Circulation and Gas Exchange Chapter 42 (all)
advertisement

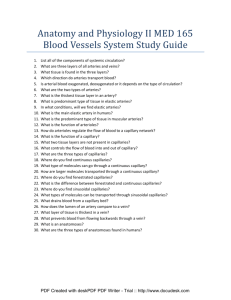
Circulation and Gas Exchange Chapter 42 (all) 4-17-06 • Overview: Trading with the Environment • Every organism must exchange materials with its environment (whether it be nutrients or gases (oxygen and carbon dioxide) – And this exchange ultimately occurs at the cellular level • In unicellular organisms – These exchanges occur directly with the environment across the cell membrane. Diffusion is adequate for necessary rapid exchange. • For most of the cells making up multicellular organisms direct exchange with the environment is not possible because diffusion distances are too great! Therefore specialized exchange and transport systems have evolved! Gills as exchange sites in aquatic animals! • The feathery gills projecting from a salmon – Are an example of a specialized exchange system found in animals Gill arch with filaments which have lamellae on both sides! Surface area of gill equal body skin surface area! Figure 42.1 • Transport systems – Functionally connect the organs of exchange with the body cells where nutrients and oxygen required! • Most complex animals have internal transport systems providing a conduit between the evironment and the cell cytoplasm! Invertebrate Circulation • The wide range of invertebrate body size and form is paralleled by a great diversity in circulatory systems. Water vascular system in star fish, open circulatory systems in insects and closed circulatory systems in earth worms and squids. Gastrovascular Cavities • Simple animals, such as cnidarians – Have a body wall only two cells thick that encloses a gastrovascular cavity (recall sea anemone sac with a mouth!) • The gastrovascular cavity – Functions in both digestion and distribution of substances throughout the body. Also gas exchange for cells lining the cavity. • Some cnidarians, such as jellies – Have elaborate gastrovascular cavities with canals radiating off the central sac! Circular canal Mouth Radial canal 5 cm Figure 42.2 Open and Closed Circulatory Systems • More complex animals – Have one of two types of circulatory systems: open or closed • Both of these types of systems have three basic components – A circulatory fluid (blood) – A set of tubes (blood vessels) – A muscular pump (the heart) Open circulatory systems • In insects, other arthropods, and most molluscs – Blood bathes the organs and tissues directly in an open circulatory system Heart Valves in heart so blood flow is unidirectional Hemolymph in sinuses surrounding ograns Anterior vessel No interstitial space or fluid! Figure 42.3a Lateral vessels Ostia Tubular heart (a) An open circulatory system Closed Circulatory System • In a closed circulatory system – Blood is confined to vessels and is distinct from the interstitial fluid Heart Closed systems are more efficient at transporting circulatory fluids to tissues and cells. Interstitial fluid Small branch vessels in each organ Dorsal vessel (main heart) Earthworm an annelid is the first time we see a closed circulatory system! Figure 42.3b Auxiliary hearts Ventral vessels (b) A closed circulatory system Survey of Vertebrate Circulation • Humans and other vertebrates have a closed circulatory system often called the cardiovascular system. • Blood flows in a closed cardiovascular system consisting of blood vessels and a two- to fourchambered heart. • Arteries carry blood from heart to capillaries – The capillaries are the sites of chemical exchange between the blood and interstitial fluid • Veins collect blood from capillaries and return blood to the heart. – Types of hearts! Vertebrate circulatory systems AMPHIBIANS REPTILES (EXCEPT BIRDS) MAMMALS AND BIRDS Lung and skin capillaries Lung capillaries Lung capillaries FISHES Gill capillaries Artery Pulmocutaneous circuit Gill circulation Heart: ventricle (V) A Atrium (A) Systemic Vein circulation Systemic capillaries Right systemic aorta Pulmonary circuit A A V Right V Left Right Systemic circuit Systemic capillaries Figure 42.4 Pulmonary circuit Left Systemic V aorta Left A Systemic capillaries A V Right A V Left Systemic circuit Systemic capillaries Fishes- two chambered heart! • A fish heart has two main chambers – One ventricle and one atrium and blood pumped from the ventricle through the gills where it is loaded with oxygen and unloadsf CO2. It then travels through the dorsal aorta to the organs and tissues thru capillary beds and is returned to the heart as venous blood. Where does heart get its oxygen? Enough remains in the venous blood. In some active species (Tuna fishes) a branch off the ventral aorta supplies oxygenated blood to the heart. Amphibians • Frogs and other amphibians have a threechambered heart, with two atria and one ventricle • The ventricle pumps blood into a forked artery that splits the ventricle’s output into the pulmocutaneous circuit (lung and skin) and the systemic circuit. Thus a certain amount of mixing of oxygenated and oxygen poor blood occures. Reptiles (Except Birds) • Reptiles have double circulation – With a pulmonary circuit (lungs) and a systemic circuit • Turtles, snakes, and lizards – Have a three-chambered heart. Mammals and Birds • In all mammals and birds – The ventricle is completely divided into separate right and left chambers • The left side of the heart pumps and receives only oxygen-rich blood – While the right side receives and pumps only oxygen-poor blood • A powerful four-chambered heart – Was an essential adaptation of the endothermic way of life characteristic of mammals and birds. Reason is because of metabolism being almost 10 times greater than the ectotherms! • A powerful four-chambered heart was an essential adaptation of the endothermic way of life characteristic of mammals and birds. Reason is because of metabolism being almost 10 times greater than the ectotherms! • Double circulation in mammals depends on the anatomy and pumping cycle of the heart (Good model). • Heart valves dictate a one-way flow of blood through the heart. • Blood begins its flow – With the right ventricle pumping blood to the lungs • In the lungs – The blood loads O2 and unloads CO2 • Oxygen-rich blood from the lungs – Enters the heart at the left atrium and is pumped to the body tissues by the left ventricle • Blood returns to the heart – Through the right atrium The mammalian cardiovascular system 7 See text for description of sequential events Capillaries of head and forelimbs Anterior vena cava Pulmonary artery Aorta Pulmonary artery 9 6 Capillaries of right lung Capillaries of left lung 2 4 3 Pulmonary vein 5 1 Right atrium 3 11 Left atrium Pulmonary vein 10 Left ventricle Right ventricle Aorta Posterior vena cava 8 Figure 42.5 Capillaries of abdominal organs and hind limbs The Mammalian Heart: A Closer Look • A closer look at the mammalian heart – Provides a better understanding of how double circulation works Pulmonary artery Aorta Pulmonary artery Anterior vena cava Left atrium Right atrium In fetus ductus artieriosus shunts blood from pulmonary artery into the aorta. Closes off at birth when the lungs inflate! Figure 42.6 Pulmonary veins Pulmonary veins Semilunar valve Semilunar valve Atrioventricular valve Atrioventricular valve Posterior vena cava Right ventricle Left ventricle • The heart contracts and relaxes – In a rhythmic cycle called the cardiac cycle • The contraction, or pumping, phase of the cycle – Is called systole • The relaxation, or filling, phase of the cycle – Is called diastole • The cardiac cycle: filling of chambers longest! 2 Atrial systole; ventricular diastole Semilunar valves closed 0.1 sec Semilunar valves open 0.3 sec 0.4 sec AV valves open 1 Atrial and ventricular diastole Figure 42.7 AV valves closed 3 Ventricular systole; atrial diastole • The heart rate, also called the pulse – Is the number of beats per minute • The cardiac output – Is the volume of blood pumped into the systemic circulation per minute and depends on the rate of contraction and the stroke volume (how much blood is “loaded” into the ventricle during diastole). Maintaining the Heart’s Rhythmic Beat • Some cardiac muscle cells are self-excitable (myogenic) – Meaning they contract without any signal from the nervous system (heart transplant). • A region of the heart called the sinoatrial (SA) node, or pacemaker sets the rate and timing at which all cardiac muscle cells contract • Impulses from the SA node spread across the atria to the atrioventricular (AV) node • At the AV node, the impulses are delayed and then travel down bundle fiber to the the Purkinje fibers that make the ventricles contract • The impulses that travel during the cardiac cycle – Can be recorded as an electrocardiogram (ECG or EKG) The control of heart rhythm • The impulses that travel during the cardiac cycle can be recorded as an electrocardiogram (EKG) 1 Pacemaker generates 2 Signals are delayed wave of signals in the atria to contract. SA node (pacemaker) 3 Signals pass at AV node. AV node to heart apex. 4 Signals spread throughout ventricles. Bundle branches Heart apex ECG Figure 42.8 Purkinje fibers • The pacemaker is influenced by – Nerves, hormones, body temperature, and exercise Blood Circulation • The same physical principles that govern the movement of water in plumbing systems – Also influence the functioning of animal circulatory systems. – Structure of circulatory system is a network of vessels that are differ in structure to accommodate function. • The velocity of blood flow varies in the circulatory system Systolic pressure Veins Venules Arterioles Capillaries Diastolic pressure Arteries 120 100 80 60 40 20 0 Aorta Area (cm2) Velocity (cm/sec) 50 40 30 20 10 0 Venae cavae Figure 42.11 5,000 4,000 3,000 2,000 1,000 0 Pressure (mm Hg) – And is slowest in the capillary beds as a result of the high resistance and large total cross-sectional area • All blood vessels – Are built of similar tissues – Have three similar layers Artery Arteries have thicker walls to accommodate the high pressure of blood pumped from the heart. Veins thinner walls. Basement membrane composed of mucopolysaccharides and collagen fibers. Not a barrier to diffusion of molecules. Vein Basement membrane Endothelium 100 µm Valve Endothelium Smooth muscle Connective tissue Endothelium Capillary Smooth muscle Connective tissue Artery Vein Venule Figure 42.9 Arteriole • In the thinner-walled veins – Blood flows back to the heart mainly as a result of muscle action Direction of blood flow in vein (toward heart) Valve (open) Skeletal muscle Valve (closed) Figure 42.10 Blood Flow Velocity • Physical laws governing the movement of fluids through pipes – Influence blood flow and blood pressure • Blood pressure – Is the hydrostatic pressure that blood exerts against the wall of a vessel • Systolic pressure – Is the pressure in the arteries during ventricular systole – Is the highest pressure in the arteries • Diastolic pressure – Is the pressure in the arteries during diastole – Is lower than systolic pressure • Blood pressure – Can be easily measured in humans 1 A typical blood pressure reading for a 20-year-old is 120/70. The units for these numbers are mm of mercury (Hg); a blood pressure of 120 is a force that can support a column of mercury 120 mm high. 4 The cuff is loosened further until the blood flows freely through the artery and the sounds below the cuff disappear. The pressure at this point is the diastolic pressure remaining in the artery when the heart is relaxed. Blood pressure reading: 120/70 Pressure in cuff above 120 Rubber cuff inflated with air 120 Pressure in cuff below 120 Pressure in cuff below 70 120 70 Sounds audible in stethoscope Artery Artery closed 2 A sphygmomanometer, an inflatable cuff attached to a pressure gauge, measures blood pressure in an artery. The cuff is wrapped around the upper arm and inflated until the pressure closes the artery, so that no blood flows past the cuff. When this occurs, the pressure exerted by the cuff exceeds the pressure in the artery. Figure 42.12 3 A stethoscope is used to listen for sounds of blood flow below the cuff. If the artery is closed, there is no pulse below the cuff. The cuff is gradually deflated until blood begins to flow into the forearm, and sounds from blood pulsing into the artery below the cuff can be heard with the stethoscope. This occurs when the blood pressure is greater than the pressure exerted by the cuff. The pressure at this point is the systolic pressure. Sounds stop • Blood pressure is determined partly by cardiac output – And partly by peripheral resistance due to variable constriction of the arterioles (anaphylactic shock). – For high blood pressure try and reduce peripheral resistance using smooth muscle relaxants! Capillary Function • Capillaries in major organs are usually filled to capacity – But in many other sites, the blood supply varies. Homeostatic mechanisms involved to keep blood pressure constant! Control of Blood Flow Through Capillaries • Two mechanisms – Regulate the distribution of blood in capillary beds • In one mechanism – Contraction of the smooth muscle layer in the wall of an arteriole constricts the vessel • In a second mechanism – Precapillary sphincters control the flow of blood between arterioles and venules Precapillary sphincters Thoroughfare channel (a) Sphincters relaxed Arteriole Venule Capillaries Arteriole Venule (b) Sphincters contracted (c) Capillaries and larger vessels (SEM) Figure 42.13 a–c 20 m • The critical exchange of substances between the blood and interstitial fluid – Takes place across the thin endothelial walls of the capillaries • The difference between blood pressure and osmotic pressure – Drives fluids out of capillaries at the arteriole end and into capillaries at the venule end Tissue cell Capillary Capillary Red blood cell INTERSTITIAL FLUID Net fluid movement out Net fluid movement in 15 m Direction of blood flow Pressure At the arterial end of a capillary, blood pressure is greater than osmotic pressure, and fluid flows out of the capillary into the interstitial fluid. At the venule end of a capillary, blood pressure is less than osmotic pressure, and fluid flows from the interstitial fluid into the capillary. Blood pressure Osmotic pressure Inward flow Outward flow Figure 42.14 Arterial end of capillary Venule end Osmotic pressure in capillary due to plasma proteins! Fluid Return by the Lymphatic System • The lymphatic system – Returns fluid to the body from the capillary beds – Aids in body defense because it passes through lymph nodes where white blood cells take out any pathogens or foreign material! • Fluid reenters the circulation – Directly at the venous end of the capillary bed and indirectly through the lymphatic system Blood • The cellular elements of mammalian blood Cellular elements 45% Cell type Separated blood elements Number per L (mm3) of blood Functions Erythrocytes (red blood cells) 5–6 million Transport oxygen and help transport carbon dioxide Leukocytes (white blood cells) 5,000–10,000 Defense and immunity Lymphocyte Basophil Eosinophil Neutrophil Monocyte Platelets Figure 42.15 250,000 400,000 Blood clotting Plasma • Blood plasma is about 90% water • Among its many solutes are – Inorganic salts in the form of dissolved ions, sometimes referred to as electrolytes • The composition of mammalian plasma Plasma 55% Constituent Major functions Water Solvent for carrying other substances (blood electrolytes) Sodium Potassium Calcium Magnesium Chloride Bicarbonate Plasma proteins Albumin Fibringen Immunoglobulins (antibodies) Osmotic balance pH buffering, and regulation of membrane permeability Separated blood elements Osmotic balance, pH buffering Clotting Defense Substances transported by blood Nutrients (such as glucose, fatty acids, vitamins) Waste products of metabolism Respiratory gases (O2 and CO2) Hormones Figure 42.15 Erythrocytes • Red blood cells, or erythrocytes – Are by far the most numerous blood cells – Transport oxygen throughout the body – Platelets function in blood clotting Blood Clotting • A cascade of complex reactions – Converts fibrinogen to fibrin, forming a clot 1 The clotting process begins when the endothelium of a vessel is damaged, exposing connective tissue in the vessel wall to blood. Platelets adhere to collagen fibers in the connective tissue and release a substance that makes nearby platelets sticky. 2 The platelets form a plug that provides emergency protection against blood loss. 3 This seal is reinforced by a clot of fibrin when vessel damage is severe. Fibrin is formed via a multistep process: Clotting factors released from the clumped platelets or damaged cells mix with clotting factors in the plasma, forming an activation cascade that converts a plasma protein called prothrombin to its active form, thrombin. Thrombin itself is an enzyme that catalyzes the final step of the clotting process, the conversion of fibrinogen to fibrin. The threads of fibrin become interwoven into a patch (see colorized SEM). A baby aspirin per day makes the platelets lazy! Collagen fibers Platelet plug Platelet releases chemicals that make nearby platelets sticky Fibrin clot Red blood cell Clotting factors from: Platelets Damaged cells Plasma (factors include calcium, vitamin K) Prothrombin Figure 42.17 Thrombin Fibrinogen Fibrin 5 µm Hemophiliacs