PrEP Promotion: A Washington State Overview
advertisement

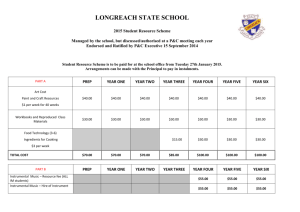
State Health Departments Implementing PrEP PrEP Promotion: A Washington State Overview Dave Kern Dave Kern Manager, Manager, Infectious Disease Prevention HIV and Adult Viral Hepatitis Prevention Services Washington April 15,State 2015Department of Public Health WASHINGTON STATE OVERVIEW • Population • 6.8 million (2011 estimate) • New HIV diagnoses • ~510 new cases / year • Prevalent HIV cases • 12,000+ persons living with HIV disease • Concentration of disease • Central Puget Sound (including Seattle) – 77 percent of new diagnoses • Trends • Decreasing diagnoses and rates WHAT WE KNOW • Our epidemic is concentrated geographically and within specific populations – gay / bisexual men in the Puget Sound. • New HIV diagnoses and rates of HIV infection are declining. • Coverage and saturation of HIV testing / screening is good – nearly 90 percent of persons living with HIV know their status. • Viral suppression in the population of persons living with HIV is good – nearly 60 percent are suppressed. • To achieve the impact we want – a 50 percent reduction in the rate of new HIV diagnoses by 2020 – we must continue to improve work along the HIV care continuum and, at the same time, improve efforts to prevent transmission to HIV-negative persons. WHERE DID WE START? • In partnership with our state’s HIV Prevention Planning Group (20112013), we mapped outcomes that influence direct transmission of HIV. Priority outcomes include: – Suppressed viral load among persons living with HIV – Decreased STD incidence (GC and syphilis) – Increased use of PrEP – Increased use of nPEP – Increased use of condoms – Increased use of clean syringes • OUTCOME THREE: Increase use of pre-exposure prophylaxis (PrEP) among gay and bisexual men in Seattle and secondary urban areas Secondary urban areas = Everett, Kent, Renton, Shoreline, Spokane, Tacoma and Vancouver WHERE DID WE START? • Our planning group recommended PrEP be a priority outcome for gay and bisexual men in urban areas. • Though supportive, the planning group expressed reservations about PrEP, citing common concerns: misuse, unintended consequences, moral objection to providing ART to HIV-negative persons while ART is not available for all HIV-positive persons, etc. • The planning group’s recommendation came after many months of discussion and as a result of their commitment to meaningfully reducing HIV transmission. • Work with this community body was an important first step in our process. WHERE ARE WE NOW? • Based on planning group recommendations, all current HIV programming connects to one or more of the 6 outcomes. • Our PrEP promotion approach includes activities aimed at increasing awareness, access and uptake of PrEP, primarily among gay / bisexual men. • Our approach is multi-faceted – community, public health, healthcare and payers. • 2014 focused on infrastructure and capacity building. WHERE ARE WE NOW? • Community engagement – Community mobilization – Community forums – Health insurance outreach and enrollment increase access to and utilization of healthcare among gay / bisexual men • Public health engagement – DIS refer to PrEP all gay / bisexual men diagnosed with syphilis and / or rectal GC (data are monitored – who’s eligible, who’s offered, who accepts, etc.) – Local health departments instituted local PrEP referral processes – DOH provided training to all funded DIS and medical case management staff WHERE ARE WE NOW? • Healthcare engagement – Identify and publicize local clinicians willing to prescribe and manage PrEP – Hosted informal dinners for Seattle-based LGBT and ID providers – Provided funding to Seattle-based doc to support PrEP program at Gay City Health Project WHERE ARE WE NOW? • Healthcare engagement (continued) – Established PrEP clinic at Seattle STD clinic • Highly targeted for gay / bisexual men with syphilis and / or rectal GC • Funding covers medical, lab and drug costs • In the future, will explore uptake and maintenance strategies (e.g., shift longer term users to PCPs?) – Provide information and non-fiscal support to other healthcare systems (e.g., guidelines, mentors) WHERE ARE WE NOW? • Payer system engagement – PrEP DAP – Medicaid / QHP enrollment of eligible persons – Purchased insurance (premium payment assistance) for participants without coverage (during open enrollment) WHERE ARE WE NOW? • PrEP DAP – Launched April 2014 – Drug assistance program to reduce barriers associated with costs of Truvada – Currently, coverage is for Truvada only, not medical or lab costs – Coverage for both co- and full-pay, depending on needs of the enrollee – Not meant to replace individual’s medical home, but to defray deductible and co-pay costs of medication – To date, soft-touch launch of program • Emails to providers (clinical, prevention and non-clinical care) • Web presence • Media WHERE ARE WE NOW? • PrEP DAP – Eligibility criteria are fairly low threshold to not curtail early interest in the program • Risk – sero-discordant couples, gay / bisexual men who meet certain risk criteria • Residence – WA State only • Healthcare provider engagement – Provider must complete part of the application • No income or requirement to use PAP • No requirements for routine medical visits (though strongly encouraged) WHERE ARE WE NOW? • PrEP DAP – Created and launched as a matter of program planning and development, rather than a legislative or agency initiative – Collaborative effort between DOH HIV prevention and HIV care / treatment programs – Built on the backbone of state’s ADAP program – eligibility processing and pharmacy benefits management – Funded exclusively with state general funds • CDC, Part B / ADAP dollars and rebate dollars cannot be used (but do free up state funds to support PrEP DAP) WHERE ARE WE NOW? • PrEP DAP – ~$2M / year allocated for coverage of ~200 clients • Conservative estimate figuring 50 percent of enrollees will be full pay (WRONG!) – System improvements and / or changes will be made as appropriate – Staffing: • 11 DOH staff tasked with some portion of PrEP DAP / promotion – 6 prevention staff – ~1.85 FTE – 4 care staff – ~0.65 FTE – 2 surveillance staff – ~0.10 FTE WHERE ARE WE NOW? 332 Applications Received 273 Active PrEP DAP Clients 41 Denied 18 Incomplete Applications Gender: • 7 are female (<3%) • 264 are male (97%) • 1 is other gender (<1%) • 1 is Transgender (FtM) (<1%) Ethnicity: • 197 Non-Hispanic/Latino(a) (72%) • 39 Hispanic/Latino(a) (15%) • 37 No Answer (13%) Race: Insurance Status: • 42 are uninsured (15%) • 231 are insured (85%) • 1 Alaskan Native/American Indian (<1%) • 1 Native Hawaiian/Pacific Islander (<1%) • 7 Other (2.5%) • 7 Black/African American (2.5%) • 13 Asian (4.8%) • 15 Multi Race (5.5%) • 18 No Answer (6.6%) • 211 White/Caucasian (77.3%) WHERE ARE WE NOW? • PrEP DAP: Risk Factors (client declared) – 27% have sexual / drug sharing partner(s) who is HIV+ – 80% identify as gay / bisexual man or other man who engages in sexual activity and has one or more of the following conditions: • 26% - Bacterial STI within the last year • 26% - Exposure to an STI within the last year • 64% - Ten or more partners within the last year • 3% - Used meth within the last year • 46% - Unprotected anal intercourse with partner of unknown hiv-1 status Month/Yr Clients Clients Active Filling 4/2014 5 3 5/2014 11 6 6/2014 14 8 7/2014 24 11 8/2014 41 32 9/2014 64 43 10/2014 91 59 11/2014 109 56 12/2014 148 91 1/2015 188 144 2/2015 241 163 3/2015** 273 91 WHERE ARE WE NOW? Costs* as of 3/15/2015 Drugs Contractor set up costs TOTAL *no DOH Staff costs included **as of 3/15/2015 $414,052.48 $ 20,660 $434,712.48 WHERE ARE WE GOING? • In 2015, we plan to: – Align existing and future PrEP promotion efforts with End AIDS Washington WHERE ARE WE GOING? • In 2015, we plan to: – Add multi-jurisdiction marketing / media PrEP promotion campaign for communities and providers – Add navigation / care coordination for PrEP users – Work with local AETC to increase provider awareness, knowledge and support for PrEP via HIV ECHO (telemedicine) – Develop data collection system to monitor PrEP utilization (e.g., accessing and analyzing Medicaid and health plan data) – Cultivate new partnerships with pharmacies to increase accessibility of PrEP – Explore options for covering medical / lab costs for PrEP DAP participants WHERE ARE WE GOING? • In 2015, we plan to: – Expand GCHP PrEP project to: • Provide a PrEP “start up” clinic for individuals without insurance and / or primary care providers • Identify and cultivate other clinician champions • Identify and market GCHP PrEP “start up” clinic to providers who are willing to assume PrEP management after initial monitoring • Work with participants to enroll them in insurance and primary care • Streamline the GCHP PrEP process to leverage other resources LESSONS LEARNED / FINAL THOUGHTS • PrEP isn’t a new and novel intervention anymore. It’s an essential tool in the tool box. PH must find opportunities to promote its use. • The collaboration between health department prevention and care / treatment programs was integral to our success. • A multi-faced approach allowed us to promote PrEP on multiple fronts (community, public health, healthcare and payer engagement). • We opted to integrate PrEP into the work of as many staff and programs as possible rather than consolidating it into one team, i.e., PrEP as a tool, not a program area. • We remain curious and open to discovery. CONTACT INFORMATION Dave Kern, Manager Infectious Disease Prevention david.kern@doh.wa.gov Richard Aleshire, Manager HIV Client Services richard.aleshire@doh.wa.gov. Beth Crutsinger-Perry, ADAP HIV Client Services elizabeth.Crutsinger-Perry@doh.wa.gov