Case study-BR
advertisement

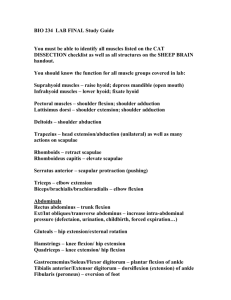
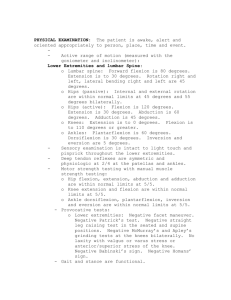
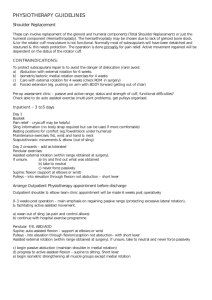
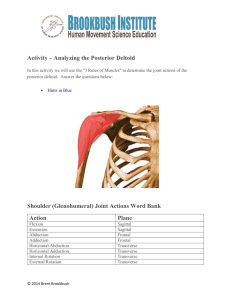
Reverse Total Shoulder Arthroplasty: An Outpatient Physical Therapy Program Using Therapeutic Exercise with Emphasis on Deltoid Strengthening Becky Roberson Introduction Total Shoulder Arthroplasty (TSA) is a widelty accepted operative intervention for many patients who suffer from glenohumeral (GH) pathology such as osteoarthritis, rheumatoid arthritis, rotator cuff tear arthropathy and humeral head fractures. For those patients with a deficient rotator cuff, a traditional TSA has not proven to give the patient the best results due to the altered biomechanics of the shoulder. The Reverse TSA (RTSA) is gaining popularity with this patient population because it takes into account that the patient no longer has a rotator cuff keeping the GH joint in alignment, and is mechanically designed to give advantage to the deltoid muscle as the prime mover of the new shoulder (1). Studies have shown that patients with a RTSA show significantly higher anterior deltoid and upper trapezius activation during abduction and flexion with the use of electromyographic analysis over the control group (2). This suggests that these muscles act to compensate for the lack of the rotator cuff (1). The conventional TSA prosthesis uses the ball in socket mechanics like the natural GH joint would have. When the patient has an intact rotator cuff this design works best to allow the rotator cuff to initiate the rotational movements in the shoulder. The prosthesis for a Reverse TSA uses an opposite approach, where a ball is placed in the glenoid cavity and the humeral head is replaced by a concave socket. This is the design that gives the mechanical advantage to the deltoid muscle as the new prime mover (4). The average weight of the human arm is approximately 5% of the total body weight (3). Using this information, we are able to determine how much strength the patient will need to regain in the deltoid muscle during the rehabilitation process in order to successfully flex and abduct at the shoulder. Using a hand held dynamometer to measure the strength of the deltoid will allow us to see the pounds of strength in the muscle, the goal is to regain equal to or greater than the weight of the arm. Physical Therapy following a total TSA whether conventional or reverse is critical for the recovery of function and to prevent Frozen Shoulder Syndrome. In the early weeks following surgery the patient wears a sling to protect the new shoulder joint. Physical Therapy is initiated at 2 weeks post- surgery with an emphasis on joint ROM. Strengthening is added once the patient is discharged from the sling, which is vital for joint protection and return to function (4). The purpose of this case study is to describe the Physical Therapy treatment plan following a Reverse TSA and to highlight the importance of incorporating deltoid strengthening into that plan. Case Description Patient The patient was a 76 year-old Caucasian male with a large rotator cuff tear to the supraspinatus and infraspinatus muscles with narrowing of the subacromial space, who elected to undergo a right RTSA. The patient was retired and lived at home with his spouse. During the winter he worked part-time as Santa Clause. The patient stated that he was independent in all activities of daily living and driving, did not use an assistive device, and was not at risk for falls. His past medical history included hypertension, deep vein thrombosis, colon cancer, and prostate cancer. His past surgical history included right total hip arthroplasty, colon surgery, tonsillectomy, appendectomy, and fracture surgery. The patient did not smoke or drink. The patient had a significant family history for heart disease, neuropathy, and angina. The patient was cleared to begin Physical Therapy at 4 weeks post- surgery. Examination The following examination was performed by the Physical Therapist in an out-patient setting, 4 weeks after the surgery. Shoulder Flexion Abduction External Rotation Internal Rotation Horizontal Abduction Passive 0/60 Unable 0/25 Belly Unable ROM Active Deferred Uninvolved WNL all MMT Right Deferred Left 5/5 all Shoulder Pain and Disability Index Score: Pre-op 8% Pain Pre op: 1/10 Problems Identified: 1. Limited Shoulder PROM 2. Pain Assessment Impression: Findings consistent with expectations at week 4. Weight: 197 pounds. Estimated weight of right arm: 10 pounds Strength of right deltoid in side-lying with elbow at 90 degrees at week 6: 12 pounds by Hand Held Dynamometer Interventions After examining the patient, the patient and Physical Therapist discussed therapy and patient goals. The following short-term and long-term goals were set and agreed upon by both the therapist and the patient. Short-Term Goals: To be met at 2 weeks. 1. Forward Flexion at 0/125 passively 2. External Rotation at 0/35 passively Long-Term Goals: To be met at 8 weeks. 1. 2. 3. 4. AROM > 70% NL Shoulder Pain and Disability Index score < 20% Pain < 2/10 GROC score > +5 The treatment emphasis was to focus on the RTSA Protocol set by the patients’ surgeon. The patient was treated 1 time a week for 8 weeks. The initial plan included patient and family education, therapeutic exercise, ice/IFC, MHP and HEP. Education The patient was educated regarding safety precautions for joint protection. The patient was advised to wear his sling at all times except during physical therapy for up to 4 weeks. He was also advised to avoid extension past neutral and adduction with internal rotation for 12 weeks post-operatively to prevent joint dislocation. The patient was instructed to avoid lifting any object heavier than a coffee cup until week 6, and to avoid supporting body weight using his right upper extremity. Therapeutic Exercise Protocol for RTSA Weeks 2-4: 1. Initiate Self-Passive ROM in forward flexion up to 125 degrees using a pulley for 7 min. 2. Initiate Self-Passive ROM in external rotation up to 45 degrees using a pulley for 7 min. 3. Active Assisted shoulder flexion <80 degrees using table slide for 7 min. 4. Manual shoulder PROM in forward flexion and external rotation in supine for 7 min. 5. Codman’s Pendulum for 7 min. Weeks 4-6: 1. All other exercises as per weeks 2-4. 2. Initiate Active Assisted forward flexion up to full range using a pulley for 7 min. Weeks 6-8: 1. 2. 3. 4. 5. Active Assisted forward flexion up to 160 degrees, and external rotation up to 55 degrees. Wall ladder without abduction for Active Assisted stretch into forward flexion for 7 min. Dowel supine stretch without weight for 7 min. Submaximal internal rotation and external rotation isometrics using a dowel for 7 min. Introduce Deltoid isometric strengthening. Weeks 8-10: 1. Initiate Internal Rotation stretch using a belt for 5 min. 2. Dowel supine with weight as tolerated for 7 min. 3. Initiate light strengthening using 1-3 pounds. Weeks 10-12: 1. Continue with ROM. 2. Progress to resisted forward flexion in standing. 3. Strengthen all components of deltoid and periscapular musculature. Weekly Home Exercise Plan: To be done once a day. Visit 1: Dowel ER stretch in seated position less than 35 degrees for 7 minutes Self- Passive forward flexion stretch in seated position for 12 minutes. Table slide stretch into forward flexion for 7 minutes. Visit 2: Self-Passive forward flexion stretch in seated for 5 minutes. Self-Passive forward flexion stretch in supine for 10 minutes. Table slide stretch into forward flexion for 10 minutes. Visit 3: Active Assisted stretch into external rotation using pulley system for 7 minutes. Active Assisted stretch into forward flexion using pulley system in seated position for 7 minutes. Active Assisted stretch into forward flexion using pulley system in supine position for 12 minutes. Active Assisted stretch into forward flexion against gravity using the wall ladder bilaterally for 7 minutes. Supine bilateral forward flexion using a dowel to facilitate stretch and light strengthening of anterior deltoid for 7 minutes. Visit 4: ER stretch using a dowel for 7 minutes. ER stretch using a pulley system with the chair angled at 25 degrees to facilitate a more aggressive stretch, for 7 minutes. Forward flexion stretch using the pulley system in supine position for 15 minutes. Active –Assisted forward flexion stretch using a wall ladder for 7 minutes to facilitate stretch and light strengthening of the anterior deltoid against gravity. Eccentric strengthening of the deltoid muscle using the wall ladder to climb up the wall, slowly lift hand away from the wall, and slowly lower it back down for 5 minutes. Supine bilateral forward flexion using a dowel with 5 pounds attached to it to facilitate strengthening of the deltoid muscle. Visit 5: ER stretch using a dowel for 7 minutes. ER stretch with elbow at the waist and hand placed on the door frame for 5 minutes. Forward flexion stretch using the wall ladder for7 minutes. Seated self horizontal adduction stretch for 5 minutes. Seated self internal rotation stretch behind the back for 5 minutes. Eccentric deltoid strengthening using a 2 pound wrist weight and climbing up the wall ladder, slowly lifting hand off the wall, and slowly lowering back down for 5 minutes Concentric deltoid strengthening in seated position, using yellow theraband looped around the elbow while the patient holds the other end with opposite hand, the elbow flexed at 90 degrees, performing 3 sets of 20 abductions. Outcome : After 5 Weeks of Physical Therapy AROM Forward Flexion External Rotation Abduction Internal Rotation Horizontal Adduction 0/115 0/10 0/100 Hip 0/90 PROM 0/135 0/25 0/125 N/A 0/90 Improved flexion, not within functional limit. Improved ER, however was still tight Improved abduction Improve IR, however still very tight. Improved Deltoid Strength: 15 pounds by Hand Held Dynamometer; for an estimated arm weight of 10 pounds. Discussion The goals of Physical Therapy after a RTSA usually fall within one of the following categories: 1. Patient education regarding precautions following the surgery. 2. The patient gaining Passive Range of Motion to prevent tissue tightness. 3. The patient gaining Active Range of Motion to prevent tissue tightness and muscle weakness. 4. The patient gaining strength especially of the deltoid and upper trapezius muscles. (2) (4) RTSA’s have certain precautions that the patient must follow to protect the new joint and healing tissue. During the first 4 weeks the patient must avoid flexion past 125 degrees and external rotation past 45 degrees. Some surgeons are able to salvage the subscapularis during the RTSA surgery. In this case, the Physical Therapists are extra careful to protect the integrity of that muscle by avoiding external rotation greater than 25 degrees during the first 6 weeks. The patient is required to wear a sling for up to 4 weeks. During the early weeks the emphasis of treatment is on gentle Passive Range of Motion. Once the sling is discharged the patient is able to actively move the shoulder and participate in more aggressive stretching and strengthening. Studies have shown that after an RTSA the deltoid and upper trapezius muscles become the key movers of the new joint (2). Knowing that the arm is approximately 5% of a persons’ body weight (3), I was able to calculate the weight of this case study patients arm at approximately 10 pounds. Using a Hand Held Dynamometer I was able to assess the patients deltoid strength in pounds, which gave me a good idea of how much strength the patient was going to need to gain in that muscle to be able to forward flex and abduct the arm. This case study patient demonstrated an increase in deltoid strength throughout the time I was treating him by participating in specific deltoid strengthening exercises daily, which directly correlated with the increase ROM during active forward flexion and abduction. Conclusion Reverse Total Shoulder Arthroplasties have become more prevalent over the last 20 years. Understanding that the new joint will be moved primarily by the deltoid and upper trapezius in the absence of a rotator cuff is extremely important for the rehabilitation process. The focus of strengthening must be targeted at those particular muscles for optimal outcome. References 1. Boudreau S, Boudreau E, Higgins L, Wilcox R. Rehabilitation Following Reverse Total Shoulder Arthroplasty. Journal of Orthopaedic & Sports Physical Therapy. 2007; volume 37, number 12. 2. Walker D, Wright T, Banks S, Struk A. Electromyographic Analysis of Reverse Total Shoulder Arthroplasties. Journal of Shoulder and Elbow Surgery. 2014; 23, 166-172 3. Tozeren A. Human Body Dynamics: Classical Mechanics and Human Movement. Springer; 1999. 4. Brigham And Women’s Hospital,Inc. Department of Rehabilitation Services; Reverse Total Shoulder Protocol. Available at: bosshin.com/_userfiles/Shoulder%20%20Reverse%2OTSA%20protocol.pdf. Accessed on October 31, 2014.