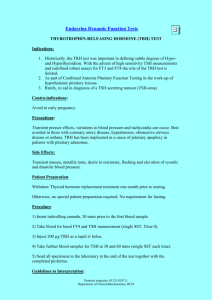
Endocrine Board Review
advertisement

Growth can be easiest way to determine overall health of a child Red Flag: Growth less than 5 cm/year Most common cause of short stature is short parents Secreted in response to GHRH Is secreted in bursts Dopamine causes release of GHRH Somatostatin inhibits the release of GH Anything that effects the pituitary gland will usually result in GH Def. Think midline defects, central incision, bifid uvula Height less than 3 SD below mean, slow growth velocity Characteristic Features Short stature Normal body proportion Increased adiposity around trunk and extremities Boys may have small genitalia Can be seen with midline defects Hypoglycemia Tests Height and bone age is delayed Low IGF-1 and low GH levels Can do GH stimulation tests ▪ Exercise ▪ L-Dopa, insulin, arginine, clonidine, glucagon Treatment GH replacement Hypoglycemia Micropenis Jaundice Midline facial abnromalities TRH TSH T4/T3 Free T4 is the only active form Most are asymptomatic at birth because of maternal thyroxine Newborn screen will check TSH Clinical Presentation Infant can present with goiter Broad nasal bridge, thick lips, poor feeding “hoarse cry” Slow heart rate, low temperature Umbilical hernia Large posterior fontenelle, large sutures on X-ray Most common cause is thyroid dysgenesis Other less common causes Defect in the synthesis Radioiodine given during pregnancy TSH deficiency Treatment should be started within 2 weeks Thyroxine Good prognosis if started early in life Most common cause Hashimoto thyroiditis Dry skin, constipation, hair loss, depressed DTR, goiter More common in girls Sharp deceleration of growth with preserved Tests High TSH Low thyroxine level Often detect antibodies SCFE – high risk with rapid changes of growth. Can see because of rapid halt! Graves disease is most common cause TSH receptor antibody stimulates thyroid cells Symptoms Tachycardia, weight loss, heat intolerance Anxiety, muscle weakness, tremor Exophthalmos,Goiter Tests Elevated thyroxine and triiodothyronine Low TSH Treatment PTU or methimazole Surgery – radioactive iodine/thyriodectomy Common cause of short stature in girls Physical findings Cubitus valgus, sheildlike chest, web neck Gonadal failure ▪ Pubic and axillary hair with no breast development or menarche WorkUp Karyotype PTH Increased Ca+ release from bones Decrease renal excretion of Ca+ Increase conversion of Vit D to 1,25 OH-D Decreases Phos reabsorption from kidney 1,25 OH-D Increase Ca+ reabsorption from gut, bone, kidney Increase phos reabsorption from gut and kidney “PTH antagonist” Decrease Ca+ bone resorption Increases renal Calcium clearance Due to aplasia/hypoplasia of parathyroid gland Can be associated with DiGeorge Also autoimmune forms Presentation can vary Muscle pain or cramps Positive Chvostek or Trousseau sign Seizures Labs: Hypocalcemia Elevated phos Low PTH/low 1,25 OH D EKG: prolonged QT Treatment Calcium Vit D (Calcitriol) Pseudohypoparathyroidism Round facies, short stature, obesity, skin hyperpigmentation, short thick necks Short 4th metacarpals and metatarsals Decreased intelligence Labs Hypocalcemia Hyperphosphatemia Elevated PTH In children usually response to low Ca+ levels Vit D deficiency Malabsorption Chronic renal disease MEN I – neoplasia Pancrease Parathyroid Pituitary Excess glucocorticoid secretion Clinical features Round face, obesity, buffalo hump, stirae, thin extremities, HTN, osteoporosis, decrease growth, hirsutism Testing Elevated urine free cortisol Dexamethasone suppression test Causes Adrenal tumor, pituitary adenoma, ectopic ACTH ACTH-secreting pituitary tumor Which results in excess glucocoriticoid secretion Acquired Deficiency of glucocorticoid and mineralcorticoid Clinical Features Thin body, hyperpigmentation of skin(bronzing) Confusion, weakness Can cause vascular colapse Testing Hyponatremia, hyperkalemia, low cortisol Treatment Replacement of hormones Autosomal recessive Get increased ACTH Causes: 21-Hydroxylase Def ▪ ▪ ▪ ▪ Most common cause Salt wasting Virilization Elevation 17-Hydroxyprogesterone 11ß-Hyroxylase Def ▪ No salt wasting – hypertension ▪ Virilization ▪ Elevated 11-deoxycortisol Presentation Shock or septic in newborn FTT Males – normal genitalia (could have hyperpigmentation of scrotum) Females- ambiguous genitalia Lab findings Low Na Low Cl High K


![SIRT1 Regulates Thyroid-Stimulating Hormone Release by Enhancing PIP5K[subscript gamma] Activity through](http://s2.studylib.net/store/data/011685278_1-09341b1c2f687c801d0cfd5a31ec3d15-300x300.png)