Hematology-Oncology Review Session
advertisement

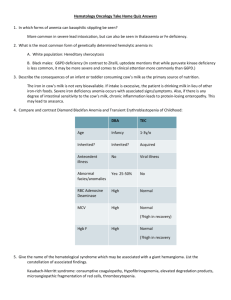
Hematology-Oncology Review Session Pete Voorhees Iron Deficiency Anemia • • • Symptoms of anemia (fatigue / weakness, SOB / DOE). Ice pica and koilonychia are specific for iron deficiency! Microcytic (low MCV), hypochromic (low MCHC) RBCs. – Other causes of microcytosis include thalassemias, sideroblastic anemias. • • • Ferritin is low, Serum Fe low, TIBC or transferrin normal or high, Fe saturation (serum Fe / TIBC) low. Causes: chronic blood loss, malabsorption, decreased intake, pregnancy. Treatment: Give iron, fix source of blood loss. Vitamin B12 Deficiency • • • Symptoms of anemia. Peripheral neuropathy (decreased proprioception, vibratory sense). Macrocytic (high MCV) RBCs. – Other causes of macrocytic anemias include liver disease, folate deficiency, anemias ass. with a high retic. ct., hypothyroidism, HIV therapy (AZT), chemotherapy. • • • • Hypersegmanted neutrophils. Dx: low B12 levels. Causes: pernicious anemia (Ab to IF), malabsorption (ileal resection), pancreatic insufficiency. Treatment: replace B12. Folate Deficiency • Same symptoms as B12 deficiency but no neuropathy. • Macrocytic RBCs and hypersegmanted neutrophils. • Dx: low folate or RBC folate level. • Causes: Decreased intake (alcoholic), malabsorption, increased utilization (depletion) of body stores (chronic hemolytic anemia) • Treatment: Replace folate. Hereditary Spherocytosis • Symptoms of waxing / waning anemia, jaundice. – Hemolysis accelerated by infection. • Splenomegaly (hyperplasia secondary to increased workload), pigmented gallstones (h/o cholecystectomy), ankle ulcers. • Family history – AD. 1 : 5000 people of european descent affected. Hereditary Spherocytosis • Blood smear: spherocytes, polychromatophilia (increased reticulocytes). • Labs: Increased retic. ct., increased LDH, increased indirect bilirubin, increased osmotic fragility. • Treatment: folate replacement, splenectomy in some circumstances). • Genetic defect: Spectrin, ankyrin mutations. • Pearl: Parvovirus B19 infection in patients with hemolytic anemis in general = aplastic crisis. G6PD Deficiency • Episodic hemolytic anemia. – Triggered by oxidant stress: drugs, infection. • Occurs in males – X-linked, 10 – 14% of males of African descent carry an unstable A- variant of G6PD. • More severe, chronic form seen in men of Mediterranean descent. – Think fava beans in a Mediterranean pt. G6PD Deficiency • G6PD is required to generate NADPH and ultimately reduced glutathione. • Glutathione required to prevent oxidative damage to hemoglobin. • Deficient glutathione leads to oxidized, methemoglobin which precipitates out as Heinz bodies. • Macrophages of the RES phagocytose bits of RBC membrane with underlying precipitated hemoglobin. G6PD Deficiency • Smear: Bite cells and blister cells. • Diagnosis: Smear, G6PD level, heinz body prep. – G6PD levels may be normal in the acute setting due to selective removal of older RBCs with lower baseline G6PD levels. • Treatment: Get rid of offending oxidant stress (drug, infection). – Important drugs to know that may precipitate hemolysis in these folks: SULFA, anti-malarial drugs, dapsone, vitamin K, fava beans. Warm Autoimmune Hemolytic Anemia • Symptoms of anemia, jaundice, splenomegaly. • Smear: spherocytes, polychromatophilia. • Labs: Increased retic. ct., high LDH, high indirect bilirubin, + direct Coomb’s test (direct antiglobulin test or DAT). – Indirect Coomb’s usually positive as well. • Treatment: immunesuppression (steroids, spenectomy), treat / remove underlying trigger. Warm Autoimmune Hemolytic Anemia • Causes: Idiopathic, SLE, lymphoproliferative disorder (lymphoma, CLL). • Drugs – Innocent bystander: quinine, quinidine, INH – Hapten: PCNs, cephs – Autoimmune: alpha-methyldopa, procainamide Cold Agglutinin Disease • Symptoms of anemia, acrocyanosis. • Smear, RBC agglutination, polychromatophilia. • Labs: Increased retic. ct., LDH, bilirubin, + Coomb’s test (C3 +. IgG -), + cold agglutinin titer. • Treatment: avoidance of cold, treat underlying disease, immune-suppression (chemotherapy). • Associated diseases: lymphoproliferative diseases (lymphoma, CLL) or after infectious mononucleosis or mycoplasma infection (“walking” pneumonia). Hemophilia A and B • X-linked. • Factor VIII (Hemo A) > Factor IX (Hemo B) deficiency. • Manifests as soft tissue and joint bleeds, provoked and spontaneous as well as other bleeding (intracranial, GU). • Long-term complications: Joint destruction from repeated bleeds, pseudotumors. • Labs: Prolonged aPTT, normal PT, normal TCT, normal platelet function screen and bleeding time. • Treatment: recombinant Factor VIII or IX replacement, ddAVP for mild hemophilia A (leads to release of endothelial stores of FVIII). Von Willebrand’s Disease • Autosomal dominant. • The most common inherited bleeding disorder. • Mucocutaneous bleeding (epistaxis, gum bleeding, GU/GI bleeding, menorrhagia). • Types 1 (mild deficiency) , 2 (qualitative abnormality), and 3 (severe deficiency). • Labs: Prolonged bleeding time / platelet function screen, slightly prolonged aPTT (due to low FVIII levels), low von Willebrand activity level, +/- low vWF antigen levels. • Treatment: Type 1: ddAVP. Type 2 and 3: vWF and FVIIIcontaining plasma product (Humate-P). Venous Thrombosis • Causes – Acquired • Cancer • Myeloproliferative disorders (P. Vera, Essential thrombocytosis) • Antiphospholipid antibody syndrome • Hyperhomocysteinemia • Pregnancy • OCPs, HRT • Prior venous thrombosis • Age • Immobilization • Surgery Venous Thrombosis • Inherited causes – Factor V Leiden mutation!!!! – Prothrombin gene mutation – Protein C def. – Protein S. def. – Antithrombin def. – Dysfibrinogenemias, elevated FVIII, IX, XI levels Venous Thrombosis • Symptoms: pain / swelling in leg, chest pain, SOB (pulmonary embolism). • Diagnosis: – Duplex ultrasonography (doppler ultrasound) – IPG – Contrast venography – Magnetic resonance venography – D-dimer Venous Thrombosis • Treatment – Heparin or low-molecular weight heparin • Potentiates anticoagulant effect of endogenous anti-thrombin. – Warfarin • Depletes vitamin K-dependent coagulation factors (II, VII, IX, and X). – Fibrinolytics (tPA) if patient clinically unstable with extensive clot burden. • Activates the fibrinolytic enzyme, plasmin. Pseudothrombocytopenia • Lab artifact! • The patient will have no bleeding history. • Clumps of platelets will be seen on the fringes of the smear. • Due to presence of EDTA in tube. • Diagnosis: smear, recheck plt count in citrated or heparin-anticoagulated tube. Disseminated Intravascular Coagulation • • • • • • Diffuse, abnormal activation of coagulation, leading to consumption of clotting factors, and thrombocytopenia. Clinically manifests as bleeding but the clinical picture is typically dominated by the disease that led to the DIC. Prolonged PT, aPTT, TCT, and low platelets, low fibrinogen, low antithrombin, elevated D-dimer. MAHA may be seen on the smear. Causes: Severe infection, AML (esp. APL or M3 AML), obstetrical complications (eclampsia), severe burns. Treatment: replacement (platelets, clotting factors with FFP, fibrinogen with cryoprecipitate), treat underlying disease. Thrombotic Thrombocytopenic Purpura (TTP) • Abnormal activation of platelets and endothelium leading to fibrin deposition in the microvasculature and destruction of RBCs and consumption of platelets. • Pentad – – – – – MAHA Thrombocytopenia Fever Renal failure Neurologic deficits • Smear shows MAHA • Labs: PT, aPTT, TCT, fibrinogen, d-dimer are normal. • Cause: Primary (idiopathic) TTP due to autoantibodies to ADAMTS13; secondary causes: pregnancy, drugs (mitomycin-C, quinine, ticlopidine, cyclosporine), HIV • Treatment – Plasma exchange Hemolytic Uremic Syndrome • Similar to TTP but renal failure dominates the clinical picture. • The blood smear will look the same and the lab work will be the same. • More common in children after diarrheal illness (esp. E. Coli O157/H7 and shigella). • Treatment: Supportive care +/- plasma exchange (less effective here than in TTP). Idiopathic Thrombocytopenic Purpura • • • • • The platelet equivalent of warm AIHA. Symptoms: mucocutaneuos bleeding. PE: petechiae. Smear: absent / few platelets. Causes: idiopathic, drugs (PCNs, sulfa (TMPsulfamethoxazole, quinine), SLE, HIV, lymphoproliferative disorders. – Heparin causes an immune-mediated thrombocytopenia paradoxically associated with excessive clotting. • Treatment: Corticosteroids +/- IVIG, splenectomy for relapse, anti-D immune globulin, immunosuppressants. Polycythemia Vera • Symptoms of increased viscosity: decreased mental acuity, blurred vision, tinnitus, headache, dizziness, paresthesias. – PV specific findings: post-bathing pruritus, erythromelalgia, thrombosis, hemorrhage, hypermetabolic symptoms. • PE: plethora, retinal vein distention, hepatosplenomegaly. • Labs: Increased WBCs, HCT, and platelets. Basophilia, high LAP score, high uric acid and vitamin B12, low erythropoietin level. • Treatment: phlebotomy, hydroxyurea, interferon-alpha, busulfan, P32. – Aspirin reduces the incidence of thrombosis. Essential Thrombocytosis • Similar to P. Vera. Asymptomatic or excessive bleeding and / or clotting, splenomegaly. • Smear: large platelets. Labs: thrombocytosis, leukocytosis. Must r/o CML. • Treatment: age < 60, no clotting risk factors (smoking, HTN, etc.), plts < 1 – 1.5 million, no h/o clotting / bleeding – observation. Otherwise, hydroxyurea, anagrelide, or interferon-alpha. – ASA alleviates symptoms of microvascular occlusion (e.g.. erythromelalgia). Idiopathic Myelofibrosis • • Symptoms of hypermetabolism (weight loss, fevers, sweats), splenomegaly (abd. pain, early satiety), anemia, +/thrombocytopenia. Leukoerythroblastic blood smear – – • • • • • Tear drop shaped RBCs, nucleated RBCs. Left-shifted WBCs. WBC count normal or high at diagnosis but eventually drops, HCT usually low at diagnosis, plts may be up, down or low. Dry tap on bone marrow aspirate. Increased fibrosis on bone marrow biopsy. P. Vera and ET can evolve into a “spent,” myelofibrotic stage. Treatment largely supportive, bone marrow transplant has been tried in younger patients. CML • Symptoms of hypermetabolism, splenomegaly, anemia. • Smear with increased numbers of WBCs (granulocytes of all stages of maturation). • Labs: Increased WBCs, +/anemia, low LAP score, low vitamin B12 level. • Cytogenetics: t(9;22), BCRABL. • Treatment: Bone marrow transplant, Gleevec. • Monitoring disease: cytogenetics, FISH for t(9;22), PCR for BCR-ABL.