File - CCFP-EM
advertisement

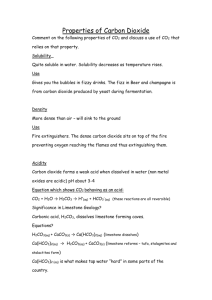
Acid Base Imbalances Acid-Base Regulation Body produces significant amounts of carbon dioxide & nonvolatile acids daily Regulated by: Renal excretion of acid (H+ combines with phosphate or ammonia, which are excreted) Respiratory excretion of CO2 Buffer systems (hemoglobin, phosphate, bicarbonate, proteins) Measurement Arterial: Normal pH 7.36-7.44; normal HCO3 25; normal pCO2 40 Peripheral venous: pH is 0.02-0.04 lower than arterial HCO3 is 1-2 mEq/L higher than arterial pCO2 is 3-8 mmHg higher, depending on peripheral extraction and use of O2 Respiratory Acidosis Definition Decreased pH due to pulmonary CO2 retention (hypoventilation causes hypercapnea) CO2 retention causes increased H2CO3 production – causes acidemia Serum HCO3 is normal acutely, and increases as compensation occurs Causes Increase in PaCO2 Anything which causes a decrease in minute ventilation has the potential to cause respiratory acidosis Airway CNS depression Pulmonary disease Hypoventilation of neuromuscular conditions Symptoms CO2 If narcosis: Headache, blurred vision Asterixis, tremors, weakness Confusion, somnolence prolonged: Signs of increased ICP Papilledema Compensation Acutely: intracellular proteins buffer HCO3 is formed by the intracellular buffers Compensation is insignificant Chronically Renal retention of HCO3 is the primary buffering system Onset: 6-12 hrs, takes days to complete Compensation Acute: HCO3 increases 1 mEq/L for every 10 mmHg rise in PCO2 Insignificant effect on pH Chronic: HCO3 increases 3.5-5 mEq/L for every 10mmHg rise in PCO2 Can almost normalize pH Usually results in hypochloremia Management Must increase minute ventilation Must also improve ventilation Bronchodilators, postural drainage, antibiotics (i.e. treat underlying cause) Role of hypoxic drive??? Respiratory Alkalosis Causes Increased minute ventilation Leads to low pCO2, high pH If acute, HCO3 is normal If chronic, HCO3 will drop due to renal comp. Causes: CNS diseases, hypoxemia, anxiety, hypermetabolic states, toxic states, hepatic insufficiency, assisted ventilation Symptoms Mimic hypocalcemia Depend on degree, acuity & cause Due to irritability of CNS & PNS, and increased cerebral vascular resistance Paresthesias of lips, extremities; lightheadedness, dizziness, muscle cramps, carpopedal spasms Management Treat i.e. remove stimulus Treat underlying cause symptoms E.g. benzos, pain medication, rebreathing mask (allows CO2 retention) Metabolic Alkalosis Definition Low pH due to increased HCO3 or decreased H+ Requires loss of H+ or retention of HCO3 Must know PCO2… elevation of HCO3 could be due to renal compensation for chronic respiratory acidosis Causes Increased HCO3 reabsorption due to volume, K+ or Cl- loss Loss of H+ and Cl- from vomiting and NG suctioning can lead to HCO3 retention Renal impairment of HCO3 excretion Causes Hypovolemic Vomiting/suction, diuretics, adenomas Euvolemic/Hypervolemic Exogenous mineralocorticoids, ectopic ACTH, Cushing’s, severe hypoK, adenoCA Unclassified Milk-alkali syndrome, IV PCN rx, metabolism of organic acid anions, massive transfusion, nonparathyroid hypercalcemia Treatment Treat underlying causes Replace losses May be saline-responsive or saline resistant Metabolic Acidosis Mechanism Increased production of acids Decreased renal excretion of acids Loss of alkali Alcoholic Ketoacidosis Normal glucose High ketones Drinking binge; starvation Lactic Acidosis 2 different forms; l- and d Increased production vs. decreased elimination Systemic Sepsis, hypovolemia, hypoxia Localized E.g. bowel ischemia, metformin, HIV meds Treatment Correct underlying cause Reduce O2 demand Ensure adequate O2 delivery to tissues HCO3 Given to improve hemodynamic consequences of acidosis Summary Look at pH Look at pCO2 and HCO3 Look at patient!! Treat the patient, not the numbers