Ampicillin vs. E.Coli: Who's the Real Winner?
advertisement

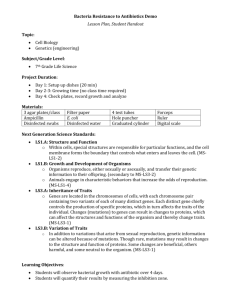
Lisa Michelle Hathaway Ampicillin vs. E.Coli: Who’s the Real Winner? Purpose • The purpose of this experiment was to get a better understanding of how the bacteria, Escherichia Coli reacts to the frequent use of antibiotics and how it affects the bacteria’s long term resistance. I became interested in this experiment after reading about the new super bugs that are antibiotic resistance and how they are gaining force. The information gained in this experiment will help others understand how the overuse of antibiotics may lead to the growth and multiplication of a new population of resistant bacteria. Problem • The excessive use of antibiotics has resulted in bacteria developing a resistance and then immunity to the antibiotics rendering the antibiotics no longer effective. This is leading to the growth and multiplication of a new population of resistant bacteria also known as “Super Bugs”. In this project I set out to test how the bacteria Escherichia Coli (E. coli) is affected by frequent and repeated use to the antibiotic ampicillin and what resistance it develops. Hypothesis • The higher the concentration of the antibiotic Ampicillin used against the bacteria Escherichia Coli (E.Coli) the faster it will develop a resistance to it when exposed to repeated doses of the Ampicillin. Variables • Independent variable: The concentration of the antibiotic Ampicillin used. • Dependent variable: The size of the inhibition zone which is free from bacteria. • Constants: The same Agar solution, same Ampicillin, same Petri dishes same room and environmental controls. • Control: Experiment was preformed with one Petri dish of E. Coli in the Agar Solution with no added Ampicillin Solution. Research : E.Coli • Escherichia coli commonly abbreviated as E. coli is a Gram-negative or rod-shaped bacterium that is commonly found in the lower intestine. Most E. coli strains are harmless, but some can cause serious food poisoning in humans. The harmless strains are part of the normal flora of the gut, and can benefit their hosts by producing vitamin K, and preventing the establishment of pathogenic bacteria within the intestine. E. coli. related bacteria constitute about 0.1% of gut flora, and fecal-oral transmission is the major route through which pathogenic strains of the bacterium cause disease. Cells are able to survive outside the body for a limited amount of time. The bacterium can also be grown easily and inexpensively in a laboratory setting, and has been intensively investigated for over 60 years. E. coli is the most widely studied prokaryotic model organism, and an important species in the fields of biotechnology and microbiology, where it has served as the host organism for the majority of work with recombinant DNA. Research: Ampicillin • Ampicillin is a beta-lactam antibiotic that has been used extensively to treat baterial infections since 1961. Ampicillin demonstrated activity against Gram-negative organisms such as influenza, E.Coli, coliforms and Proteus. Ampicillin was the first of a number of broad spectrum penicillin subsequently introduced by Beecham. Ampicillin is part of the amino penicillin family and is roughly equivalent to its successor, amoxicillin in terms of spectrum and level of activity. It can sometimes result in reactions that range in severity from a rash and many people had allergic reactions such as anaphylaxis. However, as with other penicillin drugs, it is relatively non-toxic and adverse effects of a serious nature are encountered only rarely. Research: Super Bugs • A superbug is a term used to describe a strain of bacteria that is resistant to most prescribed antibiotics. These emerging strains of bacteria can be pretty frightening, since treatments for infection are usually very limited. The following are examples of several super bugs already know to exist. Staphylococcus aureus ( “Staph”) manifests itself in many ways, but is probably most famously known as “flesh-eating bacteria”. For many years, penicillin and methicillin were considered excellent treatments for Staph infections. Strains of Staph that are resistant to methicillin were first observed in hospitals and other healthcare facilities. Tuberculosis, also known as “consumption”, is a disease that is acquired by inhalation into the lungs, where it can cause disease and can spread to other organs in the body. Prior to the discovery of antibiotics, tuberculosis was untreatable. However, even with the widespread use of antibiotics that began in the 1940s, multidrug-resistant tuberculosis (MDR-TB) has emerged and is a leading cause of death, particularly among HIV-infected individuals. MDR-TB is caused by strains of Mycobacterium tuberculosis that are resistant to at least the antibiotics isoniazid and rifampicin Enterococcus faecalis and Enterococcus faecium are found in the bowel and female genital tract and can cause urinary tract infections, blood infections, and meningitis. Enterococci can cause fatal infections in individuals with compromised health, such as infants and the elderly. Several strains of drugresistant enterococci have emerged in the last 30 years, including those that are resistant to penicillin, vancomycin, and linezolid. Streptococcus pneumoniae is a common cause of ear infections in children, meningitis, systemic infection, and pneumonia. Strains that are resistant to penicillin and other penicillin-like antibiotics have increased over the last 30 years. Research: Antibiotic Resistance • Antibiotic resistance is a type of drug resistance where a micro-organism is able to survive exposure to an antibiotic. While a spontaneous or induced genetic mutation in bacteria may confer resistance to antimicrobial drugs, genes that confer resistance can be by conjugation, transduction, or transformation. Therefore a gene for antibiotic resistance which had evolved via natural selection may be shared. Evolutionary stress such as exposure to antibiotics then selects for the antibiotic resistant trait. Many antibiotic resistance genes reside on plasmids, facilitating their transfer. If a bacterium carries several resistance genes, it is called a superbug or super bacterium. The increasing prevalence of antibiotic-resistant bacterial infections seen in clinical practice stems from antibiotic use both within human medicine and veterinary medicine. Any use of antibiotics can increase selective pressure in a population of bacteria to allow the resistant bacteria to thrive and the susceptible bacteria to die off. As resistance towards antibiotics becomes more common, a greater need for alternative treatments arises. Antibiotic resistance therefore poses a significant problem. Research: Inhibition Zone • The inhibition zone is an area around a paper disk or colony of bacteria where no other organisms are growing. For example, when the growth of bacteria susceptible to the antibiotic is inhibited. Typically several million bacterial cells are spread on the agar plate, and if their growth is inhibited, a clear "zone of inhibition" is observed around the antibiotic impregnated disc. If the bacteria are resistant to the antibiotic, a confluent "lawn" of growth is observed. To tell if it is an inhibition zone, it starts with the microbe distributed across the entire plate. If nothing is added to the plate, each microbe will grow, and produce a new microbe by cell division. After this happens for a while (1-3 days depending on the temperature), the agar will get a cloudy appearance because of all of the microbial growth and cell divisions. If no growth occurred in a small area of agar, this area would remain clear. Materials • • • • • • • • • • • • • • • • 15 Petri dishes with an agar solution in them 15 disinfected swabs 1 bottle of disinfected water 1 hole puncher 4 Test tubes 1measuring cylinder 1 digital weighing scale 1 beaker of water 1 forceps 1 marker 1 stirring rod 100mg of Ampicillin E Coil Bacteria Filter Paper 1 Inoculating needle, looped end Access to a room and ability to control the temperature at a constant 78 degrees. Procedures • • • • Prepare 18 Petri dishes using an agar solution and store in a refrigerator. Bring 3 of the Petri dishes to room temperature before the start of experiment. Label the Petri dishes 1mg, 3mg and 5mg. Prepare and label the antibiotic mixture. Labeled one 1mg - 1mg of ampicillin is mixed with 10ml water Labeled one 3mg - 3mg of ampicillin is mixed with 10ml water Labeled one 5mg - 5mg of ampicillin is mixed with 10ml water • • • Mix 10ml of E Coli bacterium culture with 40ml water in the 4th test tube. Rinse the inoculation needle using the disinfected water. Dip it into the test tube containing the bacteria culture and swipe it gently over the agar surface of the 3 Petri dishes. Punch out circular plates of filter paper using a hole puncher. Label the circular plates of filter paper 1mg, 3mg and 5mg. Pick up the filter paper plates using the forceps and dip them into the ampicillin solution according to the labeled concentrations. Place the filter paper plates at the center of the Petri dish according to their labels and cover them. Keep the dishes in a cool dry place for the bacteria to incubate for 4 days. After 4 days, measure the diameter of this area around the filter paper in the inhibition zone. Collect the surviving bacteria along the border of the inhibition zone by using a swab and use it to prepare the bacteria culture needed for subsequent experiment. Repeat 5 more times. Measure the diameter of the inhibition zone for the repeated labs and record the results. • • • • • • • • • Photos 1st Generation 2nd Generation 3rd Generation 4th Generation 5th Generation 6th Generation Live E.Coli Bacteria Agar Solution Data Ampicillin Concentration 1st 2nd generation generation 3rd generation 4th generation 5th generation 6th generation 15.5 11.5 7.5 1mg 24 22.5 19 3mg 22.5 21.5 20.5 18 16.5 12.5 5mg 21.5 21 20 19 18 17 Graph Ampicillin Concentration and Bacterial Resistance 30 25 20 1st Generation 2nd Generation 3rd Generation 15 4th Generation 5th Generation 6th Generation 10 5 0 1 mg 3 mg 5 mg Results • • • • • • In the first generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 24mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 22.5mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 21.5mg. In the second generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 22.5mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 21.5mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 21mg. In the third generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 19mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 20.5mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 20mg. In the fourth generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 15.5mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 18mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 19mg. In the fifth generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 11.5mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 16.5mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 18mg. In the sixth generation set of the experiment the Perti dish with 1mg of Ampicillin had an inhibition zone of 7.5mg. The Perti dish with 3mg of Ampicillin had an inhibition zone of 12.5mg. The Perti dish with 5mg of Ampicillin had an inhibition zone of 17mg. Conclusion • I was able to conclude from the results that my hypothesis was incorrect. The higher dose of Ampicillin killed off the E.Coli faster but the E.Coli did not develop a resistance to the stronger dose quicker. The experiment proved that the smaller dose allowed for the E.Coli to become resistant to the antibiotic quicker than the higher level doses did. The bacteria was able, at the lower dose after repeated use of the antibiotic to develop a resistance and in turn caused the antibiotic to become less effective in eliminating the bacteria faster than at the higher dose. However the high dose did mimic the same results of resistance just at lower numbers. In conclusion of these results antibiotics should be avoided unless absolutely necessary. The experiment proves that overuse of antibiotics causes resistance in turn causing the antibiotic to become ineffective. Newer and stronger antibiotics need to be developed to combat the bacteria that have developed a resistance but these antibiotics will be more expensive and with unknown side effects. Abstract • Antibiotics are among the most frequently prescribed medications in today’s world of medicine. Antibiotics cure disease by killing or injuring the bacteria. I set out to get a better understanding of how the bacteria, Escherichia Coli reacts to the frequent use of the antibiotic Ampicillin. I became interested in this topic after researching the new “Super Bugs”, (bacteria that has become resistant to antibiotics) and how they are currently gaining force. My experiment centered around how quickly the E.Coli would develop a resistance to the antibiotic. I hypothesized that the higher the concentration of the antibiotic Ampicillin used against the bacteria Escherichia Coil the faster it would develop a resistance to it when exposed to repeated doses of the Ampicillin. I preformed six generations of experiments with three concentration levels of the antibiotic to determine the rate of resistance it would develop. The data I collect from the results of six generations of experiments showed that the bacteria died quicker the higher the dose of antibiotic but also that the higher the dose of antibiotic the slower the bacteria was in developing a resistance. My hypothesis was incorrect in the end as the lower the dose of Ampicillin given the quicker the E.Coli was able to develop a resistance to it. However, now people can know these results and avoid the overuse of antibiotics to avoid more strains of bacteria becoming resistant to antibiotics and the need for stronger and more harmful antibiotic to be developed to combat them. Bibliography & Acknowledgements • Rosenberg, S, “Inhibition of Mutation and Combating the Evolution of Antibiotic Resistance”, Research Article. Published May 10, 2005. http://www.plosbiology.org/article/info:doi/10.1371/journal.pbio.00 30176 • WebMD, “What is an E.Coil Infection”, E.Coil Infections. Created September 2005, Updated June 14, 2010. http://www.webmd.com/a-to-z-guides/e-coli-infection-topicoverview?page=2 • • • • • • • World Health Organization, “Antimicrobial Resistance", Key Facts on Antimicrobial Resistance. Created and Copy-written 2011. http://www.who.int/mediacentre/factsheets/fs194/en/ Wikipedia, “Ampicillin,” Mechanism of Action. Created 1998, Updated September 25, 2011. http://en.wikipedia.org/wiki/Ampicillin Centers for Disease Control and Prevention, “Antibiotic Resistance”, Questions and Answers. Created June 30, 2009, Updated September 10, 2010. Http://www.cdc.gov/getsmart/antibiotic-use/antibiotic-resistancefaqs.html • I would like to acknowledge the following people for their help and support in the completion of this science project: Mrs. Garciga, Mr. Brezina, Jeannette Hathaway and Ann House.