IDSA Candidiasis Guidelines: Update for Fellows
advertisement

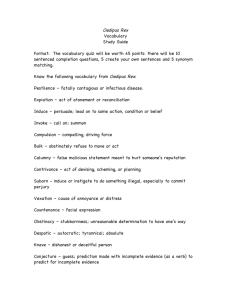
2008 IDSA Candidiasis Guidelines John H. Rex, MD Adjunct Professor of Medicine; University of Texas Medical School-Houston Vice President Clinical Infection, AstraZeneca Pharmaceuticals Rex summary of updated IDSA Candidiasis guidelines.ppt 1 How were they created? • Current version is from 2004 – Clin Infect Dis 2004;38:161-189 • A group of 14 international authorities began work a revision in spring 2007. • There are 15 major topics addressed in the revised version – Each recommendation is given a ‘grade’ based on the strength of evidence (eg, A-I, B-II, C-III) – An evidence summary follows each recommendation Rex summary of updated IDSA Candidiasis guidelines.ppt 2 Key organism principles • Helpful to know tiers of progressive difference – (most virulent, most susceptible): albicans, parapsilosis, tropicalis, dubliniensis – (intermediate): glabrata – (least virulent, least susceptible: krusei • You often know quickly if C. albicans – It’s the one that is “germ tube-positive” • Just knowing species is very helpful – P = Plastic = parapsilosis. Look for the device! – Resistance patterns • • • • glabrata & krusei: Azoles are dicey. Newer azoles are better parapsilosis: Echinocandins sometimes a little weaker lusitaniae: Amphotericin resistance is frequent guilliermondii: higher azole and candin MICs – Hint about your patient • Glabrata and krusei are weaklings. When seen, says much about patient Rex summary of updated IDSA Candidiasis guidelines.ppt 3 Key drug principles • Voriconazole – Fatty meal reduces absorption – IV form uses cyclodextrin: not well cleared by dialysis – Lots of drug-drug interaction • Candins – Very few convincing differences – Usually cross-resistant – but not always! (emerging data) • Amphotericins – Always use trade name for lipid-associated forms – Do not utter phrase “liposomal amphotericin B”: error very easy • • • • Liposomal amphotericin B = AmBisome Amphotericin B lipid complex = ABLC = Abelcet Amphotericin B colloidal dispersion = ABCD = Amphotec (Classic ampho = Amphotercin B deoxycholate = Fungizone) Rex summary of updated IDSA Candidiasis guidelines.ppt 4 Major guideline changes from 2004 • Emphasis on fluconazole and echinocandins as the ‘preferred choices’ for proven/suspected invasive disease • De-emphasis on amphotericin B and lipid-associated amphotericin B under most circumstances • Concept of step down therapy is strongly encouraged – Voriconazole generally advised as step down therapy for selected isolates (most notably, C. krusei) • There is little distinction made among the echinocandins • Fluconazole prophylaxis in neonatal units is limited to high risk sites • Resource-limited environments are acknowledged Rex summary of updated IDSA Candidiasis guidelines.ppt 5 Candidemia & not neutropenic • If species is unknown, either fluconazole (800mg loading dose, 400 mg daily) or an echinocandin is appropriate initial therapy for most adult patients (AI) • An echinocandin is favored if – Moderately severe to severe illness, – Recent azole use for treatment or prophylaxis (AIII), or – Isolate is known to be C. glabrata or C. krusei (BIII) • Fluconazole for patients who are – less critically ill and – who have no recent azole exposure (AIII). • Move from candin to fluconazole when isolates likely susceptible to fluconazole (e.g., C. albicans) and patient is clinically stable (AIII) • Remove or exchange intravenous catheters • Treat for two weeks after clearance of bloodstream Rex summary of updated IDSA Candidiasis guidelines.ppt 6 Other settings • Thinking of non-neutropenia as the start point – The less you know or – The more the patient scares you • The more the guidelines point to – An echinocandin – A (lipid-associated) amphotericin B • But, for resource constrained settings… – The guidelines do note that classic AmB works Rex summary of updated IDSA Candidiasis guidelines.ppt 7 A Survey of a Few Other Selected Topics “I don’t want you to make the wrong mistake” —Yogi Berra Rex summary of updated IDSA Candidiasis guidelines.ppt 8 Candidemia: Who do we treat? • Answer: Essentially everybody – Even a single +BC can be relevant – Concerned about hematogenous seeding • Spread to the eye – – – – Can cause blindness Lesions are common! MSG study: 29% rate Krishna: 26% Rex summary of updated IDSA Candidiasis guidelines.ppt 9 Eye followup • Krishna et al. Eye 14: 30-34, 2000 – – – – 31 patients with fungemia, followed to 6 mos Exam by 72h: 5/31 (16%) had a lesion Exam at 7d: 1/21 (5%) had a new lesion Exam at 14d: 2/16 (13%) had a new lesion • All chorioretinitis, no vitreal disease • Duration of fungemia was a weak clue – 2.5 vs. 4.3 days (no disease vs. disease) Rex summary of updated IDSA Candidiasis guidelines.ppt 10 Catheter Exchange? Yes! • Lots of consistent data – Without catheter removal, 82% had persistent infection • Lecciones, Clin Infect Dis 1992;14:875-883 – Shortened duration of fungemia from 5.6 to 2.6 days • P < 0.001 (Rex, Clin Infect Dis 1995;21:994-996) – Reduced mortality: 41% to 21% • P < 0.001 (Nguyen, Arch Intern Med 1995;155:2429-2435) • Especially true for C. parapsilosis – Very strong link with catheters • Kojic, Clin Microbiol Rev 2004;17:255-267 Rex summary of updated IDSA Candidiasis guidelines.ppt 11 Catheter Exchange? Other Sources • ~ 15% of candidemia patients have another obvious source (urine, abscess) • The gut may be a cryptic source • What does this imply? Rex summary of updated IDSA Candidiasis guidelines.ppt 12 Catheter Exchange? Definite Maybe • In non-cancer patients, suspect the catheter – Unless another source is apparent • After cytotoxic chemotherapy, think twice – Gut may be source, effect of removal is less? • C. parapsilosis is the clear exception • More data & better tools needed here – Differential quantitative and time-to-growth central/peripheral BC • Bouza, Clin Infect Dis 2007;44:820-6. – We keep wishing for good serodiagnostic tools – We have several (beta-glucan, PCR) but none have produced high levels of confidence • Kedzierska, Eur J Clin Microbiol Infect Dis 2007;26:755-766 • Nett, J Infec Dis 2007;195:1705-1712. Rex summary of updated IDSA Candidiasis guidelines.ppt 13 Empirical Therapy • In the febrile non-neutropenic patient? – Early treatment is theoretically attractive • IDSA Guidelines – “The specific basis for selecting non-neutropenic patients who should receive empiric antifungal therapy is unclear, but should be based on at least one of the following: clinical assessment of risk factors, serologic markers for invasive candidiasis, and/or culture data from non-sterile sites (BIII).” • My rules – – – – Antibiotics, lines, no other source, and… Colonized somewhere with Candida I don’t distinguish sites: anywhere works for me The more sites or fungus the better (see work of Pittet) • Prophylaxis? Even hazier Rex summary of updated IDSA Candidiasis guidelines.ppt 14 Candiduria • Asymptomatic candiduria – No treatment unless high-risk dissemination (AIII). – Focus on elimination of predisposing factors. (BIII). • High risk for dissemination – Urologic manipulations (BIII) • Use short course fluconazole or even amphotericin B – Neutropenic patients and low birth weight infants • Treat as for invasive candidiasis. • Consider imaging kidneys/collecting system (BIII) Rex summary of updated IDSA Candidiasis guidelines.ppt 15