Ch. 1 Introduction to Designing a Rehabilitation Program

Ch. 1
Introduction to Designing a
Rehabilitation Program
Introduction
• Designing the program can be a challenge
• What is an appropriate starting point?
• ROM, strengthening, stretching?
• WHERE DO I START???????
• Any good rehab program begins with a thorough EVALUATION
• This can be through the HOPS format: history, observation, palpation, special tests
Medical History
• Key component of the eval
• Must be comprehensive
• Past and current dysfunctions
• In an athletic setting, this is usually part of the pre-participation physical exam
Subjective History
• Most important part of initial eval
• Allows you to rule out many problems
• Onset of pain
• Location
• Mechanism of injury (MOI)
• Patient goals
• Previous treatments
• Activities that aggravate and alleviate pain
• Past history/social history
• Keep patient focused on immediate problem
• No tangents
• Mechanism-guide to activities to avoid
• Avoid aggravating activities in early stages
• Activities that alleviate pain (modalities and meds) may be included as a part of the rehab process
• Past history-investigate additional contributors
• Social history – guides home program
• Previous treatments-what has and hasn’t worked
• Goals-importance of the patient
Objective
• -visual inspection
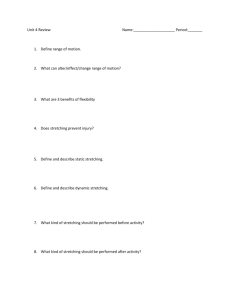
• Range of motion
• Strength testing
• Special tests
• Proprioceptive tests
• Neurological exam
Visual Inspection
• Postural assessment
• Gait biomechanics
• Functional performance biomechanics
Posture
• Assessed in all cases to determine abnormalities contributing to patient’s dysfunction
• Direct contributors- factors that cause the problem (forward head posture in a patient with cervical disk herniation)
• Indirect contributors-factors that contribute but are not the main contributor (rounded shoulders in a throwing athlete with impingement)
Gait and Functional Performance
Biomechanics
• Overuse injuries of the lower extremity
• Based on patient’s activity
Additional Information
• Deformity
• Discoloration
• Swelling
• Atrophy
• Skin conditions
• Wounds
• scars
Palpation
• Determines involved tissues
• Soft and bony tissues
• Point tenderness
• Deformity
• Crepitus
• Rigidity
• Heat
• Muscle spasm
Range of Motion
• Active and Passive
• Quality and quantity
• Presence of pain, faulty mechanics, substitution patterns, muscle weakness
• Cyriax’s rule
• Measured with a goniometer
Flexibility Testing
• Information regarding the “cause of the cause”
Joint Mobility Testing
• Hypo versus hypermobility
• Addressed through taping and bracing or surgical repair
• Hypomobility – managed through ROM exercises, stretching, joint mobilization and dynamic splinting
Strength Testing
• Manual muscle testing
• MMT’s performed isometrically
• Ability to test a single muscle
• Disadvantage – you are only evaluating strength at one point
Strength Testing
• Resistive range of motion testing
• Allows patient to move through a portion of the range against an external resistance
• Tests are more functional
• However, pain can be generated by contractile or inert tissues
• Does not allow for isolation testing
• Helps assess muscle fatigue with repeated tesing
• Avoid if AROM causes pain
Special Tests
• Testing of joints or other structures
• Reveals pain, instability, tissue tightness or neurological symptoms
• Can determine the used of weight bearing or non-weight bearing activities in the early stages of rehab
• More helpful in providing the diagnosis than guiding the rehab program
Proprioceptive Testing
• Unconscious or conscious awareness of body or joint position
• “Where you are in space”
• Measured by balance testing
• Single leg stance, wobble boards, foam cushions, foam rollers
Neurological Examination
• CNS and PNS function
• Dermatome testing
• Myotome testing
• Reflex testing
Myotome Assessment
• MMT’s for specific muscles
• Focuses on weakness rather than pain
• Decreased strength in the absence of a muscle injury is an indicator of spinal nerve root or
CNS dysfunction
Reflex Testing
• Spinal nerve root or CNS injury
• Measured using a 3-point scale
• 0- no reflex
• 1-hyporeflexive
• 2-normal
• 3- hyperreflexive
Joint Specific Testing
• Girth measurements
• Limb-length assessments
Girth Measurements
• Using a tape measure
• Comparing two joints
• Provides info regarding tissue edema, muscle hypertrophy and atrophy
• Edema – compression and elevation
• Hypertrophy – muscle imbalance
• Atrophy-need for strengthening in the plan
Limb-Length Measurements
• Small differences are common
• Differences greater than 7mm have been shown to alter gait mechanics and predispose athletes to overuse injuries
• Congenital abnormalities in bone growth
• Faulty bone healing
• Could lead to a heel lift or foot orthoses as a part of the treatment plan
Clinical Pearl of Wisdom
Although the Diagnosis is one of the most important parts of the evaluative process, it does not describe the actual cause
Determining the Diagnosis
• Important for medical decoding and 3 rd party reimbursement
• ICD-9 code – developed by the World Health
Organization, is used by insurance companies to reimburse (get paid) for rehabilitation services
• CPT codes-Current Procedural Terminology, must match with the diagnosis in order to be reimbursed
• SOAP format
• Subjective
• Objective
• Assessment
• Plan
Documentation
Subjective and Objective
• Paint a picture of the patient for other health professionals to follow
Assessment
• Made up of three parts
– Diagnosis
– Problem list
– Treatment goals
Diagnosis
• Most difficult for students or inexperienced clinicians
• The result of all your questions and tests
Formulating a Problem
• Compilation of all the abnormal findings
• From the subjective and objective part of the eval
• Each one added to problem list within the assessment portion of the note
• Each one representing a “cause of the cause”
Treatment Goals
• Guides treatment plan
• Justification for continued treatment
• Based on problem list
• Divided into short term and long term
Formulating a Comprehensive
Treatment and Rehabilitation Plan
• Each problem is paired with a goal
• Ex: Pain- modalities, rest, joint mobilization
– Edema – modalities, compression, elevation
– Postural problems-patient education, biofeedback
• Stretching
• Strengthening
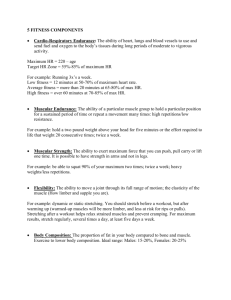
• Muscular endurance
• Bracing and taping
Problems con’t
• Gait abnormalities
– Orthotics
– Taping and footwear modification
– Stretching and strengthening
Problems
• Functional abnormalities
– Patient education
– Activity modification
– Equipment modification
– Biofeedback
– Stretching and strengthening
Problems
• Decreased AROM and PROM
– Thermotherapy modalities
– Range of motion
– Stretching
– Joint mobilization
Problems
• Decreased AROM (normal PROM)
– Neuromuscular stimulation
– Active or active assistive range of motion
– Strengthening
– Muscular endurance
• Decreased flexibility
– Thermal modalities
– stretching
Problems
• Decreased joint play
– Thermotherapy modalities
– Range of motion
– Stretching and joint mobilization
• Decreased muscular strength/atrophy
– Neuromuscular stimulation
– AROM and AAROM
– Strengthening
– Muscular endurance
Problems
• Excessive joint laxity/hypermobility
– Immobility, bracing, taping
– Strengthening and proprioception
• Decreased proprioception/balance
– Proprioceptive exercise
• Neurological deficits
– Address the cause of the neurological dysfunction
Problem
• True limb-length discrepancy
– Heel lift, orthoses, footwear modification
• Apparent leg-length discrepancy
– Stretching and strengthening
– Muscle energy techniques
– Grade III and IV joint mobilization
Incorporating Therapeutic Modalities
• Cryotherapy
• Thermotherapy
• Electrotherapy
• Ultrasound
• Iontophoresis
• Soft tissue mobilization
Re-evaluating the Patient
• Just as important as the initial eval
• Done at each appointment
• Multiple times during the session
• Don’t add more than two exercises per session
Critical Thinking
• How do your findings from the medical history impact the design of the treatment and rehabilitation plan?
Critical Thinking
• How will your goals and treatment plans change when rehabilitating a collegiate golfer with medial epicondylitis versus a factory worker with the same condition? How will your approach vary in motivating your patient to reach their goals?
Critical Thinking
• What other individuals will you include in the evaluation and rehabilitation process of the golfer and factory worker to identify the
“cause of the cause”?
Critical Thinking
• A patient comes to you with a complaint of heel pain that increases with activity. Would your assessment of the patient differ according to age? If so, how? What could be some different conditions based on age
(adolescent vs. senior)?