Infectious diseases/ Haematology/ Rheumatology/ Dermatology
advertisement

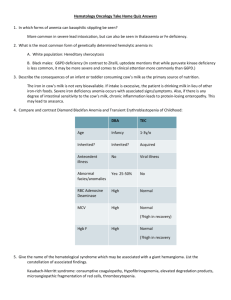
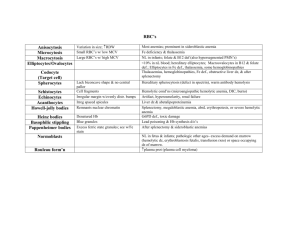
Infectious diseases/ Haematology/ Rheumatology/ Dermatology Haematological Interpretation of haematological investigations*** Anaemia** Abnormal haemoglobins* Disorders of haemostasis and coagulation*** Anticoagulant agents** Antiplatelet agents** Neutropaenia** Thrombocytopaenia** Thrombocytosis* Disorders of white cells* Myelodysplastic disorders* Paraproteinaemia* Rheumatology Rheumatoid arthritis** Gout* Septic arthritis *** Urgencies and emergencies in systemic rheumatic diseases** Thoracic and lumbar pain syndromes** Neck pain* Shoulder pain* Tendonitis and tenosynovitis* Repetitive strain injury and overuse syndromes* Regional pain syndromes* Tunnel syndromes* Complications of drugs used in rheumatic diseases* Dermatology in emergency care Dermatitis and eczema* Urticarial and allergic rashes** Viral exanthems* Macular rashes* Maculopapular lesions** Papular and nodular rashes* Petechial and purpuric rashes** Vesicular and bullous rashes** Ulceration* Cellulitis** Dermatological manifestations of underlying systemic disease** Dermatological manifestations of neoplastic disorders* Infectious disorders Universal precautions* Protection of staff from infectious disease* Isolation of patients with infectious disease* Infection control in the ED** Needlestick injury *** Vaccination in the ED ** Reportable communicable diseases* Antibiotic use in the ED** Outpatient antibiotic therapy** Febrile infant management *** Historical* SIRS *** Sepsis, severe sepsis and septic shock *** Multiple organ dysfunction*** Toxic shock syndrome** Infections in the returned overseas traveller*** Bacterial - Meningococcal ***. Rest *-** Viral - HIV and Herpes **. Rest * Mycoplasma infections* Fungal infections* Protozoal infections* Tick-born infections* Infections from human bites** Infections from animal bites** Infection from a marine source** Infection in a burns patient** Biologic weapons* Haematology Haematological Investigations Hemoglobin - <14g/dl – anemia, >18g/dl – polycythemia MCHC – elevated in hereditary spherocytosis Hematocrit = (0.0485 x Hb + 0.083) x 100 Hyperlipemic plasma may elevate Hb falsely Very high WCC can falsely elevate Hb Leukocytosis - >11 x 109 /L Neutrophilia – elevation of neutrophilic fraction of leucocytes, very non-specific finding in ED Causes o Hemorrhage o Drugs/toxins o Acute stress response o Infections – toxic cell changes more specific o Severe pain o Vomiting o Inflammation Lymphocytosis - > 4x109/L o Causes o Viral infections – EBV,CMV, HIV, HSV etc o Other infections – TB, toxoplasmosis, syphilis o Autoimmune diseases o >20x109/L usually CLL o Atypical lymphocytes in EBV sensitive Eosinophilia o Causes o Allergic diseases o Asthma o ADR o Parasitic infections o Uncommon – Hodgkin’s, vasculitis, primary eosinophilic syndromes Leukopenia o Causes o Pancytopenia due to immunosuppression, aplasia, chemotherapy o Neutropenia in severe sepsis The blood film examination Red cell morphology Anisocytosis – unequal cell sizes – macrocytosis Poikilocytosis – irregular shapes of RBC – dyserythropoiesis Hypochromia – iron deficiency Target cells – central loss of staining o Occurs in o Severe iron deficiency o Liver disease o Sickle cell disease o Thalassemia o Post-splenectomy Burr cells – spiky projections – uremia and red cell trauma Basophilic stipling – RNA granules in cytoplasm, indicated damaged young red cells o Severe anemia o Lead poisoning o Thalassemia Polychromasia – reticulocytosis Howell-Jolly bodies – remanants of nuclear material – post-splenectomy Schistocytes – fragmented RBCs o Post splenectomy o DIC o TTP o Mechanical trauma – prosthetic valve, march Tear drop cells – myelofibrosis, extramedullar hematospoiesis Heinz bodies – denatured Hb – hemolytic anemias White cell morphology Toxic granulation – lysosomal granules in neutrophil cytoplasm Band forms – unsegmented nuclei Leuko-erythroblastic picture – large number of immature precursors Causes o Ca prostate o Extensive bony metastases o Myeloma o Hodgkin’s disease o Myelofibrosis o Glycogen storage diseases Reticulocyte count – raised in Hemolytic anemias Severe bleeding Nutritional anemias recovery Erythrocyte sedimentation rate – clumping of RBC to form rouleaux in inflammatory states raised in Bacterial infection - >30mm/hr Normal pregnancy – 80mm/hr Anemia Rheumatic fever Lipidemia Hyperfibrogenemia Hyperglobulinemia Severely raised in – SLE, rheumatoid arthritis, temporal arteritis, polymyalgia rheumatic Evaluation of Anemia Classified into microcytic, macrocytic and normocytic types depending on MCV Microcytic - <80fl o Iron deficiency o Thalassemia o Sideroblastic anemia o Multiple myeloma o Chronic systemic illness Macrocytic – MCV>100fl o Vitamin B12 deficiency o Folate deficiency o Chronic alcoholism o Chronic liver disease o Hypothyroidism o Myelodysplastic syndrome o Aplstic anemia o >115fl – always due to Vitamin B12 or folate deficiency Normocytic normochromic – o Early stages of most anemias o Myelodysplastic syndrome o Bone marrow infiltration o Chronic systemic disease o Prolonged critical illness o o Hemolysis Congenital – e.g. Diamond-Blackfan syndrome Hemolytic anemias Extracorpuscular defects Corpuscular defects Membrane defects spherocytosis elliptocytosis Hemoglobinopa thies Thalassemia Enzyme defects Autoimmune Mechanical G6PD deficiency Incompatible blood transfusion Long distance runners PNH SLE, RA, UC prosthetic heart valves HbS Penicillin lymphoma, CLL Intravascular Hemolysis Extravascular hemolysis • Microangiopathic hemolytic anemia • DIC, TTP, HUS, preeclampsia, vasculitis • March hemoglobinuria • Cardiac valve / IABP • Paroxysmal nocturnal hemoglobinuria • Autoimmune diseases • Rh incompatibility Laboratory features Reticulocytosis – increased MCV Heinz bodies seen on film Increased unconjugated bilirubin Increased LDH Decreased haptoglobin Presence of methemoglobin in severe cases Glucose 6-phosphate dehydrogenase (G6PD) deficiency X linked inherited disorder – common in African-Caribbean Hemolysis due to oxidative stress in presence of low levels of reduced glutathione Usual precipitants – drugs and viruses Drugs commonly responsible o Sulphonamides o Nitrofurantoin o Anti-malarials o Methylene blue o Naphthalene o Vitamin K o Aspirin Petechiae Palpable petechiae due to Vasculitis Subacute bacterial endocarditis Rheumatoid arthritis SLE Cryoglobulinemia Causes of Paetechiae Thrombocytopenia o Platelet dysfunction Congenital Aspirin, NSAID Myeloproliferative disorders Dysproteinemia Fat embolism Small vessel disease o Infection SBE Vasculitis Meningococcal Measles o Drugs Steroids o Scurvy Cushing’s syndrome Polyarteritis nodosa Henoch Schonlein purpura Neutropenia Treatment Early recognition and treatment of bacterial infection Institution of supportive care to prevent progression to overwhelming sepsis and shock Empiric broad-spectrum antibiotic therapy after blood cultures drawn Ideally coverage for both gram negative and gram positive organisms; cover for gram positive cocci if central line in situ Ticarcillin/clavulante + aminoglycoside ± Vancomycin Addition of anti-fungal if sepsis features continue despite above after 96hrs Disposition Most neutropenic patient with/without fever will require admission Thrombocytopenia Decreased production Increased destruction Pseudothrombocytopenia Management: ITP o Immune modulation – IV glucocorticoids and IV Immunoglobulin o Splenectomy for failure of medical therapy and ongoing bleeding o Platelet transfusions only in case of life-threatening hemmorhages Drug-related o Withdrawl of drug usually results in prompt recovery Thrombotic thrombocytopenic purpura o Pentad of clinical findings Fever Thrombocytopenia Microangiopathic hemolytic anemia Neurologi abnormalities Renal involvement o Causes Idiopathic Pregnancy Verotoxin producing E.coli and Shigella dysentery Malignancy Chemotherapy, BMT o Treatment Plasma exchange – fall in mortality from 90% to <20% Hemophilia Group of congenital disorders of blood coagulation due to deficiency of clotting factor proteins of intrinsic coagulation pathway. Hemophilia A – o Commoner form (80%), 1-8000 male live births, female carriers o Deficiency of factor VIII o X-linked pattern of inheritance Hemophilia B – o Less common (20%), 1-25000 live male births o Deficiency of factor IX (Christmas disease) o X-linked pattern of inheritance Severity of disease o Mild (6-30% activity) – persistent post-op bleeding, spontaneous bleeding does not occur o Moderate (1-5% activity) – bleeding into joints and muscles post minor trauma + excessive bleeding after asurgeries o Severe (<1% activity) – spontaneous joint and muscle bleeding and all of above Common presentations o Hemarthrosis – knee, elbows, ankles, shoulders, hips and wrists o Soft tissue hematomas o Gum bleeding o Superficial bruising o CNS bleeding o Retroperitoneal bleeding Investigations o General investigations in c/o severe bleeding o Coagulation studies PT – measure factor II, VII, V and X activity thus normal PTT – measures all factors’ activity but not VIII so may be normal if activity >30% Specific factor assays indicated when suspected Treatment o R-rest, I-Ice, C-gentle compression bandage, E-elevation, S-splint o Analgesia – oral and parenteral, PCA (avoid aspirin, NSAID) o IM injections contra-indicated, limit skin punctures. o Surgery for compartment syndrome o Early consultation and multi-disciplinary approach o If >10% factor VIII activity – desmopressin may be tried, especially if past h/o response o Follow specialized treatment plans usually available with patient o Factor VII infusions – 3500IU bolus then 1750 IU 12hrly in severe bleeds, titrate smaller doses for less severe bleeding after discussions with specialist Indications for hospital admission – most patients self-administer factor VIII at home o ICH o Large bleed or bleed in close compartment – head, neck, throat o Compartment syndrome o Analgesis requirements o Social constraints o Bleeding in iliopsoas, hip or intra-abdominal o Antifibrinolytic therapies – tranexamic acid and aminocaproic acid for GI/mucosal bleeding Blood and blood product transfusions 1 Estimated fluid and blood losses (70Kg man) 2 Guidelines for transfusion of blood products Adverse reactions to transfusions