Integumentary System PowerPoint
advertisement

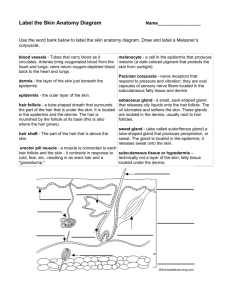
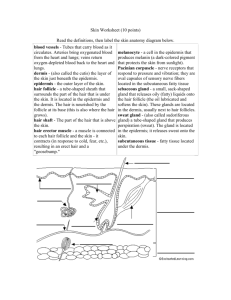
5 The Integumentary System Skin (Integument) Consists of three major regions 1. 2. 3. Epidermis—superficial region Dermis—middle region Hypodermis (superficial fascia)— deepest region Subcutaneous layer deep to skin (not technically part of skin) Mostly adipose tissue Hair shaft Epidermis Papillary layer Dermis Reticular layer Hypodermis (superficial fascia) Nervous structures • Sensory nerve fiber • Pacinian corpuscle • Hair follicle receptor (root hair plexus) Dermal papillae Subpapillary vascular plexus Pore Appendages of skin • Eccrine sweat gland • Arrector pili muscle • Sebaceous (oil) gland • Hair follicle • Hair root Cutaneous vascular plexus Adipose tissue Figure 5.1 Epidermis The Epidermis is a keratinized stratified squamous epithelium Cells of epidermis Keratinocytes- produce fibrous protein: keratin Keratin helps give skin its protective properties Melanocytes Found in the deepest layer of the epidermis Produce pigment melanin Epidermal dendritic (Langerhans) cells- ingest foreign substances and are key activators of our immune system arise from bone marrow Tactile (Merkel) cells- sensory receptors for touch. (a) Dermis Stratum corneum Most superficial layer; 20–30 layers of dead cells represented only by flat membranous sacs filled with keratin. Glycolipids in extracellular space. Stratum granulosum Three to five layers of flattened cells, organelles deteriorating; cytoplasm full of lamellated granules (release lipids) and keratohyaline granules. Stratum spinosum Several layers of keratinocytes unified by desmosomes. Cells contain thick bundles of intermediate filaments made of pre-keratin. Stratum basale Deepest epidermal layer; one row of actively mitotic stem cells; some newly formed cells become part of the more superficial layers. See occasional melanocytes and epidermal dendritic cells. Figure 5.2a Layers of the Epidermis: Stratum Basale (Basal Layer) Deepest epidermal layer firmly attached to the dermis looks like corrugated cardboard Single row of stem cells a continually renewing cell population also called stratum germinativum because these cells undergo rapid division Journey from basal layer to surface of the skin Takes 25–45 days Layers of the Epidermis: Stratum Spinosum (Prickly Layer) Several cell layers thick Cells contain a weblike system of intermediate tension resisting prekeratin filaments attached to desmosomes (cell structures specialized for cell to cell adhesion) Keratinocytes in this layer are spiked hence the name prickly layer Abundant melanin granules (skin color) and dendritic cells (sensory) Layers of the Epidermis: Stratum Granulosum (Granular Layer) Thin; three to five cell layers in which the cells flatten Keratinization begins here-cells fill with protein- keratin) Keratohyaline (help to form keratin in the upper layers) and lamellated granules (contain a water resistant glycolypid- slow water loss in the epidermis) accumulate Layers of the Epidermis: Stratum Lucidum (Clear Layer) In thick skin Thin, transparent band superficial to the stratum granulosum A few rows of flat, dead keratinocytes with indistinct boundaries Layers of the Epidermis: Stratum Corneum (Horny Layer) 20–30 rows of dead, flat, keratinized membranous sacs Three-quarters of the epidermal thickness Functions Protects from abrasion and penetration Waterproofs Barrier against biological, chemical, and physical assaults This is layer is what makes up your dander (dry skin) and dandruff (scalp). The average person sheds 40 lbs of skin flakes in a lifetime! Stratum corneum Most superficial layer; 20–30 layers of dead cells represented only by flat membranous sacs filled with keratin. Glycolipids in extracellular space. Stratum granulosum Three to five layers of flattened cells, organelles deteriorating; cytoplasm full of lamellated granules (release lipids) and keratohyaline granules. Stratum spinosum Several layers of keratinocytes unified by desmosomes. Cells contain thick bundles of intermediate filaments made of pre-keratin. Stratum basale Deepest epidermal layer; one row of actively mitotic stem cells; some newly formed cells become part of the more superficial layers. See occasional melanocytes and epidermal dendritic cells. Desmosomes Melanin granule Melanocyte (b) Keratinocytes Dermis Sensory nerve ending Epidermal Tactile dendritic cell (Merkel) cell Figure 5.2b Dermis This is your hide- corresponds directly to animal hide that makes leather. Strong, flexible connective tissue Cells include fibroblasts, macrophages, and occasionally mast cells and white blood cells Two layers: Papillary Reticular Hair shaft Epidermis Papillary layer Dermis Reticular layer Hypodermis (superficial fascia) Nervous structures • Sensory nerve fiber • Pacinian corpuscle • Hair follicle receptor (root hair plexus) Dermal papillae Subpapillary vascular plexus Pore Appendages of skin • Eccrine sweat gland • Arrector pili muscle • Sebaceous (oil) gland • Hair follicle • Hair root Cutaneous vascular plexus Adipose tissue Figure 5.1 Layers of the Dermis: Papillary Layer Papillary layer Areolar connective tissue with collagen and elastic fibers and blood vessels The looseness of this tissue allows phagocytes and other defensive cells to wander freely as they patrol the area for bacteria that may have breached the skin. Dermal papillae contain: Capillary loops- carry blood to the dermal papillae (extensions of the dermis into the epidermis) Meissner’s corpuscles- touch receptors Free nerve endings- pain receptors Layers of the Dermis: Reticular Layer Reticular layer ~80% of the thickness of dermis Coarse irregularly arranged dense fibrous connective tissue Collagen fibers provide strength and resiliency Elastic fibers provide stretch-recoil properties Skin Markings: Friction Ridges Epidermal ridges lie atop deeper dermal papillary ridges to form friction ridges of fingerprints Friction ridges Openings of sweat gland ducts (a) Skin Markings: Cleavage Lines Collagen fibers arranged in bundles form cleavage (tension) lines Externally invisible Form separations or less dense regions Incisions made parallel to cleavage lines heal more readily Skin Color Three pigments contribute to skin color: 1. Melanin Yellow to reddish-brown to black, responsible for dark skin colors Produced in melanocytes Freckles and pigmented moles Local accumulations of melanin Skin Color 2. Carotene 3. Yellow to orange, most obvious in the palms and soles Hemoglobin Responsible for the pinkish hue of skin Homeostatic Imbalance Melanin protects your skin from sun damage but excessive sun causes clumping of elastic fibers which results in leathery skin; temporarily depresses the immune system; and can alter DNA of skin cells and lead to skin cancer. Homeostatic Imbalance Many alterations to skin color signal certain disease states and in many people emotional states: Redness or erythema: blushing, fever, hypertension, inflammation, or allergy Pallor or blanching: fear, anger, or other types of emotional stress cause a person to become pale. Pale skin may also indicate anemia or low blood pressure. Homeostatic Imbalance Jaundice or yellow cast: usually signifies a liver disorder- yellow bile pigments accumulate in the blood and are deposited in body tissues. Bronzing: A bronze almost metallic pigment to the skin is a sign of Addison’s disease in which the adrenal cortex is producing inadequate amounts of its steroid hormones. It can also be a sign of a pituitary tumor. Black and blue marks or bruises: reveal where blood escaped from the circulation and clotted beneath the skinhematoma. Appendages of the Skin Derivatives of the epidermis Sweat glands Oil glands Hairs and hair follicles Nails Sweat Glands Two main types of sweat (sudoriferous) glands 1. Eccrine (merocrine) sweat glands— abundant on palms, soles, and forehead Sweat: 99% water, NaCl, vitamin C, antibodies, dermcidin, metabolic wastes Sweat is acidic: pH of 4-6 Simple coiled tubular gland- secretory part lies coiled in the dermis and the duct extends to open in funnel shaped pore at the skin surface. Function in thermoregulation- prevent overheating of the body. Sweat pore Eccrine gland Sebaceous gland Duct Dermal connective tissue Secretory cells (b) Photomicrograph of a sectioned eccrine gland (220x) Figure 5.5b Sweat Glands 2. Apocrine sweat glands—confined to axillary and anogenital areas Approx. 2000 Larger the eccrine glands, tend to lie deeper in the dermis, and ducts empty into hair follicles Secrete sweat + fatty substances and proteins Milky or yellowish color Normally odorless until bacteria on the skin decompose organic molecule = source of body odor Functional from puberty onward (as sexual scent glands?) Sweat Glands Specialized apocrine glands Ceruminous glands Lining of the external ear canal Produce a sticky bitter substance called cerumen or earwax To deter insects and block entry of foreign material Mammary Secrete glands milk Sebaceous (Oil) Glands Widely distributed Most develop from hair follicles Become active at puberty Sebum Oily holocrine secretion Bactericidal Softens hair and skin Dermal connective tissue Sebaceous gland Sebaceous gland duct Hair in hair follicle Secretory cells (a) Photomicrograph of a sectioned sebaceous gland (220x) Sweat pore Eccrine gland Figure 5.5a Homeostatic Imbalance If a sebaceous gland is blocked by accumulated sebum a whitehead appears on the skin. If the material oxidizes and dries it darkens to form a blackhead. Acne is an active inflammation of the sebaceous glands and is usually caused by bacterial infection. Seborrhea known as cradle cap in infants is caused by overactive sebaceous glands- it begins on the scalp as pink raised lesions that gradually become yellow to brown and begin to slough off as oily scales. Hair Functions Alerting the body to presence of insects on the skin Guarding the scalp against physical trauma, heat loss, and sunlight Distribution Entire surface except palms, soles, lips, nipples, and portions of external genitalia Hair Flexible strands consist of dead keratinized cells Contains hard keratin; tougher, more durable than soft keratin of skin & individual cells do not flake off. Hair pigments: melanins (yellow, rust brown, black) combine to produce hair color from blonde to black Red haired is colored by the iron containing pigment trichosiderin Gray/white hair: results from decreased melanin production, replacement of melanin by air bubbles in the hair shaft Follicle wall Hair shaft Arrector pili Sebaceous gland Hair root • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair • Cuticle • Cortex • Medulla (a) Diagram of a cross section of a hair within its follicle Hair bulb Figure 5.6a Hair Follicle Fold down from the epidermal surface into dermis Two-layered wall: outer connective tissue root sheath (derived from the dermis), inner epithelial root sheath (derived from the epidermis) Hair bulb: expanded deep end 4mm below the skin surface Hair Follicle Hair follicle receptor (root hair plexus) Sensory nerve endings around each hair bulb Stimulated by bending a hair Feel the tickle as you run your hand over the hairs on your forearm Arrector pili Smooth muscle attached to follicle Responsible for “goose bumps” Not useful to humans Animals use it to stay warm by trapping a layer of insulating air in between their fur and also to scare off enemies Hair shaft Arrector pili Sebaceous gland Hair root Hair bulb Follicle wall • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair root • Cuticle • Cortex • Medulla Hair matrix Hair papilla Melanocyte Subcutaneous adipose tissue (c) Diagram of a longitudinal view of the expanded hair bulb of the follicle, which encloses the matrix Figure 5.6c Types of Hair Vellus—pale, fine body hair of children and adult females Terminal—coarse, long hair of eyebrows, scalp, axillary, and pubic regions (and face and neck of males) Types of Hair Hair Growth Growth and density are influenced by many factors: Nutrition Hormones The Poor nutrition means poor hair growth May enhance hair growth rate of hair growth varies with sex and age but averages around 2.5 mm a week Homeostatic Imbalance Hirsutism or excessive hairiness in women Results from an adrenal gland or ovarian tumor that secretes large amounts of androgens Hair Thinning and Baldness Alopecia—hair thinning in both sexes after age 40 Coarse terminal hairs get replaced by vellus and hair becomes very wispy True (frank) baldness Genetically determined and sex-influenced condition Recessive: on the X chromosome- female would need 2 defective X Male pattern baldness is caused by follicular response to DHT- a metabolic testosterone Growth cycles become short and many hairs don’t even emerge from their follicles Structure of a Nail Scalelike modification of the epidermis on the distal, dorsal surface of fingers and toes Functions of the Integumentary System 1. Protection—three types of barriers Chemical Low pH secretions (acid mantle) and defensins (natural antibiotics secreted by skin) delay bacterial activity Physical/mechanical barriers Keratin and glycolipids block most water and water- soluble substances Limited penetration of skin by lipidsoluble substances, plant oleoresins (e.g., poison ivy), organic solvents, salts of heavy metals, some drugs Functions of the Integumentary System Biological barriers cells -1st line of defense: activators Macrophages -2nd – dispose of viruses and bacteria that have penetrated the epidermis DNA- biological sunscreen- converts potentially destructive radiation into harmless heat. Dendritic Functions of the Integumentary System Body temperature regulation 2. Sweat glands secrete about 500 ml/day of insensible (routine & unnoticeable) perspiration (at normal body temperature) At elevated temperature, dilation of dermal vessels and increased sweat gland activity (sensible perspirations) cool the body On a hot day you can lose 12L or 3 gallons of body water Cutaneous sensations 3. Cutenous receptors are classified as exteroceptors b/c they respond to stimuli arising outside the body. Temperature, touch, and pain Functions of the Integumentary System Metabolic functions 4. The skin is a chemical factory fueled in part by the sun’s rays when sunlight hits the skin, modified cholesterol molecules are converted to a vitamin D precursor Important for calcium metabolism- calcium is not absorbed in the digestive tract without vitamin D Skin cells also make collagenase- an enzyme that aids the natural turnover of collagen and deters wrinkles. Functions of the Integumentary System Blood reservoir—up to 5% of body’s entire blood volume 5. • 6. When other body organs- such as vigorously working muscles need a greater blood supply – the nervous system constricts the blood supply in the dermal blood vessels, this pushes more blood into the general circulation making it available for other organs. Excretion—nitrogenous wastes and salt in sweat Skin Cancer 1 in 5 Americans develops skin cancer at some point. Most skin tumors are benign and do not metastasize (spread ) Some are malignant or cancerous and invade other body areas Risk factors Overexposure to UV radiation Frequent irritation of the skin Damages DNA bases and causes them to fuse. Infection, chemicals, or physical trauma There is no healthy tan but some skin lotions contain tiny oily vesicles called liposomes filled with enzymes that can fix damaged DNA before the involved cells can develop in to cancer cells. Skin Cancer Three major types: Basal cell carcinoma Least malignant, most common Relatively slow growing and mestasis seldom occurs before its noticed Stratum basale cells proliferate and invade the dermis and hypodermis Accounts for 80% of skin cancers Skin Cancer Squamous cell carcinoma Second most common Arises from the keratinocytes of the stratum spinosum Tends to grow rapidly and metastasizes if not removed Skin Cancer Melanoma Most dangerous Cancer of melanocytes Highly metastatic and resistant to chemotherapy Accounts only for 2-3% of skin cancers Most appear spontaneously but one third develops from preexisting moles and spreads to surrounding lymph and blood vessels Skin Cancer Examine your skin ABCD ruleAmerican Cancer Society: Asymmetry: two sides of the pigmented spot or mole do not match B. Border irregularity: border of lesions exhibit indentations C. Color: Pigmented spot contains several colors (blacks, browns, tans, and sometimes blues and reds) D. Diameter: The spot is larger than 6mm in diameter (the size of a pencil eraser) A. Burns Heat, electricity, radiation, certain chemicals Burn (tissue damage, denatured protein, cell death) Immediate threat: Dehydration and electrolyte imbalance, leading to renal shutdown and circulatory shock Rule of Nines Used to estimate the severity and extent of burns by measuring volume of fluid loss from burns Divides the body into 11 areas each accounting for 9% of the total body area plus an additional area surrounding the genitals that accounts for 1% of body surface area Partial-Thickness Burns Burns are classified by their depth: First degree Epidermal 1st degree burn damage only Localized redness, edema (swelling), and pain Second degree Epidermal and upper dermal damage Blisters appear 2nd degree burn (a) Skin bearing partial thickness burn (1st and 2nd degree burns) Full-Thickness Burns Third degree Entire thickness of skin damaged Gray-white, 3rd degree burn cherry red, or black No initial edema or pain (nerve endings destroyed) Skin grafting usually necessary (b) Skin bearing full thickness burn (3rd degree burn) Severity of Burns Critical if: >25% of the body has second-degree burns >10% of the body has third-degree burns Face, hands, or feet bear third-degree burns Developmental Aspects: Fetal Ectoderm epidermis Mesoderm dermis and hypodermis By the 4th month the skin is fairly well developed Lanugo coat: downy covering of delicate hairs in 5th and 6th month Vernix caseosa (varnish of cheese): when a baby is born its covered by a white cheesy looking substance produced by the sebaceous gland; protects skin of fetus within the water filled amnion Developmental Aspects: Adolescent to Adult Sebaceous gland activity increases- skin becomes oilier Skin reaches its optimal appearance in 20s-30s Effects of cumulative environmental assaults show after age 30 Abrasion, wind, sun, chemicals Scaling and dermatitis become more common Developmental Aspects: Old Age Epidermal replacement slows, skin becomes thin, dry, and itchy All of the lubricating substances produced by the skin glands that make skin supple and soft become deficient Subcutaneous fat and elasticity decrease, leading to cold intolerance and wrinkles Increased risk of cancer due to decreased numbers of melanocytes and dendritic cells