Advanced Life Support Algorithm
Learning outcomes
• The ALS algorithm
• Importance of high quality chest compressions
with minimal interruption
• Treatment of shockable and non-shockable
rhythms
• Potentially reversible causes of cardiac arrest
• Role of resuscitation team
ALS algorithm
• ILS providers should use those skills in which they
are proficient
• If using an AED – switch on and follow the
prompts
• Ensure high quality chest compressions
• Ensure expert help is coming
Adult ALS Algorithm
Unresponsive?
To confirm cardiac arrest…
Not breathing or
only occasional gasps
• Patient response
• Open airway
• Check for normal breathing
• Caution agonal breathing
• Check circulation
• at same time as breathing
• Monitoring
Unresponsive?
Cardiac arrest confirmed
Not breathing or
only occasional gasps
Call
resuscitation team
Unresponsive?
Cardiac arrest confirmed
Not breathing or
only occasional gasps
Call
resuscitation team
CPR 30:2
Attach defibrillator / monitor
Minimise interruptions
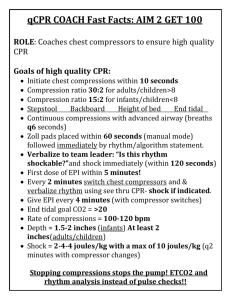
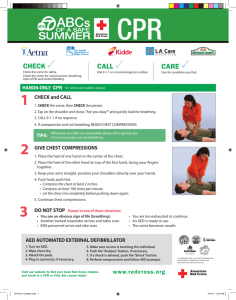
Chest compression
• 30:2
• Compressions
• Centre of chest
• Min 5 cm depth/one third total
• approximately 100 min-1 (but no
faster than 120 min-1 - 2 per second )
• Maintain high quality compressions
•
•
with minimal interruptions
Continuous compressions once
airway secured
Switch compressions provider
every 2 min cycle to avoid fatigue
Shockable and Non-Shockable
START
Charge Defibrillator
Shockable
(VF / Pulseless VT)
CPR
Assess
rhythm
Non-Shockable
(PEA / Asystole)
MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
Shockable
Shockable (VF)
(VF)
• Bizarre irregular waveform
• No recognisable QRS
•
complexes
Random frequency and
amplitude
• Uncoordinated electrical
activity
• Coarse/fine
• Exclude artefact
• Movement
• Electrical interference
Shockable
Shockable (VT)
(VT)
• Monomorphic VT
• Broad complex rhythm
• Rapid rate
• Constant QRS morphology
• Polymorphic VT
• Torsade de pointes
Automated External Defibrillation
• If not confident in rhythm recognition use an AED
• Start CPR whilst awaiting AED to arrive
• Switch on and follow AED prompts
AED
algorithm
• Follow AED prompts
• Will need to pause
compressions for rhythm
analysis
• Following shock
immediately recommence
compressions/CPR
Manual defibrillation
•
•
•
•
Plan all pauses in chest compressions
Do chest compressions when charging
Visual sweep to check bed area when charging
Ensure no-one touches patient during shock
delivery
• Brief pause in compressions to check rhythm
• Deliver shock (or Disarm/“Dump” charge)
• Resume compressions immediately after the shock
• If no shock check patient/pulse
Shockable
Shockable (VF /
(VF / VT)
VT)
Shout “(Compressions
Continue) Stand Clear”
Assess
rhythm
Shockable
Shockable (VT)
(VF / VT)
CHARGE
DEFIBRILLATOR
Assess
rhythm
Shockable
Shockable (VT)
(VF / VT)
CHARGE
DEFIBRILLATOR
Assess
rhythm
Shout “Hands Off”
Shockable
Shockable (VF
(VF / VT)
/ VT)
Assess
rhythm
Confirmed Hands Off
“I’m Safe”
Shockable
Shockable (VF
(VF / VT)
/ VT)
DELIVER
SHOCK
Assess
rhythm
Shockable
Shockable (VF
(VF / VT)
/ VT)
IMMEDIATELY
RESTART CPR
Assess
rhythm
Shockable
Shockable (VF
(VF / VT)
/ VT)
IMMEDIATELY
RESTART CPR
Assess
rhythm
MINIMISEINTERRUPTIONS
INTERRUPTIONSIN
INCHEST
CHESTCOMPRESSIONS
COMPRESSIONS
MINIMISE
Defibrillation energies
• Vary with manufacturer
• Check local equipment
• Defibrillator energy 200 Joules
• unless manufacturer demonstrates better outcomes
with alternate energy level
• If unsure, deliver 200 Joules
• DO NOT DELAY SHOCK
• Energy levels for defibrillators on this course…
Special Circumstances
• Three stacked shocks
• Well perfused and oxygenated patient pre-arrest
• Presenting arrest shockable
• First shock delivered within 20 seconds of onset of
arrest
• Precordial thump
•
•
•
•
Pulseless VT only
Well perfused and oxygenated patient pre-arrest
Defibrillator unavailable
Delivered within 20 seconds of onset of arrest
If VF / VT persists
Deliver
2nd
shock
• 2nd and subsequent
shocks
• 200 J biphasic
• 360 J monophasic
CPR for 2 min
During CPR
Adrenaline 1 mg IV
Deliver
3rd
shock
CPR for 2 min
During CPR
Amiodarone 300 mg IV
• Give adrenaline and
•
after 2nd shock during
CPR then alternate loops
thereafter
Give amiodarone after
3rd shock during CPR
DUMP/DISCHARG
Non-Shockable
E ENERGY
Shockable
(VF / Pulseless VT)
Assess
rhythm
Non-Shockable
(PEA / Asystole)
MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
Non-Shockable
Non-shockable (Asystole)
(Asystole)
• Absent ventricular (QRS) activity
• Atrial activity (P waves) may persist
• Rarely a straight line trace
• Adrenaline 1 mg IV then every alternate loop
Non-Shockable
Non-shockable (Asystole)
(PEA)
• Clinical features of cardiac arrest
• ECG normally associated with an output
• Adrenaline 1 mg IV then every alternate loop
During CPR
During CPR
Airway adjuncts (LMA / ETT)
Oxygen
Waveform capnography
IV / IO access
Plan actions before interrupting compressions
(e.g. charge manual defibrillator)
Drugs – During CPR
Shockable
• Adrenaline 1 mg after 2nd shock (then every 2nd loop)
• Amiodarone 300 mg after 3rd shock
Non Shockable
• Adrenaline 1 mg immediately (then every 2nd loop)
/Hyperthermia
Reversible Causes
/Hypokalaemia – metabolic disorders
Airway and ventilation
• Secure airway:
• Supraglottic airway device e.g. LMA, i-gel
• Tracheal tube
• Do not attempt intubation unless trained and
competent to do so
• Once airway secured, if possible, do not interrupt
chest compressions for ventilation
• Avoid hyperventilation
• Capnography - waveform
Immediate post-cardiac arrest treatment
ISBAR
• I = Identify
•
Identify the patient you are calling about
• S = Situation
•
Say what you think the current problem is/appears to be
• B = Background
•
Information about the patient
• A = Assessment
• I
nclude specific observations and vital sign/observations
values based on ABCDE approach
• R = Response/Requirement
• S
tate explicitly what you want the person you are calling
to do
Resuscitation team
• Roles planned in advance
• Identify team leader
• Importance of non-technical skills
•
•
•
•
Task management
Team working
Situational awareness
Decision making
• Structured
communication
• ISBAR or RSVP
Any questions?
Summary
•
•
•
•
•
•
•
Importance of high quality chest compressions
Minimise interruptions in chest compressions
Shockable rhythms are VF/pulseless VT
Non-shockable rhythms are PEA/Asystole
Use an AED if not sure about rhythms
Correct reversible causes of cardiac arrest
Role of resuscitation team
Immediate Life Support Course
Slide set
All rights reserved
© Australian Resuscitation Council & Resuscitation Council (UK) 2010