SVT
advertisement

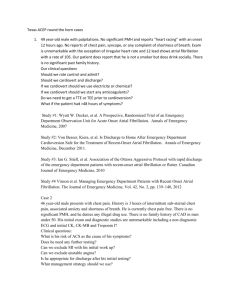
Supraventricular Tachycardia Teresa Menendez Hood, MD FACC Presbyterian Hospital of Dallas Supraventricular Tachycardias • AV nodal reentry tachycardia • AV reentry tachycardia - the WPW(WolffParkinson White) Syndrome • Atrial flutter • Atrial Fibrillation • Atrial Tachycardia • Sinus Tachycardia and Sinus Node Reentry Atrial Fibrillation • Unorganized, very rapid electrical foci in the atria • No contraction of the atria as a whole • In order to protect the ventricles, the AV node blocks most of the atrial impulses from conducting through to the ventricles, thus protecting the ventricles • Controlled rate = ventricular rate < 100 beats/min • Uncontrolled rate = ventricular rate > 100 beats/min Atrial Fibrillation • Characteristics of atrial fibrillation: – – – – – Ventricular rhythm is usually irregularly irregular Average ventricular rate is 160 – 180 beats/min on no drugs No P waves seen QRS interval is usually normal (narrow) If see discrete P waves…think of MAT • This clinical scenario is a cardiac or pulmonary patient in the ICU. Thought to be due to a hyperadrenergic state and CCB and helpful. Atrial Fibrillation – Control the rate using IV calcium channel blockers or beta-blockers…IV dig does not work – If the A-fib is chronic (> 48 hours) • Chemical cardioversion after a period of anticoagulation • Electrical cardioversion only after anticoagulation Atrial fibrillation accounts for 1/3 of all patient discharges with arrhythmia as principal diagnosis. 6% PSVT 6% PVCs 18% Unspecified 4% Atrial Flutter 9% SSS 34% Atrial Fibrillation 8% Conduction Disease 10% VT 3% SCD Data source: Baily D. J Am Coll Cardiol. 1992;19(3):41A. 2% VF Classification of Atrial Fibrillation The 3 Ps • Permanent - Conversion to sinus rhythm not possible • Persistent - Capable of being converted to sinus rhythm • Paroxysmal - Converts spontaneously to sinus rhythm Gallagher MM and Camm AJ Clin Cardiol 1997;20:381 AF: Anticoagulation - General Points • AF most common significant rhythm disorder – Prevalence: 1.5%-3% of patients in their 60s 5%-7% of patients in their 70s 15% of patients in their 80s • AF most potent common risk factor for stroke – Relative risk = 5 • Patients with AF can be stratified according to risk of stroke Feinberg WM e al. Arch Intern Med 1995;155:469 Wolf PA et al. Stroke1991;22:983 AF: Anticoagulation - General Points • Anticoagulation (INR 2.0 - 3.0) can reduce risk of stroke by 2/3 1,2 • Aspirin has little effect on risk of stroke due to AF 3 1 Hylek EM and Singer DE. Arch Intern Med 1994;120:897 2 Hylek EM et al. New Engl J Med 1966;335:540 3 The Atrial Fibrillation Investigators. Arch Intern Med 1997;157:1237 1/98 medslides.com 9 Risk Factors for Stroke in AF Risk Factor Prior stroke Age Hypertension Diabetes Relative Risk (multivariate) 2.5 1.4 (per decade) 1.6 1.7 Absolute Risk Age < 65 years and no risk factors, “lone AF”: 1%/yr. All others: 3.5%-8+%/yr lowered to ~1.5%/yr by warfarin The Atrial Fibrillation Investigators Arch Intern Med 1994;154:1449 1/98 medslides.com 10 Elective Cardioversion of AF Anticoagulation • Cardioversion appears to raise risk of embolism – 1%-5% emboli within hours to weeks – Anticoagulation well before and after greatly reduces risk • Standard guideline for electrical or drug cardioversion – INR 2 - 3 for 3 weeks before; and – INR 2 - 3 for 4 weeks after NSR – IF AF < 2 days’ duration, no anticoagulation Laupacle A et al. Chest 1995;108 Prystowsky EN et al. Circulation 1996;1262 Adequate Rate Control • At office visits – Apical (not radial) heart rate (sitting): 80 / min • On 24-hour Holter monitor – Goal: average hourly heart rate 80 / min • Exercise testing – Inadequate: 85% age-predicated maximum heart rate in stage I (Bruce) or 3 min of exercise – Digoxin alone will never control the rate unless the patient has intrinsic AVN conduction system disease Tachycardia - Induced Cardiomyopathy • Chronic tachycardia in otherwise structurally normal heart as the sole cause of developing ventricular dysfunction • Can follow any chronic cardiac tachyarrhythmia Fenelon G et al. Pacing Clinical Electrophysiol 1996;19:95 Preference for Acute Cardioversion • DC Cardioversion • i.v. Ibutilide • Other: – Oral Flecainide – Oral Propafenone – i.v. Procainamide Preference for Acute Cardioversion i.v. Ibutilide • • • • • • • QTc 460 msec Short duration of AF (<30 days) No clinical CHF. K and Mg levels OK Anesthesia risk (e.g., COPD) Patient preference Acute efficacy - flutter (63%), fib (31%) Caution: risk of polymorphic VT (8%) Stambler BS, et al. Circulation 1996; 94:1613-1621 Long term treatment • Beyond the scope of this talk • Guided by patient symptoms • AFFIRM trial did not show any benefit of NORMAL SINUS RHYTHM versus AFIB with rate control in patients who had minimal symptoms • Ablation for AFIB is guided by patients’ symptoms and drug failures Atrial Flutter • Usually a single, irritable foci in the atria (right) • AV node protects the ventricles by blocking some of the atrial impulses (decremental conduction) • P waves take on a “sawtooth” appearance and are called F waves or flutter waves – Atrial rhythm and ventricular response are usually regular – Atrial rate 250-350 beats/min. Ventricular rate varies depending on the number of impulses the AV node is blocking – No P waves or PR interval – QRS normal width or with aberrancy Atrial Flutter • Treatment: – Same as atrial fibrillation but often harder to slow the ventricular rate – Long term treatment is ablation and NOT drugs! RF Ablation of Atrial Flutter • Atrial flutter involves a macro-reentry circuit within the right atrium. • Critical areas of conduction within the right atrium are necessary to sustain atrial flutter. • RF ablation of conduction within such critical sites (most commonly the inferior vena cava-tricuspid valve isthmus) abolishes atrial flutter in 85% of cases. Cosio FG. Am J Cardiol. 1993;71:705-709. Diagram of Atrial Flutter Circuit Within Right Atrium Cosio FG. Am J Cardiol. 1993;71:705-709. Inferior vena cava tricuspid valve isthmus Differential Diagnosis of Wide-Complex Tachycardia • VT • SVT with aberrancy (atrial fibrillation/flutter)-i.e. BB Block • Antidromic AV reentry –i.e. antegrade via WPW accessory pathway • Atrial fibrillation, atrial flutter, atrial tachycardia, or AV nodal reentry in setting of WPW with rapid conduction down accessory pathway that is activated as a bystander-I.e. not an integral part of the circuit. Narrow QRS Wide QRS - BBB (Aberrant conduction) AVN A B HB RB LB Wide QRS - VT Wide QRS - Preexcitation (Conduction via AP) C D Akhtar M. In:Zipes and Jalife. Cardiac Electrophysiology from Cell to Bedside. 1990:636. Key ECG Signs • • • • • Atrial activity QRS configuration R-R cycle length Aberrant ventricular conduction Response to vagal maneuvers An EKG you will see on the Boards……….. • This has been on every Board exam I have ever taken. Please do give AVN blockers for this!When in doubt, treat as if you thought this was VT. Atrial Fibrillation with Preexcitation Electrocardiographic Differentiation of VT vs. SVT with Aberrancy • Clinical history – if the patient has had an MI in the past?…it is VT until proven otherwise • AV dissociation • QRS morphology • QRS axis • Fusion beat • Capture beat A-V Dissociation, Fusion, and Capture Beats in VT V1 E ECTOPY F C FUSION Fisch C. Electrocardiography of Arrhythmias. 1990;134. CAPTURE ECG Distinction of VT from SVT with Aberrancy Favors VT Favors SVT with Aberrancy Duration RBBB: QRS > 0.14 sec. LBBB: QRS > 0.16 sec. < 0.14 sec. < 0.16 sec. Axis QRS axis -90° to ±180° Normal ECG Distinction of VT from SVT with Aberrancy Favors VT Morphology Precordial concordance If LBBB: V1 duration > 30 ms S wave > 70 ms S wave notched or slurred V6: qR or QR If RBBB: V1: monophasic R wave qR If triphasic, R > R1 V6: R < S Favors SVT with Aberrancy R wave R < R1 Sinus Tachycardia • Sinus node is still the pacemaker, but the rate is accelerated for some physiologic reason: – Rhythm is regular – Rate > 100 beats/minute – P wave, PR interval, and QRS complex are all normal • Can look like Sinus Node Reentry – paroxysmal and less than 160 BPM; incidence of ~10% of all PSVT’s Sinus Tachycardia • Treatment: – Alleviate the underlying cause-anemia, pheo, hyperthyroid… – Could be inappropriate ST- a type of autonomic dysfunction with HR consistently above 120 Paroxysmal Supraventricular Tachycardia • Repeated episodes of tachycardia with an abrupt onset and ending (paroxysmal) • SVT is usually due to a reentry mechanism. • Could also be to abnormal automaticity or triggered activity but would have more of a warm-up and cool-down effect. Supraventricular Tachycardia • Characteristics: – Rhythm is regular – Rate 140-220 beats/minute – P waves may be buried in the QRS or the T wave and may differ in morphology from sinus P waves – PR and QRS interval may be normal or prolonged. Supraventricular Tachycardia – Long term treatment is with ablation in most cases – Response to vagal maneuvers is helpful – Acutely: meds used to decrease the rate or convert the patient to NORMAL SINUS RHYTHM: Adenosine, IV Verapamil or Esmolol – If patient is unstable: • Electrical cardioversion Pearls • ST depression is common during SVT and is not a marker of serious ischemia • If the first dose of Adenosine does not work? Then add 6mg to the amount and give again (6-1218)…do not repeat the same dose. (If given via central line then 3-6-9-12) • Adenosine may put the patient in AFB…be ready to cardiovert. Classification of PSVT • Short R-P – AVRT(slow-fast) – AVNRT • Long R-P – Atypical forms of the AVNRT (fast-slow)or AVRT(usually will have a negative P wave in 2,3,avf) – Most atrial tachycardias, SNRT – PJRT Atrial Tachycardia • Reentry, Automaticity and Triggered (rare) Activity have been found as causes • Rates 120 to 150 • Usually 1:1 AVN conduction and persistence despite AV block • Usually from right atria (Ring of Fire) • Can be seen as an incisional tachycardia from previous surgery..i.e. ASD repair • May see remission in children so do not attempt ablation until adulthood. AVN reentry • Most common from of PSVT • Can occur at any age and more common in women • Typical form is down the slow and up the fast pathway in the AVN region. • Adenosine is the drug on choice for conversion. Need to be careful about pts with reactive airway disease and those on persantine. It may not work in pts with theophylline. WPW • Pre-excitation affects 3/1000 patients on routine screening….not all develop PSVT • Antegrade (delta wave) and retrograde conduction • More common in men • Most present in young adulthood • 15% incidence of AFIB • Multiple pathways in 10%