Patient Care Rounds
advertisement
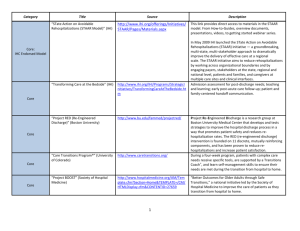
Ideal Patient Care Across the Continuum: Reducing Preventable Readmissions April 17 IHS Forum Peg Bradke RN MA St. Luke’s Hospital Director of Heart and Vascular Services Where We Have Been • Engaged Cross Continuum Teams • Condition focused • Learned about patients who are readmitted – By condition, 3 readmissions in 180 days • Used IHI Change Package for hospitalbased transitions • Learned to see and solve at the front line – Started to see from another care site perspective Where We Are Going 2012 Clinical Priorities Clinic Quality Patient Experience Hospital Home Health Adherence to Diabetes Bundle Reduce Readmissions Reduce Acute Hospitalization Improve Press Ganey Scores Improve HCAHPS Scores Improve HHCAHPS Scores 2011 Results Improved Transitions and Coordination of Care Reduction in Avoidable Rehospitalizations Post-Acute Care Activated Evidencebased Care in Community Care Settings (Better Models of Care) Alternative or Supplemental Care for HighRisk Patients * * Additional Costs for these Services Transition from Hospital to Home Patient and Family Engagement Cross-Continuum Team Collaboration Health Information Exchange and Shared Care Plans Co-designing Processes to Improve Transitions Hospitals • Perform an enhanced assessment of post-hospital needs • Provide effective teaching and facilitate enhanced learning • Ensure posthospital care follow-up • Provide real-time handover communications Office Practices • Provide timely access to care following a hospitalization • Prior to the visit: prepare patient and clinical team • During the visit: assess patient and initiate new care plan or revise existing plan • At the conclusion of the visit: communicate and coordinate ongoing care plan Home Care Skilled Nursing Facilities • Meet the patient, family caregiver(s), and inpatient caregiver(s) in the hospital and review transition home plan • Assess the patient, initiate plan of care, and reinforce patient selfmanagement at first post-discharge home care visit • Engage, coordinate, and communicate with the entire clinical team • Ensure that SNF staff are ready and capable to care for the resident patient’s needs • Reconcile the Treatment Plan and Medication List • Engage the resident and their family or caregiver in a partnership to create an overall place of care • Obtain a timely consultation when the resident’s condition changes Analysis of Results to Date • Reducing readmissions is dependent on highly functional cross-continuum teams and a focus on the patient’s journey over time. • Explicit focus on patient and family-centered work. • Importance of engaged Executive Leadership and Physician Leadership. • Improving transitions in care requires co-design of transitional care processes among “senders and receivers”. Frontline clinicians and staff involvement in developing the process improvements. • Stories are as important as data. • Providing intensive care management services for targeted high-risk patients is critical. • Reliable implementation of changes in pilot units or pilot populations requires 18 to 24 months. • Information Technology design is part of the work. Barriers to Improving Care Transitions and Reducing Rehospitalizations • Cost of copayments for medications and follow-up visits. • Lack of coverage for home health services if patients did not meet regulatory requirements. • Lack of reimbursement for transitional care services such as post-discharge phone calls, coaches and dedicated clinicians to provide extra support for patients and family caregivers. • Limitations of the electronic medical record to capture and transmit information. • Access to physician offices for follow-up visits. • Complexity of patients with multiple co-morbidities. • Challenges to completing reliable medication reconciliation. • • • • How, exactly, does IHS deliver on the Triple Aim? Align providers with a common quality agenda Use Analytics to identify at-risk patients for clinical intervention Design a care management infrastructure to follow the patient across a highly integrated provider network into all care settings Deliver comprehensive care aimed to attain and maintain health in the outpatient setting PLA-MLA Joint Meeting: February 2012 Linking the Patient Experience and Reducing Readmissions Patient/Family as Full Partner • Partner with patient/family in the way they want to be • They will speak up more if involved • Look for the patient/family clues • With their input look at what you specifically do at each transition • The patient is not discharging from the Army – they need a transition (K. White) Key Changes to Improve the Transition from Hospital to Home 1. Perform an Enhanced Assessment of Post-Hospital Needs 2. Provide Effective Teaching and Facilitate Enhanced Learning 3. Ensure Post-Hospital Care Follow-Up 4. Provide Real-Time Handover Communications Understanding of the comprehensive assessment of the post-discharge needs of patients • Streamline paperwork for nurses and enhance the work environment to free up time for nurses to spend more time with patients (TCAB changes: move laptops to patient rooms; admission nurse; bedside change-of-shift report) • Front-line nurses complete a more comprehensive assessment of home-going needs (need to specify the openended questions); bring this information plus “what the patient is worried about” to daily Care Rounds • How best to use white boards in patient rooms to assess comprehensive needs of patients? • Develop standardized processes for getting information from family caregivers and community providers Patient and family caregiver understanding and comprehension of clinical condition, plan and self-care at home • Create standard process to involve family caregivers • Ensure that all nurses, hospitalists and residents are competent to facilitate health literacy teaching sessions (Ask Me 3 and Teach Back) • Incorporate patient teaching into routine daily processes such as the bedside change-of-shift report • Change documentation fields in EMR from “what has been taught” to “what is the patient’s understanding of……?” Post-acute Follow-up Care • No universally agreed-upon risk assessment tools; may be difficult to mitigate some medical and social risks • Continue to assess utility of assessing patient’s understanding of home care and meds (using Teach Back); look at agenda of Patient Care rounds • Appropriate and timely FU care is dependent on availability and payment for services • Plan post-discharge follow-up care taking into consideration assessed needs and capabilities of the patient and family caregiver; • Chronic Disease Management/ Advance Medical Team Proposed Agenda for “Patient Care Rounds” 1. What are the goals/reasons for this admission? Are the health care team’s goals and the patient/families’ goals in synch? 2. What needs to happen during this hospitalization? What are the criteria for the discharge readiness? 3. What is the likelihood that this patient will be readmitted in 30 days? Why (predictions re: potential problems)? 4. What post-acute care plan should be put in place to meet the patient’s level of activation and to mitigate potential problems? 5. Activate and communicate real-time post-acute care plans to patients, family caregivers and community providers Handover Communications • Co-design of communication and information needed for next level of care • After care summary • Agenda for f/u office visit • Utilizing Interact tools for Nursing Facilities • Utilizing Health Coaches/Navigators • Determining who is the most appropriate individual to make the follow up calls. • Don’t confuse information with communication Scale-up and Spread • Spread: Taking a system or intervention and replicating it in an independent site – Replication without new learning or structural changes. – Ex: A pilot unit at a hospital implements changes to reduce patient injury from falls >> successes are shared with nurses in an educational forum and changes are promoted and spread hospital-wide • Scale-up: The progressive design of a system of interrelated parts; moving from one setting to a larger setting and then an even larger setting within an interrelated system – Expect new learning and structural changes to achieve results at scale. – Ex: A pilot unit at a hospital successfully implements TeachBack as the standard approach to patient education >> TeachBack is an annual core competency for all nurses and residents in the hospital and EHR has fields where nurses and doctors document “patient understanding…” Source: API and IHI Retreats Critical Capabilities for Care Redesign Include: • Cross-continuum participation and alignment • The development and use of standardized tools and compatible information infrastructure • Horizontal Leaderships and executive sponsorship; and engaged physicians • Effective external and internal learning Scale up changes cannot be a “project”, they must become the new way to do work, built into the culture 20 Reducing Readmissions with Integrated Chronic Care Disease Management Vicki Wildman, RN, MSN, Edu Iowa Health Home Care Cause of Crisis: Poor Management “Patients can undo a month’s worth of expensive and intensive care just going home and going about their normal routines.” John Charde, MD VP Strategic Development, Enhanced Care Initiatives, Inc (April 2006) Before Informed, Activated Patients Prepared Prepared Practice Practice Team Team •Motivation •Information •Skills •Confidence •Patient information •Decision support •Resources Home-Based Chronic Care Model High Touch Delivery Specialist Oversight Self-Management Support Technology After Lesson’s Learned Commitment Education Competency performance testing Hardwiring evidence-based practices Future Opportunities • Expansion of the curriculum cross continuum • Sustaining the education, training, and competency • Evidence based medicine implementation project • Hardwiring best practices related to chronic conditions • Individual employee outcome scorecards The Future • Rehospitalizations are frequent, costly and many are avoidable; • Successful pilots, local programs and research studies demonstrate that rehospitalization rates can be reduced; • Individual successes exist where financial incentives are aligned; • Improving transitions state-wide requires action beyond the level of the individual provider; systemic barriers must be addressed; • Leadership at the provider, association, community and state levels are essential assets in a state-wide effort to improve care coordination across settings and over time.