Cognitive behavioural approaches to the detection and prevention
advertisement
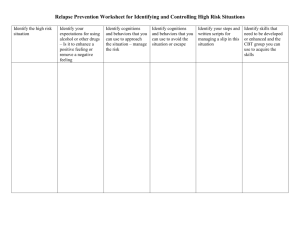
Cognitive behavioural approaches to the detection and prevention of relapse Staying Well After Psychosis II Dr Andrew Gumley Senior Lecturer in Clinical Psychology University of Glasgow & ESTEEM: Glasgow Schedule 09-30 09-45 10-15 10-30 10-50 12-00 12-30 13-30 13-45 14-15 14-35 15-15 15-45 Aims and Objectives Exercise I Rehearsal of Formulation Feedback Coffee Break Prioritising key problematic beliefs and behaviours Exercise II: Generating alternative strategies Lunch Compassionate mind versus rational mind Exercise III: Developing a behavioural experiment Coffee Break Anticipating organisational / service barriers to relapse prevention intervention Planning and action points Discussion and Close Aims This workshop builds directly the skills and themes developed within Workshop 1. Participants will have the opportunity to rehearse, revise and / or develop high level skills in formulation based cognitive behavioural strategies aimed at recovery and staying well after psychosis. By the end of the workshop participants will practice skills in – developing a personal narrative incorporating clients’ experience of psychosis, – use clients’ narrative to support them in exploring key personal themes concerning loss, humiliation, entrapment, fear, threat and shame, – understand how service and staff interpersonal responses might alleviate or intensify clients cognitive, emotional and behavioural reactions to psychosis, – rehearse cognitive behavioural strategies aims at transforming such personal meanings, and – conceptualise systemic interventions aimed at transforming problematic service responses to signs of elevated relapse risk. Workshop methodology Modelling therapeutic process Where possible, exercises conducted within clinical teams to aid dissemination. Exercises are designed to specifically target clinically relevant material. Feedback on needs and strengths of specific exercises. Therapy scenario Th: Pt: Th: Pt: Th: Pt: What do you make of your voices? They’re aliens, they tell me I’m a paedophile, an abuser, its horrific……… What does your doctor make of these voices, what does he think they are caused by? [Pause] He thinks I’ve got schizophrenia. What do you think about that? It can’t be true. That would mean I have an illness, and that would mean these voices come from me……..[Pause] Those things couldn’t come out of my head. Internal, Personal, stable attribution Attributions “Jimmy doesn’t get up cos he’s just being lazy” Expressed Emotion Criticism and hostility Negative self evaluation Psychophysiological arousal Positive Symptoms Relapse and readmission Exercise I Teams Choose patient / client from Tuesday Rehearse formulation – Interpersonal context Family and team attributions / responses – Beliefs – Emotions – Cognitive behavioural strategies Cognitive Interview for Early Signs Establish last episode (or most memorable) Identify key events Prioritise events according to significance to individual Elicit associated memories, images and other cognitions Establish meaning linked to self and self in relation to illness Link event and meaning to cognitive, perceptual and physiological experience Time frame ESTABLISH DATE OF LAST RELAPSE ESTABLISH ONSET OF PRODROME CHOOSE EVENT DURING PERIOD BETWEEN ONSET OF PRODROME AND RELAPSE – – – – Prototypic questions: When talking about your last relapse is there a particular memory that comes to mind? At what point did this occur? Are their other events which come to mind? ESTABLISH TIME LINE FOR EVENTS IN RELATION TO ONSET OF PRODROME AND RELAPSE Hot Cognitions ESTABLISH EVENT ASSOCIATED WITH ‘HOT’ COGNITIONS – Prototypic questions: – Which of these events distresses you most? – If only one of these events occurred which would have been the most upsetting? – Why is that? ELICIT MEMORIES AND IMAGES ASSOCIATED WITH THE EVENT? – – – – Prototypic questions? What was so upsetting about that? Are there thoughts and images which come to mind? Can you describe these? GUIDED DISCOVERY TO ESTABLISH MEANING – What does that event mean to you? – What was the worst thing about that? Linkage ELICIT COGNITIONS RELATED TO SELF, AND SELF IN RELATION TO ILLNESS – What does it say about your illness? – Do you still think that? – How does it make you feel about your illness? LINK EVENT AND MEANING THROUGH COGNITIVE, PERCEPTUAL, AND PHYSIOLOGICAL EXPERIENCE – When you think about that now how do you feel? (probe cognitive, perceptual and physical experience? – What do / did you notice about your thoughts? – What do/ did you notice about your body? FORMULATE AND SUMMARIZE BY LINKING EVENT, INTERNAL EXPERIENCES, BELIEFS AND EMOTIONAL/ BEHAVIOURAL SEQUELAE Therapist Tasks Identify key cognitions Identify key setting events Identify key behavioural strategies Prioritise in relation to – Emotional temperature – Interpersonal impact – Day to day impact Problematic Experiences Attachments, loss, psychosis etc Core Beliefs E.g. I am useless, Others are dangerous Overdeveloped Behaviours Underdeveloped Behaviours Aggressiveness, suspiciousness, self punitiveness Self care and nurturance, affiliation, assertiveness Pivotal Assumptions Related to relapse, adjustment and recovery Capture experiential meanings linked to psychosis and premorbid experiences Assimilation and (over)accommodation Strongly linked to emotion and “hot” cognition Linked to strategic deployment of behavioural strategies Examples If I relapse then my family will be disappointed If people know how I feel then they will laugh at me If I get stressed then I will get unwell If I do not have complete control of my thoughts then I am defective If I seek help then I will be admitted If I show any signs of weakness then they will put me in hospital If I get upset this means I am weak and needy Exercise II Prioritise – One key belief and associated recurring behaviour – Consider carefully the linked associated valued goals and benefits linked to that belief and recurring behaviour – Identify an alternative behaviour that would achieve person’s valued goal without same degree of costs. Rational Mind Looks at the evidence Is scientific, treats thoughts and ideas as theories to be disconfirmed Likes to have several alternatives to choose from Likes to test things and run experiments Does not like to be hasty Knows that knowledge develops slowly Learns from trial and error Weighs advantages and disadvantages Takes a long term view Compassionate mind Has empathy and sympathy Is concerned with growth and reaching potential Is concerned with supporting, healing and listening Is kind and friendly Is quick to forgive and slow to condemn Does not attack but repairs Recognises and accepts imperfection Self worth and self acceptance ore not earned but are unconditional Behavioural experiments Focus on target thought and explore evidence. Identify stimuli and behaviours Identify alternative belief Present rationale for experiment Conduct experiment Discuss results in terms of formulation Specific procedures Identify key target belief – E.g. I am an okay person Operationalise cognition – People are friendly towards me – People smile at me – They use eye contact with me Alternative behaviour to strengthen new belief – Giving eye contact to others, smiling etc Develop a testable prediction. – Go into Safeway, at meat counter smile, say hello. Consider what can go wrong – Person ignores me – They start laughing Exercise III Developing and planning a behavioural experiment – Identify key target belief – Operationalise belief – Alternative behaviour to strengthen new belief – Develop a testable prediction. – What can go wrong. SITUATION Social situations INTRUSIONS Images of being naked Sexual Intercourse Bodily hair METACOGNITIVE APPRAISAL I’m mixed up I’m mentally ill The devil is implanting thoughts in my head PHYSIOLOGY Tension EMOTIONS Disgust, Shame, Fear, Depression SAFETY BEHAVIOURS Avoidance, Rumination, Vigilance Assessment Anxious Thoughts Inventory Metacognitions Questionnaire Collaboratively developed assessment: – Frequency of Intrusions (0-10) – Intrusiveness (0-10) – Dwelling (0-10) – Belief “I am mentally Ill” (0-10) – Dsitress (0-10) Questions What thought would you focus on? How would you explore the thought? What behaviour would you focus on? How is behaviour linked to thought? What alternative belief could you test out? What could you set up with the patient to test out the alternative belief? What are your predictions for this test? Frequency of Intrusions 10 8 6 4 2 0 Days 55 49 43 37 31 25 19 13 7 Frequency 1 Frequency Frequency Intrusiveness 12 10 8 6 4 2 0 Days 55 49 43 37 31 25 19 13 7 Intusiveness 1 Intrusiveness Intusiveness Dwelling Dwelling 6 4 2 0 Days 55 49 43 37 31 25 19 13 7 Dwelling 1 Dwelling 8 Belief Belief 10 Belief 5 Days 55 49 43 37 31 25 19 13 7 0 1 Belief 15 Distress Distress 5 Distress Days 55 49 43 37 31 25 19 13 7 0 1 Distress 10 Pre / Post Assessment AnTI – Social = 28 – Health = 14 – Meta = 23 MCQ – – – – – Positive = 29 Control = 48 Efficiency = 18 Negative = 28 Self Consciousness = 25 AnTI – Social = 10 – Health = 7 – Meta = 8 MCQ – – – – – Positive = 29 Control = 20 Efficiency = 10 Negative = 17 Self Consciousness = 17 Contact: a.gumley@clinmed.gla.ac.uk