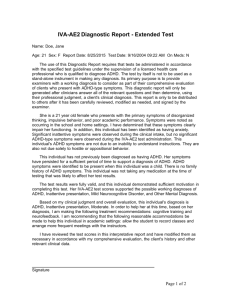
Screening & Diagnosis of ADHD
advertisement

Children and Adolescent ADHD www.pspbc.ca Child & Adolescent Attention Deficit Hyper Activity Disorder (ADHD) dreamstimefree_1471290 2 Fast Facts: Child & Adolescent ADHD Receives much media attention and controversy Neuro-developmental psychiatric disorder Impairs social, academic, family, and occupational functioning In Canada: 5 – 10 % in youth; 3 – 5 % in adults Associated with serious mental disorders: › Learning Disability › Conduct Disorder › Oppositional Defiant Disorder › Anxiety Disorders › Major Depressive Disorder › Disruptive Mood Dysregulation Disorder › Intermittent Explosive Disorder 3 Fast Facts: Child & Adolescent ADHD Greater risk for: › Poorer academic achievement › Fewer friends › Lower self-esteem › Teen pregnancies › Substance misuse/abuse › Interpersonal difficulties More prone to: › Physical injury › Accidental poisoning › Traffic accidents www.freedigitalphotos.net Upsidedown Vehicle by Bill Longshaw 4 Fast Facts: Child & Adolescent ADHD More likely to: › Score lower on achievement tests › Repeat grades › Suffer suspensions › Have problems with school Early treatment & effective therapies can help: › Medications › Psycho-education, and/or › Behavioral Intervention 5 Typical School Report Card Notes Stan [Kutcher] is disruptive in class, he is always talking and has great difficulty sitting still Stanley cannot settle down to do desk work – he is always fidgeting Stanley is not getting his homework done, he forgets to take his work home or to bring his homework to school Stanley’s grades do not reflect what he is capable of doing Stanley is so disorganized that he will never be successful at anything 6 ADHD Screening Question 3. Overall, do you have problems concentrating, keeping your mind on things or do you forget things easily (to the point of others noticing and commenting)? › If YES – consider ADHD › Apply the SNAP-IV 18 item scale › Proceed to the Identification, Diagnosis and Treatment of the Child and Adolescent ADHD Module 7 www.freedigitalphotos.net Schoolboy Does Exam Papers ADHD Screening Tool – Parent Version Does your teenager usually not finish things that he or she starts? Is your teenager not able to pay attention to things for as long as other teenagers? Does your teenager fidget or move around much of the time, even when he/she knows she should not? Is your teenager impulsive or does he/she act without thinking much of the time? Is your teenager’s behaviour causing him/her problems at home and at school? Have these difficulties been there for a long time (six months or longer)? www.freedigitalphotos.net Family by Master isolated images 8 8 ADHD Screening Tool – Youth Version Are you able to finish most things that you start within the time others expect? Do you have trouble paying attention to things that are not that interesting to you? Do you fidget or feel you have to move around much of the time? Do you often do things without thinking? Are you having problems at home or school related to your behaviour or because of trouble paying attention? Have these difficulties been there for a long time (six months or longer)? www.freedigitalphotos.net Question Or Doubt by Jeroen van Oostrom 9 9 Key Steps for Treatment of ADHD to Children & Adolescents 1. 2. 3. 4. 5. 6. Identification of child/youth at risk for ADHD Methods for screening & diagnosis Treatment template Suicide assessment (for adolescents only) Safety and contingency planning Referral flags 10 Step 1: Identification of Risk for ADHD Well established and significant risk effect Less well established risk effect 1. A previous diagnosis of ADHD 1. Exposure to severe environmental factors (i.e., lead contamination, prenatal exposure of alcohol and cigarette, birth trauma, low birth weight, head injuries). 2. Psychosocial adversity such as maternal depression, paternal criminality, chaotic home environment, and poverty 3. Substance misuse/abuse (early onset of use including cigarettes and alcohol) 4. Head injury (concussion) 2. Family history of ADHD 3. Family history of mental disorders (affective, anxiety, tics or conduct disorder) 4. Psychiatric Disorder: Oppositional Defiant Disorder, Conduct Disorder or a Learning Disorder Possible “group” identifiers (these are not causal for ADHD but may identify factors related to adolescent onset ADHD) 1. School failure or learning difficulties 2. Socially isolated from peers or behavioural problems at home and at school (including gang activity & legal problems) – accident prone. 3. Bullying (victim and/or perpetrator) 11 11 If Child is High Risk… Check for patterns of: › Declining grades › Frequent lates/absences › Discipline concerns › Homework not completed › Concentration problems › Over-activity or inattentiveness Confidentiality & informed consent › Speak with both child and parents › Easier for child to access care › Easier for parents to know what to expect 12 www.freedigitalphotos.net Decreasing Bar Chart by jscreationzs Step 2: Useful Methods for Screening & Diagnosis of ADHD in the Clinical Setting Part of general health visits › Screen at regular visits › Screen teens during visits for contraception/sexual health issues › Presentation of ADHD symptoms may change over time Younger children are more impulsive and hyperactive Adolescents are less hyper, but have inner restlessness, impulsivity and inattention Co-morbidity of ADHD › Anxiety, Opposition Defiant Disorder, Disruptive Mood Dysregulation Disorder, Conduct Disorder, and Learning Disorder › Consider possibility of one or more of these disorders 13 Screening & Diagnosis of ADHD Approx. 65% of children with ADHD still meet diagnostic criteria during adolescence Child/Adolescent may show: › Inattention › Distractibility › Impulsivity › Hyperactivity Requires health provider intervention › Differentiate between normal responses to circumstances or developmental changes in normal children › Use the “Distress versus Disorder” model 14 Freedigitalphotos Africa 31513qkoh8f72ro Screening & Diagnosis of ADHD 3 Sub-categories 1. Predominantly Inattentive › 20 – 30% of children and adolescents with ADHD › Daydreaming, distractibility and difficulty focusing on a single task for a prolonged period 2. Predominantly Hyperactive-Impulsive › 5 – 10% of children and adolescents with ADHD › Manifesting as a situational inappropriate and excessive motor activity such as fidgeting, excessive talking, impulsive actions and restlessness 3. Combined Inattentive/Hyperactive › 60 – 70% of children and adolescents with ADHD › Manifesting as a combination of the above two subtypes 15 Screening & Diagnosis of ADHD No biological diagnostic tests for ADHD › Clinical assessments of: Signs Symptoms Clinical History › Carry out evaluations over more than one visit 2 to 3 visits are often needed No hurry for a diagnosis; Take Your Time 16 freedigitalphotos ID 33138y9acpx7jy3 Clinical Findings for ADHD Early Childhood 3 – 5 years of age Difficulty attending › Reading a storybook with parent, or coloring/drawing “Squirmy” Difficulties “settling” Very active, always on the go › Bumping into things/getting hurt Parents refer to child as: › “Not listening” › “Zippy” › “Always running around” 17 dreamstimefree_113773 Clinical Findings for ADHD Middle Childhood 6-12 years of age Child may not persist long with most tasks › Particularly what they do not want to do Parents report child: › Does not pay attention or listen › Is very forgetful or disorganized Described as: › “Overactive”, “always on the go” & “cannot sit still”, › Acting out of turn › Blurting out in class › More evident in situations where attention is expected www.freedigitalphotos.net Girl With Bunny by Teeratas 18 Clinical Findings for ADHD Middle Childhood 6-12 years of age School reports, “…not living up to academic potential” Difficulty with peers Impulsivity & intrusiveness An active child does not mean ADHD Girls with ADHD may demonstrate inattentiveness, not hyperactive symptoms 19 Clinical Findings for ADHD Adolescence 13 – 19 years of age Easily distracted from tasks Feelings of inner restlessness Stopping short on tasks Forgetful; fail to complete tasks Fidgety Difficulty with relationships › Many “breakups” Impaired temper control Impulsive decision making 20 www.freedigitalphotos.net Glamour by federico stevanin Clinical Findings for ADHD Adolescence 13 – 19 years of age Engage in “risky” behavior › At higher risk for traffic accidents Considered “lacking maturity” for their age Without treatment, exhibit signs of demoralization › Due to negative comments › “Nagging” from parents, teachers, adults and peers › Do not confuse demoralization with depression May get involved in drug use and criminal behavior School drop outs, especially with unidentified learning disability 21 Screening & Diagnosis of ADHD Not likely ADHD if: › Symptoms only in one setting › Not functionally impairing ADHD type symptoms may be › Post Traumatic Stress Disorder (PTSD) › Consider PTSD as a diagnostic possibility in youth who exhibit ADHD symptoms for whom a significant traumatic event has recently occurred. Remember: ADHD prior to age 12. 22 www.digitalphotos.net Stressful by Danilo Rizzuti Youth ADHD Screening Q’s Inquire about substance misuse/abuse - Including marijuana Youth with ADHD may be more likely to use a variety of substances Specialist consultation for substance abuse & ADHD 23 stockxchng ID 1049528