Factors affecting respiratory function
advertisement

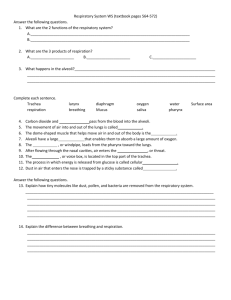
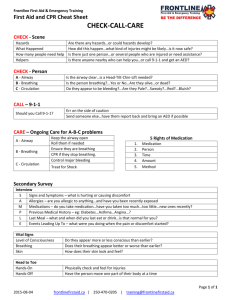
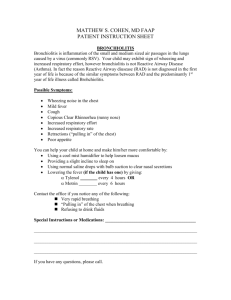
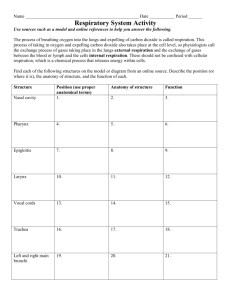
Oxygenation Dr. Suad Jassim Key Terms; Alveoli; clusters of small air-sac, its wall made up of single –cell layer of squamous epithelium allows for gas exchange with capillaries covering it, the average adult has more than 300 million alveoli. Perfusion; is the process by which oxygenated capillary blood passes through body tissue. Atelectasis; is a closure of alveoli as a result of reduced ventilation which causing lung collapsed. Bradypnea; slow respiration rate. Bronchodilator; is an agent that expand the opening of the airway passage. Cilia; which are a microscopic hairlike projection, propel trapped material &accompanying mucus toward the upper airway & removed by cough. Diffusion; is the movement of gas (O2 &CO2) from area of high concentration or pressure in (alveoli) to low (blood in the capillaries) Dyspnea; it`s difficulty in breathing. Incentive spirometry ; an instrument provides visual reinforcement for deep breathing to patients. Hyperventilation: is abnormal rapid deep breathing. Hypoventilation; decreased rate or depth of air movement in the lungs. Hypoxia ; is a condition in which an inadequate amount of oxygen is available to cell. Surfactant; a phospholipids cells ,reduces the surface tension between the moist membrane of the alveoli so preventing from collapse. endotracheal intubation ;is the passage of a tube through the mouth , pharynx and larynx into the trachea to establish an airway . Anatomy & physiology of respiration; The respiratory system performs its function through : 1. pulmonary ventilation, 2. respiration& 3. perfusion. Essential Factors of normal respiratory function; 1. 2. 3. the integrity of airway system to transport air to& from the lungs. A properly functioning alveolar system in the lungs to oxygenate venous blood & to remove co2 from the blood. A properly functioning cardiovascular &hematological system to carry nutrients &wastes to & body cells . Structure of respiratory system; 1. Airway, it is a pathway of transport & exchange of o2 &co2,it begins at the nose & ends at the terminal bronchioles, it divided into upper & lower. 2. Upper airway, composed of the nose, pharynx, larynx & epiglottis, its main function; is to warm, filter &humidify inspired air. 3. Lower airway or(tracheobronchial tree) , it includes, trachea, segmental bronchi, Terminal Bronchioles it`s major function are; 1. 2. 3. 4. conduction of air mucociliary clearance production of surfactant. helps in protection of underlying tissue from irritation& infection. 5- lungs & thoracic cavity are lined with a serous membrane called pleura, it consist of two layers; • visceral pleura, covers the lung. • parietal pleura, lines the thoracic cavity. (intrapleural pressure always negative pressure) . Regulation of respiration; Respiration is controlled by tow methods; • Neural ,medulla in the brain stem, above the spinal cord. • Chemoreceptors in the aortic arch& carotid bodies, are sensitive to same arterial blood gas level &blood pressure &can activate medulla. Factors affecting respiratory function; • Level of health, acute & chronic illness may affect respiratory function, such as MI disease, or kidney failure. • Age – related developmental consideration. • Medication affect function of respiratory system , such as opioids, which depress the medullary respiratory center, resulting in decrease rate & depth of respiration. Factors affecting respiratory function cont. • Lifestyle, activity levels & habits can affect a persons respiratory status, exercise (e.g. aerobic , walking, swimming) &cigarette smokinghabits. • Environment, air pollution & occupational exposure to asbestos, silica or coal dust, can lead to chronic pulmonary disease. • Psychological health, individuals responding to stress may sigh exhibit hyperventilation. Nursing process; Assessment; Focused oxygenation guide Usual pattern of respiration Do you have any allergy? What relief measures do you use? Medication Are you taking any medication to breathing? Health history Do you have any, heart, lung or breathing condition? Recent changes Have you noticed any changes in your breathing (cough, wheezing, pain)? Do you have chest pain ? Do you have a respiratory infection & what type? Life style & environment Do you smoke? Are you exposed to respiratory irritant in your work place? cough How much & how often do youcough? Are you exposed to dust? Or fumes? How are you treating the cough? Assessment cont. sputum Do you cough up & spit sputum? What color ?is it with blood tinged? Chest pain Do you have pain with breathing? Where is the pain? Is the pain worse with inspiration or expiration? Dyspnea Is it constant remittent or related to any activity? How dose it affect your daily activity? fever Have you had pneumonia recently? Do you have any contact with people who have tuberculosis? Do you have night sweat? Common diagnostic test: 1- Pulmonary function studies; it includes a group of tests used to evaluate patients with respiratory problem &evaluate pulmonary status & detect abnormalities. 2- spirometry; it measures the volume of air in liters exhaled or inhaled by the patient over time. Common diagnostic test cont. 3- Peak Expiratory Flow Rate (PEFR);IT refers to the point of highest flow during forced expiration which reflect changes in the size of pulmonary airways. 4- pulse oximetry; is a noninvasive technique that measure the arterial oxyhemoglobin saturation (SaO2 or SpO2) of arterial blood, pulse oximetry, is useful for monitoring patients receiving oxygen therapy, & detecting those at risk of hypoxia. 5- Thoracentesis; is a procedure of puncturing the chest wall &aspirating pleural fluid for diagnostic& therapeutic purposes. Diagnosing; oxygenation Nursing diagnosis Related factor Ineffective airway clearance Thick yellow secretion, fever, fatigue, poor nutrition, dehydration. Impaired gas exchange Smokes one pack per day, works with asbestos in auto factory, has had a cold for 7 days . Ineffective breathing patteren Anxiety about cardiac surgery. • • • • • • Other N. D alteration in respiratory function; Activity intolerance related to shortness of breath, Anxiety related to feeling of suffocation Acute pain r/t to pleural inflammation Acute confusion r/t impaired ventilation Imbalance nutrition; less than body requirement r/t to difficulty breathing. Ineffective health maintenance r/t smoking. Implementation; 1. Promoting optimal function , teaching patients with respiratory disorder about pollution free environments is important, & negative effect of smoking. 2. Promoting comfort; • Positioning, proper position for the patient that allows free movement of the diaphragm & expansion of the chest, dyspnea patients & orthopnea are comfortable with FOWLERS P. • Maintaining adequate fluid intake, to loosen the secretion, dinking about (1.9 -2.9 L) of clear fluid. • Providing humidified air, dry air causing irritation of respiratory passage. 3. Promoting proper breathing ; instruct the patient to take deep breath enough to move the bottom ribs, & using incentive spirometry. 4. Promoting & controlling coughing; a cough is a cleansing mechanism of the body to clear the airway . • Non productive cough, is the dry cough. • Productive cough , cough producing secretion or (sputum). 5. Performing chest physiotherapy; it loosen &mobilize the secretion, it includes; percussion, vibration, and postural drainage. 6. Administering inhaled medication; it administered to open narrowed airways, such as; -bronchodilator, it is used to liquefy the thick secretion (mucolytic) , or to reduce inflammation in airway (corticosteroids). -Nebulizer, a liquid medication used in the machine. -metered – dose inhaler; such as, albuterol , theophylline & corticosteroids. Providing supplemental oxygen; The flow rate of oxygen, measured in liters per minute, determine the amount of oxygen delivered to the patient. Providing supplemental oxygen supply via oxygen therapy, can increase the amount of O2 transported in the blood, it considered a medication so it must be ordered by health care provider. Precautions for oxygen administration; 1. Avoid open flames in the patients room. 2. Place “ NO SMOKING “ signs oxygen in use, in places near patient room. 3. Check the electrical equipment used in the room, such as, electric bell cords, razor, radios & suctioning equipment. 4. Avoid wearing & using fabric that build up static electricity. 5. Avoid smoking. Oxygen delivery system; methods Amount Delivered FiO2 Priority of N interv. Nasal cannula Low flow 1 L/min=24% 2L/min=28% 6L/min=44% -check frequently the pores in the pt. nares -patient can speak & eat during oxygenation. Simple mask Low flow 6-10L/min=35-60% -monitor pt. frequently to check mask placement. Partial rebreather mask Low flow 6-15L/min=70-90% -Set flow rate to remains two thirds full during inspiration. -keep reservoir bag free of twist or kinks Nonrebreather mask Low flow 6-15L/min =60-100% -Maintain flow rate so the reservoir bag collapses slightly during inspiration . -monitor SaO2 with pulse oxymeter. Venturi mask High flow 4-10L/min=24-55% -requires careful monitoring to verify FiO2 at flow rate ordered. Endotracheal tube; it is a polyvinylchloride airway that is inserted through the nose or the mouth into trachea, using a laryngoscope as a guide.it used ; To administer O2by mechanical ventilation. To suction secretion from airway easily. Tracheostomy; it is a tube inserted to replace endotracheal tube, to provide method for mechanical ventilation of the patient, or to remove tracheobronchial secretions. Administering cardiopulmonary resuscitation; it is the combination of mouth- to mouth breathing, which supplies oxygen to the lungs & decompressed chest, it described in terms of ABCDs of basic life support. Airway, Breathing , Circulation & Defibrillation Reference: • Taylar L..“ FUNDAMENTALS OF NURSING” 7TH. EDITION , Walters comp.2008,page 1347- 14. • online litrature.