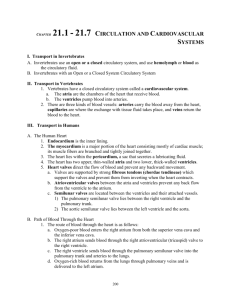
Circulatory System – designed for transportation of oxygen, nutrients
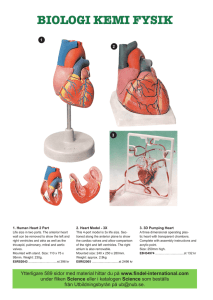
advertisement

Circulatory System – designed for transportation of oxygen, nutrients, cell wastes, hormones, and other substances vital for body homeostasis • Two major divisions – the cardiovascular system and lymphatic system • Heart - major organ of the circulatory system hollow, four chambered about the size of a person’s fist Vessels: lymph vessels and arteries, veins, and capillaries for blood Blood Vessels – transports blood from the heart to the capillaries and back to the heart • Blood leaves heart -> large arteries → smaller arteries -> arterioles -> capillaries for gas and solute exchange → venules → veins → heart • Arteries always carry blood away from heart; veins always return blood to the heart • Exchanges between tissue cells and blood occur only in the capillary beds Blood Vessel Structure • Tunica intima – Endothelial layer (squamous epithelium) that lines the lumen – slick surface decreases friction for moving blood • Tunica media – mostly smooth muscle and elastic tissue • smooth muscle is controlled by sympathetic nervous system – changes diameter of vessels – as vessels dilate or constrict, blood pressure increases or decreases • Tunica externa – outermost tunic – collagen fibers that protect and reinforce vessels Elastic Arteries • Thick-walled arteries near the heart; the aorta and its major branches – Large lumen allow low-resistance conduction of blood – Contain elastin to allow for recoil from blood pressure – Has the most smooth muscle to allow for dilation and constriction Muscular Arteries and Arterioles • Muscular arteries – distal to elastic arteries; deliver blood to body organs • Arterioles – smallest arteries; lead to capillary beds – Control flow into capillary beds via vasodilation and constriction Capillaries • The smallest blood vessel – Walls are one cell thick – Allow only a single RBC to pass at a time – – about 1 mm long (combined length in body = 60,000 miles) all cells in body are less than a mm away from any capillary for exchanges between blood and interstitial fluid for gases and wastes Venous System: Venules • Venules are formed when capillary beds unite – Allow collected fluids and solutes to pass from the tissues into the circ. system • low pressure (about 2 mmHg); too low to return blood to heart against gravity Veins • Veins are: – Formed when venules converge • Veins have much lower blood pressure and thinner walls than arteries • To return blood to the heart, veins have special adaptations – Large-diameter lumens, which offer little resistance to flow – Valves which prevent backflow of blood when blood is pushed up by skeletal muscle contraction Blood Pressure (BP) • Force per unit area exerted on the wall of a blood vessel by its contained blood – Expressed in mm Hg – Measured in reference to systemic arterial BP in large arteries near the heart – Systolic- when heart contracts, higher BP – Diastolic- when heart relaxes and fills up with blood • The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas Factors Aiding Venous Return • Venous BP alone is too low to promote adequate blood return and is aided by the: – Respiratory “pump” – pressure changes created during breathing suck blood toward the heart by squeezing local veins – Muscular “pump” – contraction of skeletal muscles push blood toward the heart • Valves prevent backflow during venous return Monitoring Circulatory Efficiency • Efficiency of the circulation can be assessed by taking pulse and blood pressure measurements • Vital signs – pulse and blood pressure, along with respiratory rate and body temperature • Pulse – pressure wave caused by the expansion and recoil of elastic arteries – Radial pulse (taken on the radial artery at the wrist) is routinely used – Varies with health, body position, and activity • Systemic arterial BP is measured with auscultation – A sphygmomanometer is placed on the arm superior to the elbow – Pressure is increased in the cuff until it is greater than systolic pressure in the brachial artery – Pressure is released slowly and the examiner listens with a stethoscope • • • • – The first sound heard is recorded as the systolic pressure – The pressure when sound disappears is recorded as the diastolic pressure Normal is 90-120/60-80 mm Hg Affected by age, sex, weight, race, mood, socioeconomic status, and physical activity Hypotension – systolic pressure is below 90 mm Hg, can also occur from sitting or laying too long and quickly rising Hypertension – condition of sustained elevated arterial pressure of 140/90 or higher – can be caused by fever, physical exertion, and emotional upset – Chronic hypertension can be caused by diet, obesity, age, race, heredity, stress, smoking, arteriosclerosis, and endocrine disorders – Chronic elevation is a major cause of heart failure, vascular disease, renal failure, and stroke Heart • Location – located within the thoracic cavity in the region known as the mediastinum – Left of the midline, flanked on both sides by the lungs – Superior of diaphragm – Anterior to the vertebral column, posterior to the sternum – pointed apex is directed toward the left hip and rests on the diaphragm at the level of the fifth intercostal space – broader base, from which the great vessels emerge, points toward the right shoulder and lies beneath the second rib • Pericardium – a double-walled sac of serous membrane around the heart composed of: – A superficial fibrous pericardium for protection – A deep two-layer serous pericardium which produces lubricating fluid which allows frictionless environment for beating heart • parietal layer lines the internal surface of the fibrous pericardium • visceral layer or epicardium lines the surface of the heart • separated by the fluid-filled pericardial cavity • Pericarditis – inflammation of the pericardium; results in decrease in the amount of serous fluid; causes pericardial layers to bind & stick to each other, forms painful adhesions that interfere with heart movements • Heart Walls – composed of three layers: 1. Epicardium – outside visceral layer; protection 2. Myocardium – thick bundles of cardiac muscle tissue twisted into ringlike arrangements; forms the bulk of the heart; responsible for pumping action (contracts) 3. Endocardium – thin, glistening sheet of endothelium that lines the heart chambers; continuous with endothelium of blood vessels External Heart: Major Vessels of the Heart (Anterior View) • Vessels returning blood to the heart include: – Superior and inferior venae cavae – Right and left pulmonary veins • Vessels conveying blood away from the heart: – Pulmonary trunk, which splits into right and left pulmonary arteries – Ascending aorta (three branches) – brachiocephalic, left common carotid, and subclavian arteries External Heart: Major Vessels of the Heart (Posterior View) • Vessels returning blood to the heart include: – Right and left pulmonary veins – Superior and inferior venae cavae • Vessels conveying blood away from the heart include: – Aorta – Right and left pulmonary arteries Chambers, Valves, and Vessels • Heart is a double pump consisting of four hollow chambers – two atria and two ventricles each chamber is lined with endocardium which helps blood flow smoothly • Superior left & right atria – receiving chambers; not important in pumping activity of heart; contract and empty blood into the ventricles • Interatrial septum – divides atria longitudinally • Inferior left & right ventricles – discharging chambers; pumps of the heart; propels blood out of the heart and into circulation • Interventricular septum – divides ventricles longitudinally • Double pump consisting of: 1. right side – works as pulmonary circuit pump receives oxygen-poor blood from veins of body through the superior and inferior venae cavae and coronary sinus and pumps it out through the pulmonary trunk pulmonary trunk splits into the right and left pulmonary arteries, which carry blood to lungs, where oxygen is picked up & carbon dioxide is unloaded oxygen-rich blood returns to left side of heart through 4 pulmonary veins 2. Left side – systemic circulation blood returns to left side of heart from pulmonary veins and is pumped out of heart into the aorta to supply all body tissues supplies nutrient-rich blood to all body organs oxygen poor blood is returned to the right atrium through the superior and inferior venae cavae walls of left side are thicker than those of right ventricle because it must pump blood over much longer pathway through body Pathway of Blood Through the Heart and Lungs • Right atrium tricuspid valve right ventricle • Right ventricle pulmonary semilunar valve pulmonary arteries à lungs • Lungs pulmonary veins left atrium • Left atrium bicuspid valve left ventricle • Left ventricle aortic semilunar valve aorta • Aorta systemic circulation Cardiac circulation – flow of blood through vessels in the myocardium of heart • Left and right coronary arteries – main coronary vessels; arise from aorta • Each artery forms many branches to deliver oxygen & nutrients to cells of heart wall and to collect wastes from cells; become compressed when ventricles contract & fill when ventricles relax • Myocardium is drained by cardiac veins, which empty into coronary sinus, which empties into right atrium • Valves – allow blood to flow in only one direction through the heart chambers; 4 valves – 2 types • 1. Atrioventricular, or AV valves are located between the atrial and ventricular chambers on each side; prevent backflow into the atria when ventricles contract left AV valve – bicuspid or mitral valve – consists of two cusps chordae tendineae – “heart strings” – anchor cusps to walls of ventricles so that they can’t be pushed up into atria papillary muscles secure chordae tendineae to ventricular walls right AV valve – tricuspid valve – has three cusps 2. semilunar valves – guards bases of large arteries leaving ventricular chambers; both have three cusps; open when ventricles contract; closed when ventricles relax to prevent blood from reentering heart - pulmonary semilunar valves – located between right ventricle and pulmonary artery - aortic semilunar valves – located between left ventricle and aorta • Mild leaks may be heard as a heart murmur; when a valve does not close tightly (incompetent), a swishing sound will be heard as blood flows backwards through a partially open valve; forces heart to pump and repump same blood, heart weakens and fails • Valvular stenosis – valve flaps become stiff, often because of repeated bacterial infections (endocarditis); compels heart to contract more forcible than normal, heart weakens and fails • Valves may be replaced with synthetic valve or valve from a pig heart • Angina pectoris – when heart beats at very rapid rate, myocardium may receive inadequate blood supply because relaxation periods (when blood is able to flow to the heart tissue) are shortened results in myocardium being deprived of oxygen which results in crushing chest pain myocardial infarction (heart attack or coronary) may occur as ischemic (deprived of blood) heart cells die Conduction system of the Heart may be controlled in two ways 1. Nerves from autonomic nervous system act to decrease (parasympathetic nervous system) or increase (sympathetic nervous system) heart rate depending on which division is activated 2. Intrinsic rhythmicity - cardiac muscle cells can contract spontaneously and independently from central nervous system stimulation nodal tissues - specialized cardiac muscle tissue which coordinates contractions composed of specialized tissue much like a cross between muscle and nerve tissue Parts of intrinsic conduction system • Sinoatrial (SA) node - located in the right atrium; tiny cell mass which has highest rate of depolarization in the whole system starts each heartbeat and sets pace of whole heart; generates impulses about 75 times/minute often called the pacemaker • atrioventricular (AV) node - located at junction of the atria and ventricles; delays impulse approximately 0.1 second from atria until contraction is complete • • atrioventricular bundle (bundle of HIS) - receives impulses from AV node; located in septum Bundle branches - located in the interventricular septum; receives impulses from AV bundle and passes them on to Purkinje fibers • Purkinje fibers - spread impulses within muscle of ventricle walls results in “wringing” contraction of the ventricles that begins at the apex and moves toward atria; effectively ejects blood superiorly into large arteries leaving the heart • Heart block results in the atria and ventricles beating at different rates atria and ventricles are separated from one another by “insulating” connective tissue; depolarization waves can reach the ventricles only by traveling through the AV node damage to the AV node can partially or totally release the ventricles from the control of the SA node ventricles beat at their own rate which is much slower • Fibrillation - rapid uncoordinated shuddering of the heart muscle (bag of worms); makes heart totally useless as a pump and is major cause of death from heart attacks in adults usually due to Ischemia - lack of adequate blood supply to the heart muscle • damage to SA node - results in slower heart rate; artificial pacemakers usually installed surgically to correct rhythm • tachycardia - rapid heart rate (over 100 beats/min); may progress to fibrillation • bradycardia - slow heart rate (less than 60 beats/min); not pathological Electrocardiology - recording of electrical currents of the heart • Impulses can be detected on the body surface and recorded with an electrocardiograph (ECG) two or more electrodes are placed on skin over the heart; position of electrodes provides different info. • Typical ECG has three recognizable waves 1. P wave - small and signals the depolarization of the atria immediately before they contract; missing or abnormal wave indicates dysfunction of SA node 2. QRS complex - results from the depolarization of the ventricles; precedes the contraction of the ventricles; abnormal QRS generally indicates heart problems of the ventricles; enlarged R spike indicates enlarged ventricles 3. T waves - results from currents flowing during the repolarization of the ventricles; altered wave may indicate arteriosclerosis or other heart diseases atrial repolarization is generally hidden by the large QRS complex which is being recorded at the same time abnormalities in the shape of the waves and changes in their timing send signals that something may be wrong with the intrinsic conduction system or may indicate a myocardial infarct (present or past) myocardial infarct - area of heart tissue in which heart cells have died • during fibrillation, the normal pattern of the ECG is totally lost and the heart ceases to act as a functioning pump Extrinsic Innervation of the Heart • Heart is stimulated by the sympathetic cardioacceleratory center • Heart is inhibited by the parasympathetic cardioinhibitory center Cardiac Cycle and Heart Sounds • Cardiac cycle - events of one complete heartbeat, during which both atria and ventricles contract and then relax; usually takes about 0.8 sec. • systole - heart contraction • diastole - heart relaxation (these terms always refer to the contraction and relaxation of the ventricles unless otherwise stated) 1. Mid-to-late diastole - complete relaxation pressure in heart is low blood is flowing passively into and through the atria into the ventricles from the pulmonary and systemic circulations semilunar valves are closed AV valves are open atria contract and force blood remaining in their chambers into the ventricles 2. Ventricular systole - ventricular contraction begins & pressure builds up rapidly increasing pressure causes AV valves to close; produces characteristic “lub” heart sound isovolumetric contraction - contraction of ventricle when both valves are shut; blood volume in the ventricle is not changing semilunar valves open when pressure in heart is higher than pressure in large arteries leaving the heart atria are relaxed and begin filling with blood 3. Early diastole - ventricles relax pressure in ventricles begins to drop as ventricle relaxes semilunar valves snap shut (prevents backflow of blood from arteries into ventricles); produces characteristic “dub” heart sound isovolumetric relaxation - AV and semilunar valves are shut and ventricles are expanding; volume is not changing when pressure in ventricles drops below pressure in atria, AV valves open and ventricles fill with blood Cardiac Output – amount of blood pumped out by each side of the heart in 1 minute • Stroke volume (SV) – volume of blood pumped out by a ventricle with each heartbeat increases as the force of ventricular contraction increases • cardiac output (CO) CO = Heart rate (HR) x SV CO = HR (75 beats/min) x SV(70 ml/beat) CO = 5250 ml/min • Average adult blood volume is about 5000 ml; entire blood supply passes through the body once every minute Regulation of stroke volume • Starling’s law of the heart – the critical factor controlling stroke volume is how much the cardiac muscle cells are stretched just before they contract • More stretching = stronger contraction • More venous return = more stretching • Anything that increases the volume or speed of venous return also increases stroke volume and force of contraction • Severe blood loss or very rapid heart rate decreases venous return which decreases stroke volume causing the heart to beat less forcefully Regulation of Heart Rate – may be influenced temporarily by the autonomic nerves, and by various chemicals, hormones, and ions • Sympathetic division of autonomic nervous system stimulate the SA and AV nodes and the cardiac muscle itself to beat more rapidly allows blood to reach body cells during periods of stress, excitement, or exercise (brings more oxygen and glucose) • Parasympathetic nerves slow and steady the heart when demand declines during non-crisis times • Epinephrine – mimics sympathetic nerves • Thyroxine – increases heart rate • Electrolyte imbalances pose threat to heart low blood calcium = depress heart high blood calcium (hypercalcemia) – prolonged contractions; heart may stop entirely • Physical factors influence hart rate age – fetus = 140-160 beats/min gender - females = 72-80 beats/min males = 64-72 beats/min increased body temperature = increased heart rate (fever, exercise) • Congestive heart failure – condition in which the heart is nearly “worn out” due to age or hypertensive heart disease, the heart is depressed so that circulation is inadequate to meet tissue needs; progressive reflects weakening by coronary artherosclerosis, persistent high blood pressure, or multiple myocardial infarcts death due to suffocation (fluid in lungs) or complete heart failure digitalis – drug which simulates parasympathetic nerve; slows and steadies the heart, resulting in a stronger heartbeat Developmental Aspects of the Heart • Fetal heart structures that bypass pulmonary circulation – Foramen ovale connects the two atria – Ductus arteriosus connects pulmonary trunk and the aorta Age-Related Changes Affecting the Heart • Sclerosis and thickening of valve flaps – occurs where stress of blood flow is greatest (mitral valve) – results in heart murmurs • Decline in cardiac reserve – aged heart less able to respond to both sudden and prolonged stressors that demand increased output; sympathetic control less efficient, HR becomes more variable & there is a decline in max HR – less of a problem if physically active • Fibrosis of cardiac muscle – cardiac cells die & are replaced with fibrous tissue; heart stiffens & is less efficient; decreased stroke volume; stiffened nodes result in conduction problems (arrhythmias) • Atherosclerosis – leads to heart attack and stroke; accelerated by inactivity, smoking, stress; diet is more important contributor than age