Introduction to Medical Nutrition Therapy
advertisement

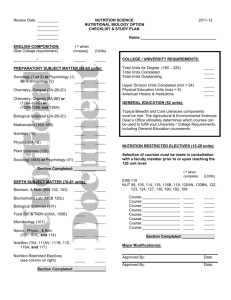
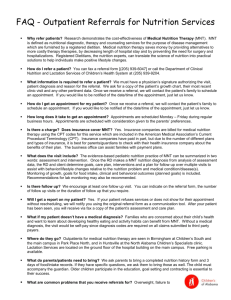
Introduction to Medical Nutrition Therapy NFSC 470 Nutrition Care Process Process of planning for and meeting MNT needs of the individual 1. Assessing nutrition status and analyzing data to identify nutrition related problems 2. Coming up with a nutrition diagnosis 3. planning & prioritizing nutrition intervention(s) to meet the patient’s needs 4. Evaluating the nutrition care outcomes Medical Nutrition Therapy • The use of specific nutrition interventions to treat an illness, injury or condition. Standards of Care Standards of care: treatment guidelines that specify appropriate treatment protocols based on scientific evidence, and collaboration between medical professionals involved in the treatment of a given condition. Example: • Treatment standards applied within public hospitals to insure that all patients receive appropriate care regardless of financial means. MNT Protocols • MNT protocols are a set of steps incorporating current professional knowledge (evidence-based) that clearly define the level, content and frequency of nutrition care appropriate for a disease or condition. MNT PROTOCOLS – SAMPLE TOPICS • • • • • • • • • • Nutrition Assessment Nutrition Risk Levels Referrals to Nutrition Care Professional Supervision of Nutrition Documentation Providing Therapeutic Diets Height/Weight Monitoring Significant Weight Loss Protocol Calculating Nutrition Needs Pressure Sores Dysphagia • • • • • • • • • • • • Pernicious Anemia Vitamin B12 Deficiency Megaloblastic Anemia Folate Deficiency Respiratory Diseases Cardiovascular Disease Cerebrovascular Disease Cancer Clients on NPO Enteral Nutrition Total / Peripheral Parenteral Nutrition Gastrointestinal (GI) Disorders Liver disease: hepatitis & cirrhosis http://www.guideline.gov/summary/summa ry.aspx?doc_id=3295&nbr=2521&string=c holesterol Who makes sure the standards of care are met and appropriate protocols are followed? JCAHO: What is JCAHO? • Independent, not-for-profit organization • Governed by a board that includes physicians, nurses, and consumers • Sets standards of patient care • Evaluates the quality and safety of care for more than 15,000 health care organizations • To maintain and earn accreditation, JCAHO conducts an extensive on-site review at least once every three years. JCAHO evaluates the organization's performance in areas that affect patient care. • Accreditation is awarded based on how well the organizations met Joint Commission standards. Patient Screening for Malnutrition or Need for Nutrition Intervention JCAHO: screen for nutrition risk within 24 hours of admission – I.e. – Nutrition “triggers” indicate need for more intensive nutrition assessment: • • Within • Enloe re-screens right away by • Examples of screening criteria: – Over age 80 automatically = moderate risk – Diagnosis: • • • • – – renal failure = moderate risk trauma and ICU = high risk Peds in ICU = high risk Ventilated pt. in ICU = high risk • Risk level is established based on screening criteria until RD assesses the patient. • Then, it’s a point system to determine actual risk level, with diagnosis, dietary intake, albumin, and wt status all considered to be worth a given number of points. • The points are added up to determine nutrition risk level for the purpose of prioritizing who will be seen first and most frequently. Case Example Influences on Nutrition Care • Managed care – A concept based on an effort to control escalating health care costs by the health insurance industry – Defines a “reasonable maximum fee” which health care providers may charge for any given service – Providers have to accept these maximum fees if they wish to be listed in directories of “approved” physicians of specific insurance companies. Types of Managed Care Organizations 1. Health Maintenance Organization (HMO) • • • • • • Insurance company controls all aspects of the health care of the insured. Each member is assigned a primary care provider (PCP) who is responsible for the overall care of members assigned to him/her. Pt. must obtain a referral from the PCP to see a specialist. PCP must authorize non-emergency hospital admissions Typically, services are not covered if performed by a provider not specifically approved by the HMO, unless it is an emergency situation as defined by the HMO. Since the 1980s, HMOs have been protected by Federal law from malpractice litigation on the grounds that the decisions regarding patient care are administrative rather than medical in nature. 2. Preferred Provider Organization (PPO) – – – – – – Policy-holder is free to choose his/her own physician Better benefits if a PCP (from the approved “network”) is seen “Network" caregivers and facilities are independent of insurance company ownership, and may hold contracts for reimbursement with multiple insurors. "Pre-certification" (prior approval) may be required before nonemergency hospital admissions, testing, consultations or outpatient surgery under many plans. Providers remain liable for malpractice. PPO provders hold contracts with insurance companies, under which they agree to accept the reimbursement that was negotiated at rates agreed upon between themselves and the insuror. 3. Federal Insurance Plans a. Medicare – Part A: ______________________________ • Medicare's Part A helps to cover hospital stays, skilled nursing facility care, some home health care, and hospice care. Part B: _______________________________ _____________________________ • Medicare's Part B helps to cover doctors' services, outpatient hospital services, and other medical services not covered by Part A, such as home healthcare. (Monthly Premium: $88.50/month in 2006) b. Medicaid – Federal program, but run by individual states so wide variation in eligiblility When is MNT a covered health insurance benefit? • Medicare, MediCal and private insurers may cover MNT when determined to be reasonable and medically necessary. • The RD must be acting upon referral from a physician with a “prescription” for assessment and counseling for a nutrition-related diagnosis. • International Classification Diseases (ICD-9CM) codes are used to identify different diagnoses such as diabetes and hypertension. The diagnoses codes are selected by the referring physician. • Insurance plans are required by California law to cover Diabetes Self-Management Training (DSMT) – MNT provided by an RD or qualified nutrition professional. – Medi-Cal may cover DSMT/MNT but is not required to. • Medicare part B covers MNT for – – – – – Type 1 and Type 2 Diabetes Gestational Diabetes Non-Dialysis Kidney Disease Post renal transplant (6 to 36 months) with the RD as a Medicare provider. What are ICD-9-CM Codes? • The International Classification of Diseases, 9th revision, Clinical Modification codes, developed by WHO are medical and surgical diagnosis codes. (revised each year) – – • Many codes require extensions to clarify the diagnosis: – 272.0 for – 272.2 for What are Current Procedural Terminology (CPT) Codes? • CPT codes are procedural codes developed by the AMA for professional billing. • Billing codes for MNT: – 97082 = initial assessment and intervention, faceto-face with the patient. Each billed unit is 15 minutes. – 97083 = reassessment and intervention, face-to-face with the patient. Each billed unit is 15 minutes. – 97084 = a group visit of 2 or more individuals. Each unit is 30 minutes. Study demonstrates MNT costsavings Cost-Savings MNT Outcomes study (Illinois Dietetic Assoc.) determined cost-savings and cost-prevention realized within two years of an initial MNT visit provided by an RD. The results, based on 42 patient outcomes, show that MNT can have the following impact and average cost savings per patient: • • • • • reduction of rx meds reduction in lab, other tests reduction in MD office visits reduction in # of hospitalizations reduction in emergency room visits $1,052 $ 654 $ 505 $4,960 $2,400 The study also demonstrates that MNT can save insurers and employers $19, 305 per patient. Total estimated dollars saved when coupling costsavings with cost-prevention ranged from $220 to $70,420 per patient. Shows the value of documenting MNT patient outcomes, which are strongly needed to build the case for nationwide MNT coverage. Review of Medical Charting • Medical record = legal document – Communication among members of health care team. – Confidentiality – POMR • • • • • • Computer or black ink Chronological order Institution’s accepted abbreviations Signature, and actual date and time of entry Professionalism Corrections/addendums • If you didn’t chart it, you didn’t do it. • Never chart for another person. • Confidentiality issues – Verbal, written, electronic – Legal penalties – Disciplinary action by hospital Writing a SOAP Note • Subjective – Information pt. or caregiver/family tells you, what you observe but haven’t measured. – Significant nutritional history • Appetite, home diet practices, chewing and swallowing ability, N/V/D, etc. – Pertinent socioeconomic, cultural info – Level of physical activity • Objective – Factual, reproducible observations (anthropometric and lab data) – Dx. And pertinent medical history – Age, gender, height, weight, %IBW, etc. – Desirable weight/weight goal – Labs (pertinent) – Diet order/nutrition support (current diet provides…) – Meds (pertinent) – Calculated nutrient needs (may also go under “A” • Assessment – Your assessment of pt. nutritional status based on S & O data • If you make an assessment statement in “A,” the information has to be under “S” or “O.” Example: pt. w/mod. depleted visc. prot. stores per alb level (must be listed under ‘O’). – Do not repeat lab values in assessment (“alb. Of 3.0 indicates…” No-no) – Evaluation of pertinent nutritional history – Assessment of labs – Assessment of patient’s comprehension and motivation, if appropriate – Assessment of the diet order and/or feeding modality – Anticipated problems and/or difficulties for patient compliance or adherence • Plan – Diagnostic studies needed – Suggestions for gaining further pertinent data – MNT goals – Recommendations for nutrition care and nutrition education – Recommendations for other health care providers – Specific parameters you will monitor – Plan for follow-up (time frame) This is your plan to improve nutritional status or make recommendations to the doctor examples: 1. Educate pt. on 1500 kcal diabetic diet 2. Provide Ensure w/meals TID 3. Recommend MVI q day 4. Provide food preferences (list specific changes) 5. Recommend increased TF rate to 75cc/hr. 6. Monitor ______ (labs) 7. Follow-up in 2 days Other documentation styles: • DAR – diagnosis, assessment, recommendations • PIE – problem, intervention, evaluation • PGIE – problem, goal, intervention, eval. • (content is the same regardless of recording style)