor or health care professional if any of these symptoms happen to you. Your dose may need to be changed. Psychiatric disturbances Psychiatric disturbances can occur including agitation, anxiety, confusion, dizziness, headache, euphoria, insomnia, memory loss, nightmares, toxic delirium, hallucinations, paranoid delusion, psychosis, and hypomania and depression Sinemet’s psychiatric effects tend to be progressive and frequently a compromise must be reached between psychiatric effects and control of parkinson symptoms. Dopamine Agonists Pramipexole Mirapex Ropinirole Requip Directly stimulate dopamine receptor sites in brain Actions similar to levodopa Severe side effects limit usefulness Consultation Take this medicine with a glass of water. Take it with or without food but if it upsets your stomach, take it with food. Do not stop taking this medicine except on your doctor's advice. Do not stand or sit up quickly, especially if you are an older patient. This reduces the risk of dizzy or fainting spells. (orthostatic hypotension) Antimuscarinic Drugs Much less effective that other drugs Used as an adjunct to levodopa/carbidopa Adverse effects similar to high doses of atropine Benztropine Cogentin (on top 200) Consultation May be administered without regard to meals Your mouth may get dry. Chewing sugarless gum or sucking hard candy, and drinking plenty of water may help This medicine may cause dry eyes and blurred vision. If you wear contact lenses you may feel some discomfort. Lubricating drops may help. You may sweat less than usual while you are taking this medicine. As a result your body temperature could rise to a dangerous level. Be careful not to get overheated during exercise or in hot weather. You could get heat stroke. Avoid taking hot baths and using hot tubs and saunas.