Off-the-Field Evaluation
advertisement

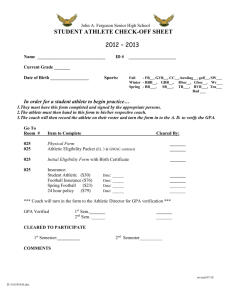
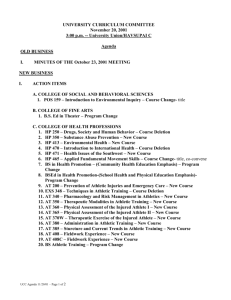
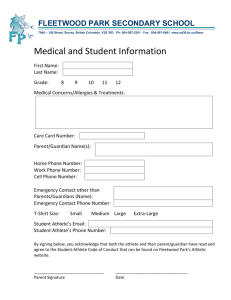
Off-the-Field Evaluation Athletic Medicine I Objectives ● Know: The organs located in each abdominopelvic quadrant. o Difference between clinical and medical dx. o The order in which evaluations are conducted. o The specifics of HOPS. o What different ROMs are testing for. o How to document injuries. o Evaluation of Sports Medicine Injuries ● Four distinct evaluations o o o o Pre-participation On-the-field Off-the-field Progress (during rehabilitation) Diagnoses ● Athletic Trainers offer a clinical diagnosis. o Accurately identifies the pathology of injury, the limitations and possible disabilities associated with a condition. ● Physicians offer a medical diagnosis. o o Use of X-rays, MRIs, CT scans, blood tests, etc. Ultimate determination of a patient’s physical status. Basic Knowledge Requirements ● Athletic trainers must have a thorough knowledge of human anatomy and its function, as well as the sport and its demands. Anatomy ● Surface Anatomy ● Abdominopelvic Quadrants o Quadrants ● Musculoskeletal Anatomy o o o Bones Landmarks Muscles Abdominopelvic Quadrants ● URQ o o Liver Gallbladder ● ULQ o o o o Spleen Stomach Liver Kidney Abdominopelvic Quadrants ● LLQ o Colon ● LRQ o Appendix Activity ● We must understand what demands specific activities place on the body. o Football vs. swimming vs. tennis. Descriptive Assessment Terms ● Etiology: Cause of disease/injury. ● Mechanism: Mechanical description of the cause. ● Pathology: Structural and functional changes that result from injury. ● Sign: Indicator of disease (you can see it). ● Symptom: Change that indicates injury (athlete describes it). ● Diagnosis: Name of a specific condition. ● Prognosis: Predicted outcome of injury. ● Sequela: Condition resulting from disease or injury. Off-the-Field Injury Eval Process ● HOPS o o o o History Observation Palpation Special Tests History ● MOST critical aspect of the evaluation. ● Information obtained: Mechanism o Chief complaints o Pain location, character, duration, variation, aggravation, distribution, intensity, and course. o Existing conditions. o History: 10 Questions ● ● ● ● ● ● What’s going on? How did it happen? When did it happen? What did you hear? What did you feel? Where does it hurt? ● What does it feel like? ● On a scale of 1-10, how bad is the pain? ● Has this happened before? ● Have you done anything for it? Observation ● Usually done while taking a history. ● Things to look for: Obvious deformity o Limp; abnormal movements o Posture o Facial expression o Edema; redness; bruising o Asymmetries o Abnormal sounds o Palpation ● Two types: o o Bony Can reveal abnormal gap in joint, swelling on a bone, joints that are misaligned, or abnormal protuberances associated with a joint or bone. Soft tissue Swelling, lumps, gaps, muscle tension, temperature variations. Special Tests ● Designed to detect specific pathologies. ● To decide which tests to perform, take into account all information up to this point. ● Types of special tests: Movement assessment Manual muscle testing o Neurological assessment o Joint stability o Functional performance o o Special Tests: Movement Assessment ● Active Range of Motion (AROM) o Athlete moves joint with no assistance. ● Passive Range of Motion (PROM) o Athletic trainer moves joint with no assistance from the athlete. ● Resisted Range of Motion (RROM) o Athlete moves joint through range against resistance applied by athletic trainer. Special Tests: ROM ● Tells us what types of structures may be involved. Pain with AROM, PROM and RROM: Most likely bone or ligament. o Pain with AROM and RROM, but not PROM: Most likely muscle. o Special Tests: Manual Muscle Testing ● Tests muscular strength ● Places athlete in different positions to test different muscles. ● Athlete holds body part in specific position while the athletic trainer provides resistance. Special Tests: MMT Scale 1: Unable to move affected body part. 2: Unable to hold affected body part against gravity. 3: Able to hold the position against gravity. 4: Able to hold position against gravity and minimal resistance. 5: Able to hold position against gravity and maximal resistance. Special Tests: Neurological Exam ● Five major areas: o o o o o Cerebral Cranial nerve Cerebellar Sensory Reflex ● You only need to do the first three if you suspect a head injury. Special Tests: Sensory Testing ● Dermatome: Area of skin innervated by a single nerve. ● Myotome: Muscle or group of muscles innervated by a specific nerve. ● Need to test: Superficial sensation o Superficial pain o Deep pain o Special Tests: Joint Stability ● Special tests used to test ligaments and cartilage. o o i.e. Lachman’s for ACL; McMurray’s for meniscus. https://www.youtube.com/watch?v=oFWjwxJJmm Q Injury Documentation Injury Documentation ● For documenting what we see, there is a specific way we must document. ● Why do we document? o o See any changes that are occurring. Document the treatment that we did. SOAP Notes ● Used to document injuries. ● Subjective (everything the athlete tells you). ● Objective (everything you see feel and measure) ● Assessment (Diagnosis) ● Plan (what are you going to do?) Subjective Pt. is complaining of sharp pain in L ankle. Recalls “rolling” it in a soccer game yesterday when she stepped on an opponent’s foot. Pt. states that pain is 5/10 with walking and 2/10 at rest. Pt. was not able to finish the game. Pt. reports feeling a pop in ankle; did not hear it. Reports spraining ankle last soccer season. After current injury, went home and iced and elevated. Objective Observation: No obvious deformity. Moderate edema over L lateral malleolus. Discoloration distal to lat. mallelous and near phalanges. Walking with obvious limp. Palpation: TTP over distal L lat. malleolus and sinus tarsi. No bone tenderness. No palpable deformity, crepitus. Mild temperature difference when compared bilat. Mild palpable edema. Objective ● ROM o AROM: Plantarflex: Full when compared bilat., mild pain. Dorsiflex: Full when compared bilat. Inversion: Diminished when compared bilat., moderate pain. Eversion: Full when compared bilat.; mild pain o PROM o RROM o Manual Muscle Test Plantarflex: 5/5 Dorsiflex: 5/5 Objective/Assessment/Plan ● Special Tests: o o o o (-) Bump test (-) Compression test (+) Anterior drawer for pain; mild laxity (+) Talar tilt for pain ● Assessment: L Grade 2 ATFL Sprain ● Plan: RICE ~48 hours; begin ROM exercises when pain subsides. Progress Notes Done periodically during rehabilitation.