NICU Resident Orientation - University of Missouri
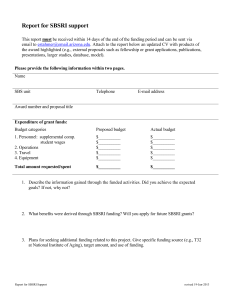
advertisement

Jan Sherman, RN,NNP,PhD Associate Professor of Clinical Practice Neonatal Nurse Practitioner Coordinator Department of Child Health University of Missouri - Columbia Adjunct Teaching Associate Professor College of Nursing University of Missouri - St. Louis College of Nursing University of Missouri - Columbia Updated 07-05-2011 1 Objectives Provide an overview of basic neonatal care To assist you in preparing for your NICU rotation The information is not meant to replace standard neonatal textbooks and only basic information will be discussed in this powerpoint presentation. Additional information can be obtained from the neonatal classic textbooks listed in the references at the end of the presentation Information specific to the NICU at WCH will be presented to you in the NICU 2 Fluids and Electrolyes Fluid and electrolyte management is an important and challenging part of the initial management of any very preterm or critically ill newborn After birth, the newborn rapidly must assume responsibility for fluid and electrolyte balance Primary responsibility lies with caregivers! Challenging for very preterm neonates in whom water loss is large and highly variable 3 Body Compositon of Fetus and Newborn Infant Early stages of development, body mostly water 3rd month fetal life, TBW = 94% of wt 24wks, TBW = 86% of wt 40 wks, TBW = 78% of wt ECF as gestation progresses 59% at 24 wks -> 44% at term Increasing cell numbers and size ICF as gestation progesses 27% at 24 wks -> 34% at term 4 Body Compositon of Fetus and Newborn Infant Neonates are born with an excess of TBW, primarily ECF, which needs to be removed Infants with hydrops have excessive ECF!! After birth, TBW falls Contraction of ECW Mobilization of extracellular fluid related to improved renal function Normal physiologic process 5 Water Loss 2 types of water loss Sensible = primarily urinary, account for ~50% of daily fluid requirements Insensible (IWL) = lost through skin and resp tract IWL Lose of water by evaporation 30% through resp tract 70% through skin Inversely proportion to gest age and wt Premature infants surface area compared to wt 6 7 The graph is only a guideline. Total fluids should be discussed in rounds with the attending. Generally you would start at the low end of the Water Requirements to determine your ml/kg/day of total fluids, i.e., < 750 grams, day 1 – start at 100 ml/kg/day. Fanaroff, A. A., Martin, R. J., & Walsh, M. C. (2010). Neonatal-Perinatal Medicine: Diseases of the Fetus and Newborn. 8 Fluid Requirements Maintenace Fluids = fluid quantities required to preserve neutral fluid balance Total fluid requirements = Maintenance (IWL + urine + stool water) + Growth requirements Stool = 5-10 ml/kg/day Growth = weight gain is 70% water, an infant growing 30-40 gm/day requires 20-25 mL/kg/day of water 9 Calculating Fluid Requirements Take desired ml/kg/day x wt Example: 100 ml/kg/day and 1 kg baby 100 x 1 kg = 100 ml ÷ 24 hrs = 4.1 ml/hr total fluid All of your fluids which the baby is receiving needs to equal 4.1 ml/hr Include all fluids - drips, TPN, lipids, carrier fluids, etc. Can be a challenge with very small infants! 10 To calculate fluid rates i.e. Need 100 ml total fluids in 24 hours = 4.1 ml/hr total fluids Currently have the following fluids running Dopamine = .05 ml/hr x 24 hr = 1.2 ml Dobutamine = .05 ml/hr = 1.2 ml UAC fluids (1/2 NS) = 1 ml/hr = 24ml 20% lipids = 0.5ml/hr = 12ml Glucose/insulin drip = 0.5ml/hr = 12ml 11 100 ml total fluids in 24 hours (Use this number as the initial ml of TPN or primary glucose solution to order – other fluids are subtracted from this initial mo and the amount left will determine the rate of the TPN/glucose solution) - 2.4 ml (Dopamine and Dobutamine) = 97.6 ml - 24 ml (UAC fluids) = 73.6 ml -12 ml (lipids) = 61.6 ml - 12 ml (glucose/insulin drip) = 49.6 ml left to be used for TPN = 49.6 ÷ 24 hours = 2 ml/hr TPN Double check your calculations by adding up all of your hourly rates to be sure it equals your original calculation, i.e 4.1 ml/hr 12 825 grams with total fluids (TF) = 140ml/kg/day .825gm x 140 ml/kg/day = 115ml in 24 hours 115 ml - 16 ml (feeds = 2 ml q 3 hours) = 99 ml - 12 ml ( lipids = 12 ml) = 87 ml left to be used for TPN = 87 ÷ 24 hours = 3.6 ml/hr TPN ** if make baby NPO will need to increase IV fluids to 4.2 ml/hr (16 ml ÷ 24 hr = 0.6 ml/hr, 3.6 + 0.6 = 4.2ml/hr) to maintain same TF Replacement of Deficits and Ongoing Losses Be careful to calculate all output Chest tubes, repogyl, surgical wounds Excessive output needs to be replaced to avoid dehydration – watch urine output closely!! Generally replace output ml:ml May use ½ replacement – discuss with attending General guideline to consider replacement is if output is > 5ml/kg every 4 hours NS or LR most commonly used for replacement Can send sample of output for electrolyte analysis Determine what fluid to use for replacement based on electrolyte content of output 14 Fluid Requirements Be cautious with your fluid administration Increase fluids if Weight loss excessive , i. e. > 10% birth weight Na+ is rising s/s dehydration: HR, ↓ BP, BUN, metabolic acidosis Urine output low (< 2 ml/kg/hr) *** be sure to check BUN/creatinine if renal failure is the cause of ↓ urine output, be cautious with fluid increases!! Poor perfusion Cardiac, sepsis 15 Fluid Requirements Decrease fluids if Excessive wt gain Na+ is falling – dilutional hyponatremia Urine output ↓ from renal failure Indocin or Ibuprofen administration may cause renal dysfunction Evidence of PDA Fluid overload may worsen a PDA 16 Fluid Composition Glucose Basic metabolic needs for glucose are 4-8 mg/kg/min Do not give > D10W in a peripheral line without discussing with the attending Central lines (UVC or PICC) may run higher glucose concentrations To calculate glucose infusion rate (GIR) ml/kg/day 24 hr 60 minutes x mg/ml of glucose i.e. 60ml/kg/day of D10W (100mg/ml) 60 24 60 x 100 = 4.2 mg/kg/min GIR If you have multiple sources of glucose, i.e. drips, TPN, calculate each GIR separately and add together for total GIR 17 Fluid Composition Watch for hyperglycemia Glycosuria Premature infants may have a low renal threshold for glucose and can spill glucose at chemstrip of 120 Normal threshold is > 180 chemstrip Osmotic diuresis may occur Rapidly become dehydrated with increased urine output Calculate the GIR Baby may be receiving excessive glucose!! Maximum GIR should be discussed with the attending 18 Fluid Composition Hypoglycemia Watch IDM and IUGR/SGA infants closely Both may have high glucose needs > 8mg/kg/min GIR 19 TPN American Academy of Pediatrics, the clinician’s objective is for the infant (< 1500 grams) to grow as well as in-utero Prevent extrauterine growth restriction! Glucose and protein administration soon after birth of are of primary importance Protein turnover and protein breakdown increase proportionately with the immaturity of the baby 20 TPN ~1 g/kg/day of amino acids (AA) Helps with protein synthesis Keeps the baby in nitrogen equilibrium Provides a positive nitrogen balance Early aggressive use of AA to prevent "metabolic shock.“ Irrepressible glucose production may be the cause of the socalled glucose intolerance Start with Vanilla TPN at 60ml/kg/day on admission Remainder of total fluids composed of D5W or D10W < 1000 grams may need D5W in fluids to prevent hyperglycemia Adamkin, D. (2006). Nutrition Management of the Very Low-birthweight Infant I. Total Parenteral Nutrition and Minimal Enteral Nutrition. NeoReviews Vol.7 No.12 2006 e602 21 Protein Maximum AA intake is usually 3 gm/kg/day Intakes of 3.5 g/kg/day for infants weighing less than 1,200 g may be appropriate when enteral feedings are extremely delayed or withheld for prolonged periods Adamkin, D. (2006). Nutrition Management of the Very Low-birthweight Infant I. Total Parenteral Nutrition and Minimal Enteral Nutrition. NeoReviews Vol.7 No.12 2006 e602 22 Lipids Lipids are essential components of parenteral nutrition for preterm infants to provide essential fatty acids (EFAs) Parenteral lipids are an attractive source of nutrition in the first postnatal days High energy density Energy efficiency Isotonic with plasma Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 23 Lipids 3 - 7 day delay in supplying lipids leads to biochemical EFA deficiency Increases antioxidant susceptibility Reduces body and brain weights EFA deficiency can be prevented with introduction of as little as 0.5 to 1 gm/kg/day of lipids Discuss amount of lipids in rounds with the attending Always use 20% lipids, not 10% Limit lipids to 40 – 50% of total calories (Gomella, 2009. Page 78) May cause ketosis Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 24 Potential Adverse Effects of Parenteral Lipids Increased risks of sepsis coagulase-negative staphylococci (CONs) Displacement of bilirubin from albumin Increased unbound bilirubin -> increased risk of kernicterus Pulmonary complications Deposition of fat globules Increase in pulmonary vascular resistance Activation of inflammatory mediators Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 25 Practical Tips for Lipids Fat is a concentrated energy source, providing 9 kcal/g. Use of 20% lipid emulsion is preferable to a 10% solution Smaller volume to administer Decrease the risk of hypertriglyceridemia, hypercholesterolemia, and hyperphospholipidemia. Plasma triglycerides are monitored Discuss with attending when to check Serum triglycerides should be <200 mg/dL If the infant has severe hyperbilirubinemia or severe respiratory disease Consider discontinuing lipids or decrease dose Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 26 Practical Tips for Lipids Maximum lipid dosage is usually 3 gm/kg/day Calculate ml of lipids Gm/kg/day ÷ 0.2 gm fat x kg = ml to give i.e. 1.5 kg, 2 gm/kg/day lipids 2 gm/kg/day ÷ 0.2 x 1.5 kg = 15 ml lipids in 24 hours = 0.6 ml/hr of lipids Hourly infusion should not exceed 0.12 g/kg/hour Give over 24 hours Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 27 Enteral Nutrition The timing of initial feedings for the preterm infant has been debated for nearly a century remains controversial! Swallowed amniotic fluid may play in nutrition and in the development of the gastrointestinal tract By the end of the third trimester, amniotic fluid provides the fetus with the same enteral volume intake and ~ 25% of the enteral protein intake of a term, breastfed infant Adamkin, D. (2006). Nutrition Management of the Very Low-birthweight Infant .I. Total Parenteral Nutrition and Minimal Enteral Nutrition. NeoReviews Vol.7 No.12 2006 e602 28 Enteral Nutrition TPN does little to support the function of the gastrointestinal tract Animals studies have shown that intraluminal nutrition is necessary for normal gastrointestinal structure and functional integrity Prevents intestinal atrophy Enteral feedings Have both direct trophic effects and indirect effects due to the release of intestinal hormones 29 Enteral Nutrition Feeding volumes are to be discussed in rounds with the attendings General feeding guidelines VLBW infant (<1000 gm, < 28 wks) Gavage feed only PO feeds after 32 – 34 weeks PMA when suck/swallow coordination has developed Start at 10-20 ml/kg/day, every 3 hours bolus Advance per attending – generally 10 -20 ml/kg/day Breast milk is ideal, if no breast milk use Special Care 20cal Advance to 24cal after full feedings attained or at direction of the attending Gomella, 2009. Page 92 -95 30 So why aren’t we more aggressive with feeding…. Necrotizing Enterocolitis (NEC) NEC is defined as an ischemic and inflammatory necrosis of the bowel primarily affecting premature infants (Gomella, 2009) 10% of cases are seen in term infants Rarely see until after feedings are initiated 10 – 30% mortality associated with NEC 31 Minimal Enteral Nutrition NEC occurs rarely in infants who are not being fed Association between feedings and NEC Feedings thought to act as vehicles for the introduction of bacterial or viral pathogens or toxins into the gut Efforts aimed at minimizing the risk of NEC Focused on the time of introduction of feedings Feeding volumes Rate of feeding volume increments Gut priming, minimal enteric feedings, hypocaloric feedings, or trophic feedings are all different names for gut stimulation 32 Enteral Nutrition – Feeding Intolerance Residuals – examine infant and if exam benign < 20% of feeding can be refed (Gomella, 2009. Page 92) and full volume feedings given if > 20% consider subtracting volume of residual from feeding volume i.e. feeding to be given = 20ml – 5ml residual = 15ml of new feeding and return the 5ml of residual Persistent large volume residuals, bilious or bloody aspirates, emesis, bloody stools, abdominal distention, increased apnea and bradycardia, hypotension, acidosis, change in LOC, decreased urine output Exam infant’s abdomen look for distention, bowel loops, guarding , discoloration Obtain KUB Hold feedings until KUB seen and condition discussed with attending 33 34 35 Radiographic Determination of NEC Radiographs can help predict the severity of NEC Duke abdominal assessment scale (DAAS) Tool for predicting the severity of disease in neonates and infants with suspected NEC Patients with higher DAAS scores were more likely to undergo surgical intervention than patients with lower scores The DAAS provides a standardized 10-point radiographic scale that increases with disease severity For every 1-point increase in the DAAS score, patients were statistically significantly more likely to have severe disease as measured by need for surgical intervention Coursey, C.A., Hollingsworth, C. L. Wriston, C. Beam, C. Rice, H., & Bisset, G. (2009). Radiographic predictors of disease severity in neonates and infants with necrotizing enterocolitis. AJR Am J Roentgenol. 2009 Nov;193(5):1408-13. . 36 Duke Abdominal Assessment Scale (DAAS) 37 Pneumatosis intestinalis gives a bubbly appearance to bowel . May see persistent dilated static loop of bowel, portal venous air or pneumoperitoneum if the bowel has perforated. Bubbles are filled with hydrogen gas 38 air in the portal vein – portal venous air The plain abdominal film shows: 1) air in the portal vein 2) air in the bowel walls 3) a large pneumoperitoneum [subdiaphragmatic free air 4) perihepatic free air 5) double wall sign (blue arrows) 6) triangle sign (green arrows) 7) falciform ligament (red arrow) 39 Management of NEC NPO Respiratory support May need fluid boluses and pressors to maintain adequate blood pressure Obtain CBC, CRP, blood gas, and blood culture Antibiotic coverage Usually Vanc, Gent, and Clindamycin or Flagyl 40 Management of NEC Serial abdominal films to watch for perforation Usually every 6 – 12 hours Sooner if change in exam noted Can transilluminate abdomen to check for perforation Bowel rest and decompression with repogyl to low intermittent suction Surgical consult as needed 41 Fluid Composition: Potassium Potassium Ideal lab range is 3.5-5.5 mEq/L. Discuss supplemental K+ in the first days of life with the attending Be cautious with potassium administration! Don’t automatically add potassium to IV fluids in preterm infants Gomella, 2009. Pages 304-307. 42 Hyperkalemia Serum K+ > 6mEq/L. Etiology Heelstick vs central Heelstick values may be hemolyzed giving false elevations. Redraw by venous or arterial sample to confirm Excessive supplemental K+ Bruising Renal failure Renal immaturity Infants < 800 gram, first 2-3 days of life Pathologic hemolysis of RBC from IVH or other thrombus NEC – tissue necrosis Adrenal insufficiency Gomella, 2009. Pages 304-307. 43 Hyperkalemia Metabolic acidosis decrease in pH by 0.1 unit -> increase in K+ by 0.3-1.3 meq/l Medications which can cause hyperkalemia Digoxin -> redistribution of K+ Aldactone – K+ sparing Indomethocin -> renal dysfunction Gomella, 2009. Pages 304-307. 44 Hyperkalemia Look at EKG pattern on the infant’s monitor If no EKG changes stop supplemental K+ Consider Lasix if renal function is adequate Consider Kayexalate (sodium polystyrene sulfonate) Binds K+ Dose = 1 gram/kg/dose rectally q 2-6 hrs 1 gram resin removes ~ 1 meq K+ Works slowly!! Watch lytes closely with frequent labs Gomella, 2009. Pages 304-307. 45 Hyperkalemia If EKG changes -> medical emergency Give Calcium gluconate IV Decreases myocardial excitability Correct any acidosis with NaHCO3 Glucose – insulin drip Inhaled albuterol 46 47 Monitoring Fluid and Electrolyte Balance Normal values Urine output = > 2ml/kg/hr Urine SG = 1.008-1.012 Weight loss no greater than 10 - 15% of BW Calculate daily and report to attending in rounds i.e. down 12% of birth weight today Base deficit < - 6 Watch closely for acidosis in preterm infants BD > - 6 needs attention! After full feedings or full TPN attained infant should gain 10-30 gm/kg/day 20-30 gm/kg/day ideal 48 References Adamkin, D. (2007). Use of Intravenous Lipids in Very Low-birthweight Infants. NeoReviews Vol.8 No.12 2007 e543 Adamkin, D. (2006). Nutrition Management of the Very Low-birthweight Infant I. Total Parenteral Nutrition and Minimal Enteral Nutrition. NeoReviews Vol.7 No.12 2006 e602 Christensen, R. D. (2000). Hematologic Problems of the Neonate. Cloherty, J. P., Eichenwaid, E. C., Stark, A. (2008). Manual of Neonatal Care, 5th ed. Lippincott. Coursey, C.A., Hollingsworth, C. L. Wriston, C. Beam, C. Rice, H., & Bisset, G. (2009). Radiographic predictors of disease severity in neonates and infants with necrotizing enterocolitis. AJR Am J Roentgenol. 2009 Nov;193(5):1408-13. Fanaroff, A. A., & Martin, R. J. (2002). Neonatal-Perinatal Medicine: Diseases of the Fetus and Newborn. Gomella, T. L. (2009). Neonatology management, procedures, on-call problems, diseases and drugs. Polin, R. A., Fox. W. W., Abman, S. H. (2004). Fetal and Neonatal Physiology. Taeusch, H. W., Ballard, R. A., & Gleason, C. A. (2005). Avery’s Diseases of the Newborn. 8th ed. 49 CNS One of the primary concerns for infants in the NICU is the development of intracranial hemorrhage which can cause later neurologic issues Term infants tend to have: Subdural, subarachnoid, or subtentorial Generally related to birth trauma, hypoxic-ischemic events, coagulopathies (thrombophilias or thrombocytopenia) Gomella, 2009. pg 549 - 557 50 CNS Preterm infants tend to have: Intraventricular (IVH) Generally originates from vascular rupture in the germinal matrix Incidence of IVH decreases with increasing gestational age Rare in newborns > 32 weeks’ gestational age or > 1,500 gm birthweight Periventricular leukomalacia (PVL) PVL of the white matter may occur in isolation or follow an IVH May occur in preterm and term infants 51 Coronal View 52 53 Germinal matrix -located in the caudo-thalamic groove The occipital horn of the lateral ventricle is filled with choroid plexus. The choroid tucks up in the caudothalamic groove in the floor of the lateral ventricle and may be echogenic. Sagittal View 54 CNS General presentation Seizures Rapid drop in hematocrit Sudden deterioration in condition Diagnosis Preterm HUS to look for IVH – can be done at the bedside Term HUS CT scan – rapid test, will show hemorrhagic damage MRI – Generally done with more stable infant – time consuming Specific for hemorrhage and hypodensities Gomella, 2009. pg 549 - 557 55 CNS The most widely used classification system for IVH is that originally described by Papile and associates Grades from 1 to 4 with increasing severity Rhine, W. D. & Blankenberg, F. G. , (2001). Cranial Ultrasonography. NeoReviews Vol.2 No.1 January 2001 56 CNS ICH usually begins within the first 24 to 72 hours of life May have occurred antenatal Ask the attending when to obtain the HUS – generally the HUS will be done at 7 days of age in our NICU HUS may be obtained sooner on very sick infants or infants who have: Unexplained hematocrit drop Acidosis Change in neurologic status 57 Grade 1 IVH – Referred to as a germinal matrix or subependymal hemorrhage Seen on HUS as an abnormally increased number of echoes in the caudothalamic groove (ie, notch) in the expected location of the germinal matrix. 58 Bilateral small germinal matrix hemorrhages http://www.google.com/imgres?imgurl=http://neuropathology.neoucom.edu/chapter3/images3/3ivh.jpg&imgrefurl=http://neuropathology.neoucom.edu/chapter3/chapter3dGmh.html&usg=__O5BiBTFDXt_6r1m7R0DbzMgNLo=&h=446&w=500&sz=170&hl=en&start=5&itbs=1&tbnid=3kwwgVKjog8fYM:&tbnh=116&tbnw=130&prev=/images%3Fq%3DGrade%2B1%2 59 BIVH%26hl%3Den%26sa%3DG%26gbv%3D2%26tbs%3Disch:1 Grade 2 describes extension of a germinal matrix/subependymal hemorrhage into the ventricles without any ventricular enlargement A. The sagittal view demonstrates the echogenic bulbous collection of blood that bears no resemblance to the normal germinal matrix that tapers as it courses anteriorally in the caudothalamic groove and also never is seen anterior to the foramen of Monro. B. Coronal view, showing a bulbous echogenic collection of blood in the left caudothalamic groove. C. A sagittal view through the anterior fontanelle that is angled slightly more posteriorly shows an echogenic clot filling the occipital horn posterior to the calcar avis. The choroid plexus never is seen in the occipital horn. 60 Grade II IVH http://www.google.com/imgres?imgurl=http://neuropathology.neoucom.edu/chapter3/images3/3ivh.jpg&imgrefurl=http://neuropathology.neoucom.edu/chapter3/chapter3dGmh.html&usg=__O5BiBTFDXt_6r1m7R0DbzMgNLo=&h=446&w=500&sz=170&hl=en&start=5&itbs=1&tbnid=3kwwgVKjog8fYM:&tbnh=116&tbnw=130&prev=/images%3Fq%3DGrade%2B1%2 61 BIVH%26hl%3Den%26sa%3DG%26gbv%3D2%26tbs%3Disch:1 Grade 3 has blood extending into the ventricles and causing ventriculomegaly at the time of the initial observation of IVH. Grade 3 germinal matrix hemorrhage 3 and 10 days after birth. A. On day 3 of life, the coronal view demonstrates massive bilateral IVH and germinal matrix hemorrhage with ventricular dilation. B. The sagittal view confirms the presence of massive IVH and germinal matrix hemorrhage. On day 10 of life, progressive posthemorrhagic hydrocephalus is evident on the coronal (C) and sagittal (D) views. 62 Grade 4 describes a germinal matrix hemorrhage that dissects and extends into the adjacent brain parenchyma, irrespective of the presence or absence of IVH. It is also referred to as an intraparenchymal hemorrhage (IPH) when found elsewhere in the parenchyma. Bleeding extending into the periventricular white matter in association with an ipsilateral IPH has been classified as periventricular hemorrhagic venous infarction (PHVI). 63 Grade IV IVH http://www.google.com/imgres?imgurl=http://neuropathology.neoucom.edu/chapter3/images3/3ivh.jpg&imgrefurl=http://neuropathology.neoucom.edu/chapter3/chapter3dGmh.html&usg=__O5BiBTFDXt_6r1m7R0DbzMgNLo=&h=446&w=500&sz=170&hl=en&start=5&itbs=1&tbnid=3kwwgVKjog8fYM:&tbnh=116&tbnw=130&prev=/images%3Fq%3DGrade%2B1%2 64 BIVH%26hl%3Den%26sa%3DG%26gbv%3D2%26tbs%3Disch:1 Treatment of IVH Supportive Ventilation Volume expansion and pressors as needed PRBC and platelets as needed Check CBC frequently Correct anemia and thrombocytopenia as directed by attending Correct acidosis 65 PVL in weeks 1 and 4 of life. A. Coronal view of the frontal lobe region demonstrates abnormally increased periventricular echogenicity bilaterally at week 1. B. Follow-up coronal view at week 4 demonstrates cystic degeneration, involution of the periventricular white matter and mild ventricular dilation. PVL describes a characteristic pattern of cystic degeneration over the next 2 to 3 weeks, resulting in a “swiss cheese” pattern of white matter loss that can be detected readily with CUS However, PVL can arise without ICH and vice versa. Affects white matter tracts of the brain and can cause severe neurological problems with movement. 66 Hypoxic-ischemic Encephalopathy (HIE) Birth Depression HIE in both preterm and term neonates may cause a wide range of CNS injuries that may not be visible by HUS In the term newborn, severe HIE can lead initially to generalized cerebral edema Including small, slit-like ventricles Poor gray-white signal differentiation on HUS 67 Treatment of HIE Supportive Ventilation Volume expansion and pressors as needed Correction of acidosis Head and Body Cooling Recent advance has been development of hypothermia in which the body and brain are cooled down to about 92°F (33.5°C) Hypothermia is appropriate for full-term babies Generally must begin treatment within 6 hours of birth 68 Retinopathy of Prematurity Retinopathy of prematurity (ROP) is a disorder of retinal vascular development in preterm infants. It remains a major cause of childhood blindness worldwide Retinal vascular development is incomplete in preterm infants. Postnatal interference with normal development may lead to ROP 69 Pathogenesis of ROP Still unknown Current concept of the pathogenesis of ROP suggests that preterm birth interrupts the normal processes of retinal blood vessel development Postnatal developing retina is exposed to a less stable and relatively hyperoxic oxygen environment 70 Pathogenesis of ROP Normal physiologic hypoxia “drive” of angiogenesis is reduced. Local and systemic concentrations of growth factors, notably insulin-like growth factor 1 (IGF-1) are low Process of retinal vascularization is delayed Peripheral retina remains avascular 71 Pathogenesis of ROP Preterm infants have low circulating concentrations of IGF-1, which increase with postnatal growth When tissue concentrations of IGF-1 reach a critical threshold level, vascular endothelial growth factor (VEGF) signaled angiogenesis is permitted Rapid-onset, excessive VEGF effects are seen in the retinal blood vessels 72 Pathogenesis of ROP Extra-retinal new vessels grow into the vitreous (stage 3 ROP) Posterior retinal blood vessels become dilated and tortuous (plus disease) If the condition is untreated, a progressive gliosis of the retina and vitreous occurs Leads to retinal detachment and blindness (stage 4 and stage 5 ROP) 73 Screening Examination of the Retina Most infants born at less than 28 weeks’ gestation develop some degree of ROP In most, the disease is mild and regresses spontaneously A small proportion of infants, even up to 32 weeks’ gestation (and if SGA at even greater gestations), develop potentially severe retinopathy Screening of infants at risk can monitor the progress of retinopathy Timely intervention has a good chance of preventing progression and preserving vision 74 Screening Examination of the Retina AAP Guidelines on Timing of First Eye Exam Based on Gestational Age at Birth Gestational Age at Birth, wk 22a 23a 24 25 26 27 28 29 30 31b 32b Shown is a schedule for detecting pre-threshold ROP with 99% confidence, usually well before any required treatment. Infants with a birth weight of less than 1500 g or gestational age of 30 weeks or less (as defined by the attending neonatologist) and selected infants with a birth weight between 1500 and 2000 g or gestational age of more than 30 weeks with an unstable clinical course, including those requiring cardiorespiratory support and who are believed by their attending pediatrician or neonatologist to be at high risk, should have retinal screening examinations performed after pupillary dilation using binocular indirect ophthalmoscopy to detect ROP." a = This guideline should be considered tentative rather than evidence-based for infants with a gestational age of 22 to 23 weeks because of the small number of survivors in these gestational age categories. b = If necessary POLICY STATEMENT ERRATA: Section on Ophthalmology, American Academy of Pediatrics; American Academy of Ophthalmology (2006). American Association for Pediatrics Ophthalmology and Strabismus. Screening Examination of Premature Infants for Retinopathy of Prematurity. PEDIATRICS 2006;117:572–576. Age at Initial Examination, wk 31 31 31 31 31 31 32 33 34 35 36 Postmenstrual Chronologic age 9 8 7 6 5 4 4 4 4 4 4 75 Classification of Clinical ROP Location The retina is divided into three zones – I, II, and III Zone I - which is most posterior, consists of a circle with a radius of twice the distance from the optic disc to the center of the macula, centered on the optic disc Zone II extends from zone I forward to the anterior edge of the retina (ora serrata) on the nasal side of the eye Centered on the optic disc. Ora serrata is closer to the optic disc on the nasal side than on the temporal side of the eye Zone III is the retina anterior to zone II Only present on the temporal side 76 ROP Zones 77 Classification of Clinical ROP In the absence of retinopathy, the retina of the very preterm infant merges imperceptibly from vascularized centrally to avascular peripherally ROP affects the entire retina Normal immature retina, not fully vascularized 78 Classification of Clinical ROP Stage 1 ROP: A flat line of demarcation occurs between the vascular and avascular retina. Stage 2 ROP: The line of demarcation acquires volume to become a ridge. Tufts of new vessels may appear on the posterior edge of the ridge, but these vessels still are within the retina Stage 2 ROP, indicated by the development of a ridge between the vascular and avascular retina 79 Classification of Clinical ROP Stage 3 ROP Neovascularization can be seen within the ridge, and extraretinal vascularization extends out of the retina Stage 3 ROP, showing neovascularization within the ridge and extraretinal vascularization out of the retina. Courtesy of Professor Michael O’Keefe, Dublin, Ireland. 80 Classification of Clinical ROP Stage 4 ROP Partial retinal detachment occurs, May be extrafoveal or foveal Stage 5 ROP Eventually total retinal detachment may occur With resulting complete blindness 81 Classification of Clinical ROP Plus disease: Indicated by tortuosity of the posterior retinal vessels 82 Treatment of ROP The finding of threshold ROP, as defined in the Multicenter Trial of Cryotherapy for Retinopathy of Prematurity, may no longer be the preferred time of intervention Treatment may also be initiated for the following retinal findings: ● zone I ROP: any stage with plus disease ● zone I ROP: stage 3—no plus disease ● zone II: stage 2 or 3 with plus disease 83 Treatment of ROP BIO-delivered diode laser ablation of the peripheral avascular retina has become the usual method of treating ROP cryotherapy is used rarely Aim is to produce almost confluent burns of all areas of the avascular retina anterior to the ROP ridge, extending to the ora serrata Careful primary treatment, ensuring complete cover of the retina and avoiding untreated “skip” areas, reduces the risk for retreatment 84 Treatment of ROP New approach to ROP treatment is under investigation Intravitreal injection of anti-VEGF antibodies is used widely in ophthalmology for the treatment of neovascular forms of age-related macular degeneration and diabetic retinopathy Injections are administered under sterile conditions through the sclera adjacent to the cornea into the vitreous A volume of 0.025 mL is used A single injection appears to be sufficient in most cases. Normal retina is not subjected to laser ablation Permanent scarring Some reduction of the peripheral visual field 85 References Fleck, B. W. & McIntosh, N. (2009). Retinopathy of Prematurity: Recent Developments. NeoReviews 2009;10;e20-e30. DOI: 10.1542/neo.10-1-e20 AAP 2006 Position Statement: Screening Examination of Premature Infants for Retinopathy of Prematurity. PEDIATRICS Vol. 117 No. 2 February 2006, pp. 572-576 (doi:10.1542/peds.2005-2749) 86 References Christensen, R. D. (2000). Hematologic Problems of the Neonate. Cloherty, J. P., Eichenwaid, E. C., Stark, A. (2007). Manual of Neonatal Care, 6th ed. Lippincott. Fanaroff, A. A., Martin, R. J., & Walsh, M. C. (2010). Neonatal-Perinatal Medicine: Diseases of the Fetus and Newborn. Gomella, T., et al. (2009). Neonatology: Management, Procedures, On- Call Problems, Diseases, and Drugs. 6th ed. MacDonald, MC, Mullett, MD, & Seshia, MK (2005). Avery’s Neonatology: Pathophysiology & Management of the Newborn. 6th ed. Polin, R. A., Fox. W. W., Abman, S. H. (2004). Fetal and Neonatal Physiology. Taeusch, H. W., Ballard, R. A., & Gleason, C. A. (2004). Avery’s Diseases of the Newborn. 8th ed. 87 Jobe, A. H., The New BPD. NeoReviews, Oct 2006; 7: e531 - e545. 88