Life Threatening EKGs Encountered in the Outpatient Setting
advertisement

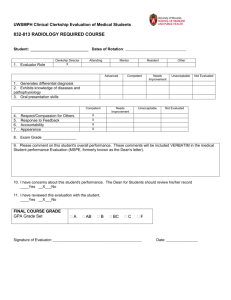
Teaching Students from Jan to June: Reaching the Unreachable Sundip Patel, M.D. Drew Nyce, M.D. Council of Residency Directors Meeting April 3rd 2012 Atlanta, Georgia Outline • • • • • • Qualifications LCME Rules & Unreachable Why it’s Important to Reach the Unreachable Key Motivational Factors for the Unreachable Methods to Reach the Unreachable Do’s and Don’ts Qualifications • Cooper AAMC Graduation Survey Data Poor Fair Good Excellent Our Clerkship 0.0 25.0 50.0 25.0 National Avg 6.0 13.9 36.7 43.4 Our Clerkship 3.8 11.5 26.9 57.7 National Avg 6.1 13.7 35.0 45.2 Our Clerkship 3.6 3.6 32.1 60.7 National Avg 4.5 11.5 33.1 51.0 Our Clerkship 0.0 2.3 34.9 62.8 National Avg 4.3 11.3 32.4 51.9 Our Clerkship 0.0 12.0 12.0 76.0 National Avg 4.3 11.1 32.1 52.6 Year 2007 2008 2009 2010 2011 LCME & Unreachable LCME ED – 17 “Educational opportunities must be available in a medical education program in multidisciplinary content areas (e.g., emergency medicine, geriatrics)” • Where in the curriculum? • How is it covered? LCME & Unreachable • ED – 17 – Requirement not met in Surgery / Medicine clerkships • Limited EM exposure • H&P on patient in ED not enough – Easiest way for med school to fulfill • Required EM clerkship • All students must rotate • Hence the “Unreachable Students” LCME & Unreachable • EM rotations – 36% mandatory, 14% selective in 20071 – 65% clerkships have EM rotation only in 4th yr 1 – In 2012 • These numbers likely higher • If not a required EM clerkship, just wait…… • More Unreachable students 1 Wald DA, Manthey DE, Kruus L, et al. The state of the clerkship: a survey of Emergency Medicine clerkship directors. Acad Emerg Med. 2007; 14: 629-634. LCME & Unreachable ED – 10 “must include behavioral and socioeconomic subjects…” – Exposure to suicidal, psychotic, drug abuse pts – Exposure to homeless, inability to pay for meds – How do students meet this requirement? Just have them see the first pt on overnight ED shift LCME & Unreachable • Summary – EM clerkship meets many LCME requirements – If not required EM clerkship, just wait….. • All students • Jan to June • Unreachable students – Engage? – Personalize? – Motivate? Why Reach out to the Unreachable • Need to answer to your dean, chairman – Clerkship stats • • • • • Organization Educational experience Patient care Faculty / resident educators Dreaded “Additional Comments” – All stats affected by “Unreachable” students Why Reach out to the Unreachable • You are ALWAYS showcasing your EM program – Mistreatment of “Unreachable” student • Creates bad reputation for your dept • Turns off home students interested in EM • Has this really happened?? Why Reach out to the Unreachable • We’re educators, Darn it!! – We enjoy educating everyone • Even those not going into EM – We’ve never shown preferential treatment to students going into EM – We want to create a reputation that we enjoy educating everyone Key Motivational Factors for Unreachable Students • Fulfill a required rotation • Fulfill a required rotation • Fulfill a required rotation and………………….. • Where to go on vacation? Key Motivational Factors for Unreachable Students • Things you need to remind students to motivate them – Procedures • Fulfill medical school requirements • Practice procedures will be doing as interns – Opportunity to see things may never see again • Peds student seeing elderly patients • IM student seeing surgical abdomens • Pathology student seeing living patients Key Motivational Factors for Unreachable Students • Things you need to remind them to engage them – 6 months argument i.e. “You will soon be an intern” • Committing to plans • Working on interpersonal skills – Handling sick patients • 2am on-call page - “Mrs. Smith is really short of breath and doesn’t look good….” • ACLS algorithms Key Motivational Factors for Unreachable Students • How do we motivate & engage the Unreachable? – EM Clerkship Orientation Day – Our orientation is different depending on the time of year • July – Nov orientation (For EM bound students) – Focus on LORs – Additional EM experiences – If deciding late, how to go about the process / visiting rotations Key Motivational Factors for Unreachable Students • Jan – May orientation (geared for non-EM bound students) – Focus on procedures – Completing med school requirements – Obtaining skills to help when they are an intern Methods to Reach the Unreachable • • • • • • Simulation…..with a twist….. Teaching shifts EBM Enrichment Experience Ultrasound Mid-Clerkship Feedback Simulation • Other clerkships focus on small area – Anesthesia – Airways – OB/Gyn – Deliveries • EM sim gives students opportunity to do more – ACLS protocols • Real life, students never run codes • Ability to manage sick pts on own – Medications – Procedures – Learn how to run a team Simulation • Do students love running ACLS protocols? – Yeung CJEM 2010; 12: 212-219 – 2 x 2hr ACLS lectures with 8 hr skills session – Students ranked ACLS training above • Clinical shifts • Supervised shifts (teaching shifts) • Procedural skills lab – ACLS is a hands-on activity that they can apply clinically Simulation • What’s our twist? • Tailor sim experience to student’s interest – Example – Student going into Dermatology • • • • Take septic shock case Have pt with toxic epidermal necrolysis become septic Show images of TEN Benefits – YOU cover septic shock – THEY love it Simulation • Other examples – Optho – globe rupture with trauma sim – Ortho – long bone fxs with trauma sim – Radiology – pregnant trauma • Discuss radiation exposures • Other imaging options – Family Medicine • Sim about end of life • Breaking bad news – Pathology • Nothing you can do for them • Send them to the anatomy lab Simulation • Tailoring sim to student interest – More work / prep on your part – Students have total buy-in – Still covering main topics – Great evaluations Teaching Shifts • We have used for over 7 yrs • Teach 2-3 students on a 6 hr shift • Dedicated faculty member – Does not hear resident cases – Generally does not see pts primarily • More time for education • Directly observe students – Real time feedback – LCME requirement Teaching Shifts • Problems – Need buy-in from faculty worried about RVUs – Need lots of • It works (Cassidy-Smith CJEM 2011; 13: 259-266) – Students – better bedside teaching, rotation – Faculty – more available, quicker dispositions – Residents – increased faculty availability Other Shifts • Besides Teaching shifts – Only 1 student each shift • Constant engagement • No competition for procedures • Can’t hide – One on One faculty interactions • Fast Track • “Broadway” Shift Evidence Based Medicine • LCME ED-6 provide EBM to students • ED provides real scenarios • So many different aspects of EBM – Gold standards – Sensitivity, specificity, NPV – Intention to treat – Applicable to your patient population Evidence Based Medicine • Tailor the EBM to their future interests – Ortho – do open distal tuft fxs need OR washout? – Pediatrics – fever workup in children 8 weeks old? – Surgery – Does morphine prevent an accurate abdominal exam? – Pathology – Will you ever raise your hand in a plane if they ask for a doctor? Evidence Based Medicine • On-line Journal Club – Article posted online – Questions about article also posted online • Design of study, sensitivity, specificity • Strengths, weaknesses • Apply to your patients – Go over the article and questions on test day – Student feedback very positive Enrichment Experience • Optional experience • Student meets with EM faculty member twice in 4 weeks • Must cover the following 1. 2. ECG Module • Clinical Vignettes with ECGs • Questions Enrichment Case • Slow dissection of a case » Pertinent positives and negatives in H&P » Work-up and treatment plans » Interpretation of labs and xrays Enrichment Experience 3. Interesting case selected by the student • • • Student gives oral presentation Discussion of differentials Gives faculty member something new each block 4. EBM presentation • • • 10 min powerpoint presentation Summary of ED case with a question Journal article that answers question Enrichment Experience • Overall good student feedback – Love one-on-one interaction with faculty – Really like ECG module • Problems – Large time commitment by faculty – Initial startup requires time / effort • Creating ECG module • Creating Enrichment Case Ultrasound • No experience on other rotations • Radiology rotation – Read ultrasounds – Don’t do them • Perfect marriage – Disease process – Imaging – Procedure – Patient contact Ultrasound • Could provide ultrasound experience – Integrated into EM clerkship • Pros – Every student gets exposure – Enhances rotation • Cons – Time taken from other aspects of the clerkship – Not enough time to gain ultrasound competence Ultrasound • Solutions – Separate ultrasound rotation • More time to focus on ultrasound techniques • However students not going into EM won’t do it • Another course you need to run – Concentrate on one aspect during clerkship • Pelvic ultrasound for first trimester pregnancies • FAST exams in trauma • Peripheral IV insertion Mid-Clerkship Feedback • • • • Students appreciate feedback Not given well in other rotations Hard to do in 4 weeks LCME requirement Mid-Clerkship Feedback • • • • Wake-up call to students not motivated More detailed the better Solutions to correct deficiencies Example of the feedback at Cooper – Focus on 3 areas • Clinical work • Required patient encounters • Written patient notes Mid-Clerkship Feedback • Feedback on the Feedback Do’s and Don’ts • Do’s • Let them see cases in desired field in a limited basis (Ex – student going into ortho picking up ankle fracture) – If prevent them from seeing cases they’re interested in » Unhappy student » Poor evaluations – If you allow them to focus primarily on those cases » Miss out on true EM experience » Not really an EM rotation » Faculty will be resentful • Need a nice mix Do’s and Don’ts • Do’s – Flexibility in scheduling • Allow students to go to ortho conference, meet with advisor, etc. • However students still need to make up shift • Must meet all requirements Do’s and Don’ts • Do’s – SAME expectations in seeing patients • Don’t lower the bar for what is expected in clinical work • If you lower the bar, students going into EM unhappy • Short-changing these students – Think what they are doing is ok – Will transfer this practice to actual patient care as interns Do’s and Don’ts • Don’t – Cut down shift number Jan-July • • • • Your faculty will pressure you into doing this You may really want to do this Unfair to non-EM student who rotated in July Sends wrong message Do’s and Don’ts • Don’t – Allow faculty to ignore or let non-EM students slide • Don’t allow faculty to send students home early • Don’t allow students – To stop seeing patients early – Shadow residents • Your chairman should support you in preventing this Summary • EM fulfills many LCME requirements • If not required EM clerkship, just wait • Motivations of the Unreachable – Fulfill a requirement – Gain skills to become good house officers • Techniques to Reach the Unreachable – Motivate – Personalize – Challenge Summary Methods to motivate / challenge the “Unreachable” 1. Tailoring Sim to their interests 2. Teaching Shifts 3. EBM • • 4. 5. 6. 7. Shifts On-line journal club Enrichment Experience Ultrasound Mid-clerkship Feedback Can’t reach pathology students……lost cause